1. Introduction
The number of report cases of sinonasal organized hematoma has dramatically increased during the recent five years. The reasons for its increase include. First, the diagnostic rate was increased as clinical features and characteristic imaging findings are somewhat elucidated. Second, the specific pathologic findings suggesting organized hematoma might help to increase the incidence of reports (1-3). Besides one case involving the sphenoid sinus, all reported cases affected the maxillary sinus, presenting as an expansile and soft tissue mass with or without spreading to the nasal cavity (4).
We report computed tomography (CT) findings of a case of giant organized hematoma originating from the inferior turbinate without any paranasal sinuses involvement with an emphasis on different patterns of enhancement of the tumor on enhanced CT scans. To our knowledge, this is the first case report in English literature reporting organized hematoma originating from the inferior turbinate.
2. Case Presentation
A previously healthy 40-year-old man presented with a one-month history of right-sided nasal obstruction. He also complained of frequent nasal bleeding and right-sided ear fullness. He had no significant medical problem including facial trauma, bleeding tendency, allergy or sinus surgery. Because anterior rhinoscopic examination demonstrated a large reddish mass totally occupying the right nasal cavity, it was not possible to examine the right nasal cavity by endoscopy. The retrovelar nasopharyngoscopy revealed filling of the right posterior choana (Figure 1). This mass tended to bleed easily with touching by suction tip. Preoperative pathologic evaluation of the specimen demonstrated only vascular fibrous tissue with chronic inflammation, but the pathologist was not able to confirm the exact pathologic diagnosis. CT examination of the paranasal sinuses and nasal cavity was performed on a multidetector-row CT scanner (LightSpeed Plus; GE Healthcare, Waukesha, WI). The enhanced scans were obtained immediately after intravenous administration of 100 mL contrast media (Iopromide, Ultravist 300; Schering, Seoul, Republic of Korea) at a rate of 1.8 mL/s. The precontrast axial CT examination revealed a large soft-tissue mass in the right nasal cavity extended to the choana. Unenhanced axial (Figure 2) and contrast-enhanced axial and coronal (Figure 3) CT scans showed a soft tissue mass with heterogeneous patchy enhancement and opacification of the maxillary and ethmoid sinuses because of the mass obstructing the draining sinus ostia. Moreover, the nasal cavity extension was evident with bowing of posterior septum to the left side and the inferior turbinate was very thin, upwardly displaced and compressed. However, there was no loss of bony contour of medial wall of the maxillary sinus and ethmoid sinus.
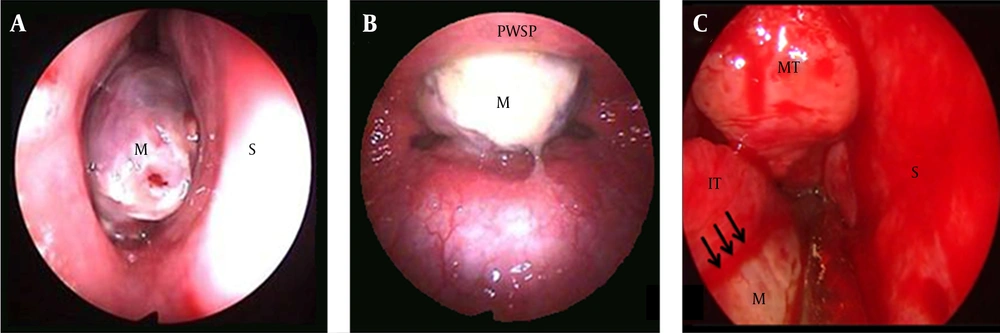
A 40-year-old man with nasal obstruction, frequent nasal bleeding and right-sided ear fullness. A, Preoperative endoscopic findings showing a reddish polypoid mass occupying right nasal cavity; it was easily bled and nasal passage was completely obstructed. B, preoperative retrovelar nasopharyngoscopic view showing a mass extended to the choana. C, after partial removal of the mass, we verified the mass was attached to anterosuperior portion (black arrows) of the inferior turbinate. (M: mass, S: Septum, MT: middle turbinate, IT: inferior turbinate, PWSP: posterior wall of soft palate).
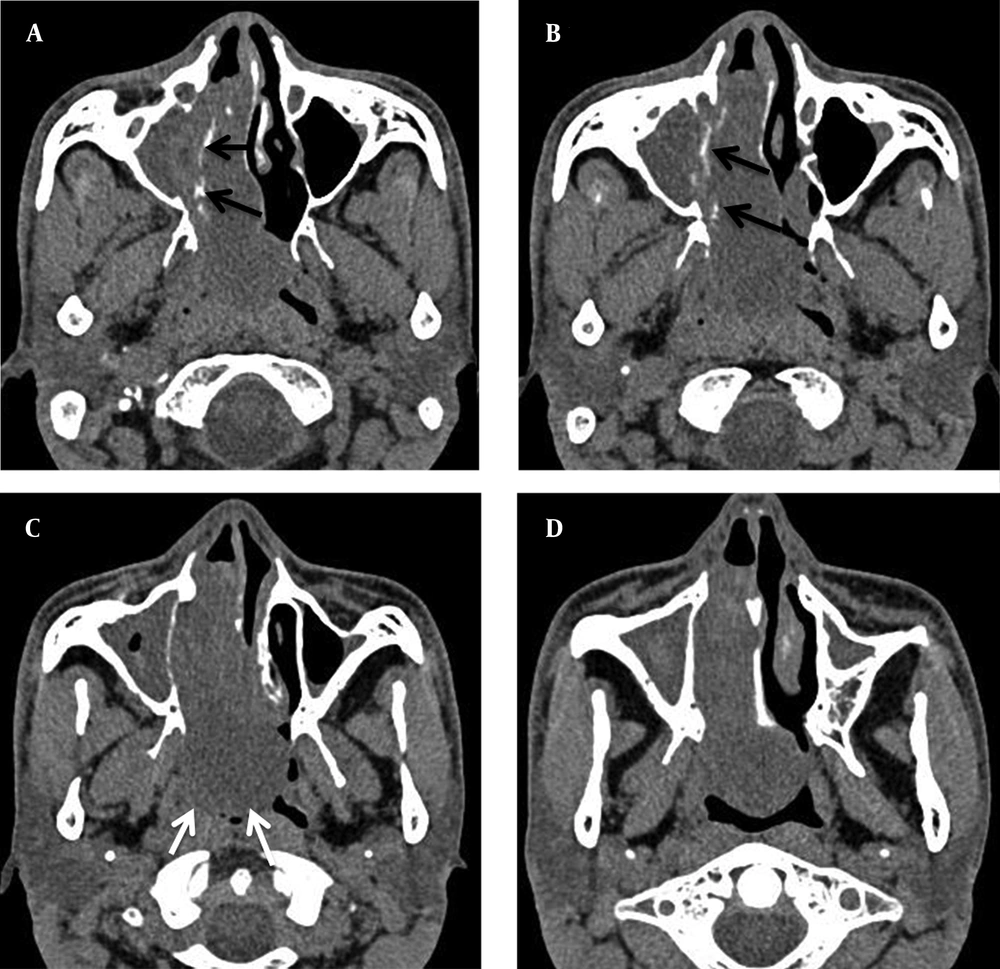
A-D, Preoperative axial CT scans without contrast-enhancement of the paranasal sinus show a well-defined huge soft tissue mass from anterior choana extended to nasopharynx and opacification of right maxillary sinus, secondary accumulation of secretions (black arrows: inferior turbinate, white arrows: posterior margin).
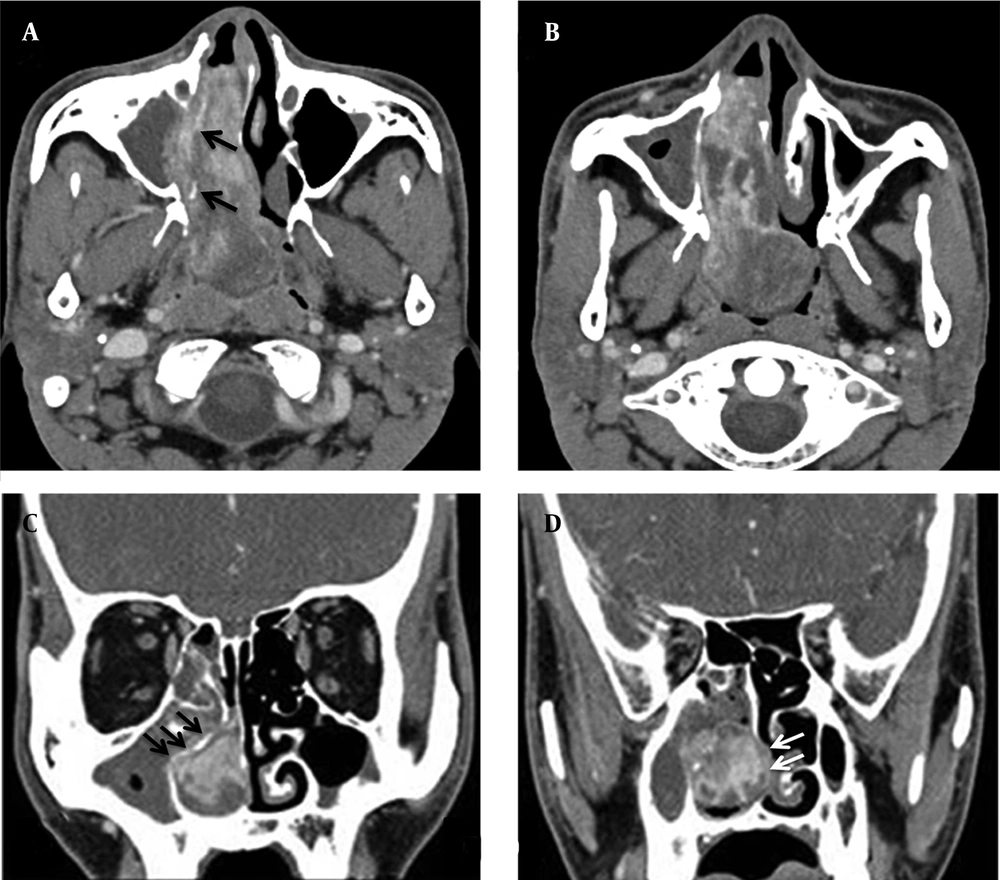
Contrast-enhanced CT scans showing a huge soft tissue mass with heterogeneous patchy enhancement and opacification (secondary accumulation of secretions) of the maxillary and ethmoid sinuses. Also, the inferior turbinate (black arrows) was very thin, upwardly displaced and compressed. The nasal cavity extension is evident with bowing of posterior septum (white arrows) to the left side (A, B: axial view, C, D: coronal view).
Although the mass was friable and easily broken, complete resection of the mass was achieved by trans-nasal endoscopic surgery and bleeding was controlled with a coagulation-suction device. The precise origin site of this mass was anterior portion of the inferior turbinate. The inferior turbinate was very thin, upwardly displaced and compressed. Histopathological finding was consistent with organized hematoma (Figure 4). The patient had a satisfactory postoperative course. There was no recurrence of lesion at 12 months follow-up.
3. Discussion
Organized hematoma is believed to develop initially from the accumulation of blood resulting from various causes, such as trauma, surgery, bleeding diatheses, hemorrhagic lesion within the sinus and loss of mechanical integrity of an arterial branch (3). Because the maxillary sinus is the largest paranasal sinus that allows conditions of negative pressure, significant leakage of blood could happen from the nasal cavity into the sinus through ostium (5). Therefore, organized hematoma occurs most frequently in the maxillary sinus and is known as organized hematoma of maxillary sinus (OHMS) (6). In our case, organized hematoma originated from the inferior turbinate without inclusion of paranasal sinuses. Because there is no cavity with negative pressure for blood accumulation in nasal lumen, we think that the pathophysiology for our case was different from OHMS mentioned above. Therefore, further case studies are needed.
Similar to major symptoms of OHMS (6), our patient complained of frequent nasal bleeding and nasal obstruction. However, because the patient presented with a 1-month history of nasal obstruction developing abruptly, we could suppose that it had grown very fast. rate. Probably, because there were no restrictions in nasal cavity from anterior nares to choana, it shows rapidly expansile character. Therefore, in cases of organized hematoma of the nasal cavity, it can be diagnosed at early stages due to early nasal symptoms compared to OHMS.
The reported CT findings of organized hematoma include an expansive, clearly demarcated and compressive mass causing bony erosion but never destructive (1). After administration of contrast, heterogeneous enhancement in a patchy distribution is usually found within the lesion (2). There is no significant difference between OHMS and the present case in CT findings except for uncommon origin site. In our case, CT scans showed a full-filling soft tissue mass with heterogeneous patchy enhancement in the nasal cavity and opacification of maxillary and ethmoid sinuses without loss of bony contour of sinus wall. Moreover, nasal cavity expansion was evident with bowing of posterior septum to the left side and the inferior turbinate was very thin, upwardly displaced and compressed. Those findings were suggestive of organized hematoma originating from the nasal cavity. MR imaging is superior to CT for determining the margin and extent of lesion. In MR images, the heterogeneous signal intensity reflects the various components contained within the lesion, such as hemorrhage, fibrosis and vascular proliferation. It has biphasic appearance that central part of the lesion presents low intensity on T1-weighted images and high intensity on T2-weighted images, corresponded with hematoma and peripheral part is less enhanced with zone of fibrosis (1). In addition, on T2-weighted MRI, a conspicuous “shell” of T2 dropout surrounded the lobules of each mass. These shells were part of the soft tissue mass and were not dead space in the sinus (7). However, there is no report on MRI in case of organized hematoma restricted to nasal cavity. Because enhanced CT showed typical findings of organized hematoma except for the lesion located in the nasal cavity rather than the paranasal sinus, we suspected the organized hematoma originated from the nasal cavity as preoperative diagnosis based on endoscopic and imaging findings.
Recently, according to the development of endoscopic sinus surgery, it is possible to completely remove the lesion without excessive surgical invasion in the treatment of sinonasal organized hematoma (4). In cases where adequate endoscopic operative field is not achieved for the lesion such as in our case, endoscopic sinus surgery with the assistance of a microdebrider should be chosen for complete removal. In addition, during the operation, we could verify the precise origin site of this mass as anterior portion of the inferior turbinate, but it had not extended into the sinus.
The specific pathologic findings suggesting organized hematoma might help to increase the incidence of reports. Histologically, combination of three findings of fibrous tissue, neovascularization and extravasated red blood cells in the subepithelium with no evidence of malignancy is characteristic to confirm organized hematoma (6). Although there is no serious complication reported, preoperative biopsy is consistently nondiagnostic and does not provide helpful information in differentiating more worrisome neoplastic processes (7).
The nasal cavity may be involved in a wide variety of hypervascular lesions, either benign or malignant and differential diagnosis may be challenging. A differential diagnosis of a hypervascularized mass of the nasal cavity in patients with nasal obstruction and/or epistaxis might include juvenile angiofibroma, angiofibromatous polyp, hemangioma (lobular or capillary), hemangiopericytoma, paraganglioma, angiosarcoma and hypervascular metastasis, particularly from kidney, thyroid, lung or breast (8).
The most important disease that should be differentiated with organized hematoma of the nasal cavity is lobular capillary hemangioma (LCH). The reasons are as follows. First, both may rarely present as a mass of considerable size and thus entire filling of the nasal cavity. Second, both accompany clinical manifestations such as nasal obstruction and recurrent epistaxis and both may be seen as a red to purple single hypervascularized mass on endoscopic findings. Third, surgery is the treatment of choice for both and radical resection can be performed through an endoscopic approach even in large lesions. Finally, microtrauma from nasal packing and intubation is one of the most common predisposing factors for LCH (9), and in cases of organized hematoma, history of trauma is an important factor. However, unlike organized hematoma of the nasal cavity, LCH is well-circumscribed and intensely enhanced with no internal calcification or phleboliths on contrast-enhanced CT scan. Furthermore, MR images result in low signal intensity T1-weighted images and very high signal intensity on T2-weighted image (10).
In conclusion, we reported CT findings of a case of huge organized hematoma of the nasal cavity originating from the inferior turbinate, which completely obstructed the right nasal cavity and the nasopharynx without any involvement of sinus, with an emphasis on different patterns of enhancement of the tumor on the enhanced CT scans. This case was exceptional because of unusual location and difficulties in diagnosis. Therefore, organized hematoma in nasal cavity alone is a rare lesion of unknown etiology, which should be considered in the differential diagnosis of rapidly enlarging vascular lesions within the nasal cavity.