1. Background
The meticulous cleaning, shaping, and filling of the root canal systems are the primary aims of root canal treatment (1). The maxillary first molar tooth has one of the most complex root and canal anatomies (2, 3). Countless studies and discussions have been based on the existence of a second canal in the mesiobuccal (MB) root of the maxillary molars (4, 5), since it is strongly believed that one of the foremost reasons for endodontic failure in maxillary first molars is the difficulty of detecting and treating those second mesiobuccal (MB2) canals (2).
Several techniques have been used to detect MB2 canals in maxillary molars in both in vitro and clinical studies, including operating microscopes (6-11), ultrasounds (12), the use of a bur and explorer (10, 13), and conventional or advanced radiographic techniques (14-18). Such approaches are commonly used to facilitate the detection of MB2 canals (10, 19, 20); however, the abovementioned methods cannot reliably detect MB2 canals (15). The literature reveals that although MB2 canals of maxillary first molars have been found in more than 70% of in vitro studies (5, 7, 21, 22), they were detected clinically in less than 40% of cases (2, 23-25). Cone beam computed tomography (CBCT) is a new technology in the field of endodontics that has several advantages, including the ability to perform three-dimensional (3D) imaging of root canal systems with lower radiation doses, higher resolution, and no superimposition (26-28). Therefore, CBCT could be useful for several common endodontic fields, including endodontic surgery, dental trauma, internal or external root resorption, diagnosis of apical pathosis, and evaluation of the complex root canal configuration (29-32).
2. Objectives
Researchers have evaluated the efficiency of CBCT when it comes to identifying MB2 canals, and CBCT has been suggested to be a reliable method for the detection of these canals (4), while other authors have considered the localization of MB2 canals using CBCT scans (14). However, few studies with sufficient and satisfactory findings regarding the localization of MB2 canals using CBCT could be found in the literature. Therefore, the aim of the present in vitro study is to develop a new approach for localizing MB2 canals in the maxillary first molars using CBCT. This method could facilitate the detection of MB2 canals in clinical practice.
3. Patients and Methods
This retrospective study included CBCT data from patients who were referred to the department of dentomaxillofacial radiology, faculty of dentistry, Gaziantep, Turkey, from 2011 to 2014. The CBCT data were recorded for several reasons, including implant surgery, pathological reasons, or orthodontic treatment. A total of 468 maxillary first molars were investigated from 296 patients (155 males and 141 females) with a mean age of 24.42 (±11.29) years (range 7 - 68 years).
Maxillary first molar teeth with no caries or defects, filled materials, periapical lesions, root canal treatments, or root canals with open apices, resorption, or calcification were evaluated to prove that reliable, good quality CBCT images were available. Any cases of the abovementioned conditions were excluded from the study since they may adversely affect the image quality. All of the CBCT images were obtained using the same scanner (Planmeca, Promax, Helsinki, Finland). Axial, sagittal, and coronal sections were imaged, and the images were analyzed using special CBCT software (Romexis, Planmeca, Helsinki, Finland). The study was approved by the local ethics committee of the university of Gaziantep.
All of the images from 296 maxillary molar teeth were evaluated on the axial section. Using the axial section as a guide allowed the accurate localization of the designated parameters without superimposition in different planes. Thus, the reproducibility of the measurements was ensured by the use of such standardization (33). The first axial section where the angles formed by the canal orifices were seen from the axial plane was used to determine the angles used in the present study. In fact, there was no final decision on this matter in the literature. The following parameters were recorded: the presence of MB2 canals; the angle formed by the mesiobuccal, distobuccal, and palatal root canal orifices (∠MDP); and the angle formed by the mesiobuccal, distobuccal, and MB2 canal orifices (∠MDMB2). The presence of MB2 was analyzed according to age, gender, and side (right or left) where the MB2 canals were identified. In addition, the ∠MDP and the ∠MDMB2 were analyzed and evaluated.
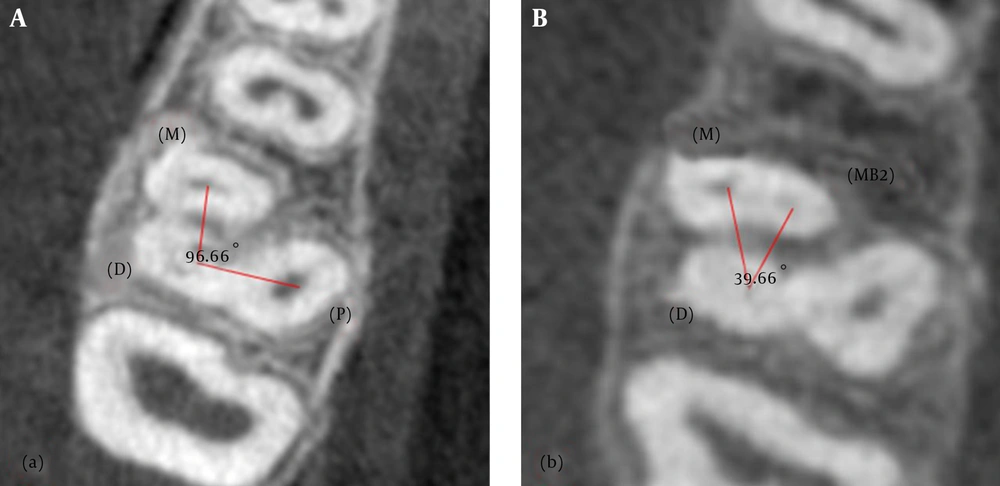
All of the measurements and analyses were performed twice by one dentomaxillofacial radiologist (AMA) and one experienced endodontist (EK), with a two-week interval between the assessments. If there was any disagreement in the results, they were discussed and a final decision was made. All data were obtained after the final calibration. A consensus was reached between the radiologist and the endodontist as to how many canals were present in the MB root of the tooth in question, as well as to how the ∠MDP and ∠MDMB2 angles were measured on the CBCT scans (Figure 1). The observations were carried out under dimmed lighting and against a black background. The images were viewed on a 24 inch ultrasharp LED TFT monitor (Dell, USA) that displayed 2 megapixels, with a 0.27 pixel pitch.
To compare the two groups, Student’s t-test (for continuous variables), the chi-squared test (for categorical variables), and Pearson correlation (for two numerical variables) were used. Next, a multiple linear regression model was employed for the predictions. The intra- and inter-observer agreements were calculated using the interclass correlation coefficient (ICC). Means and standard deviations were given as descriptive statistics. All analyses were performed using SPSS for Windows version 22.0 (IBM Corp. Released 2013. IBM SPSS Statistics for Windows, Version 22.0. Armonk, NY: IBM Corp.). A two-sided P value < 0.05 was considered as statistically significant.
4. Results
Data were obtained from 728 patients, and 468 maxillary first molar teeth in 296 subjects (155 males and 141 females) were investigated in this retrospective CBCT-based study. The age range of the subjects was 7 to 68 years, while the mean age was 24.42 years (±11.29). Of the 468 first molars, 205 MB2 canals were observed. Of those, 103 MB2 canals were in males and 102 were in females. The incidence of MB2 canals was found to be 43.80%. There were no statistically significant differences according to the gender of the patients (P= 0.300) (Table 1). The ICC scores of the observers, AMA and EK, were found to be 0.862 and 0.901 for the intra-observer agreements, and the ICC was also found to be 0.759 for the inter-observer agreement.
| Presence or Absence | Females (%) | Males (%) | Total (%) | |
|---|---|---|---|---|
| Subjects | MB2 Presencea | 131 (62.68) | 78 (37.32) | 209 (100.00) |
| MB2 Absence | 95 (55.23) | 77 (44.77) | 172 (100.00) | |
| Total | 141 (47.64) | 155 (52.36) | 296 (100.00) | |
| Teeth | MB2 Presence | 102 (49.76) | 103 (50.24) | 205 (100.00) |
| MB2Absence | 124 (47.15) | 139 (52.85) | 263 (100.00) | |
| Total | 226 (48.3) | 242 (51.7) | 468 (100.00) | |
| P value | 0.300 | |||
Abbreviation: MB2, second mesiobuccal canal.
aMB2 was found on at least one side.
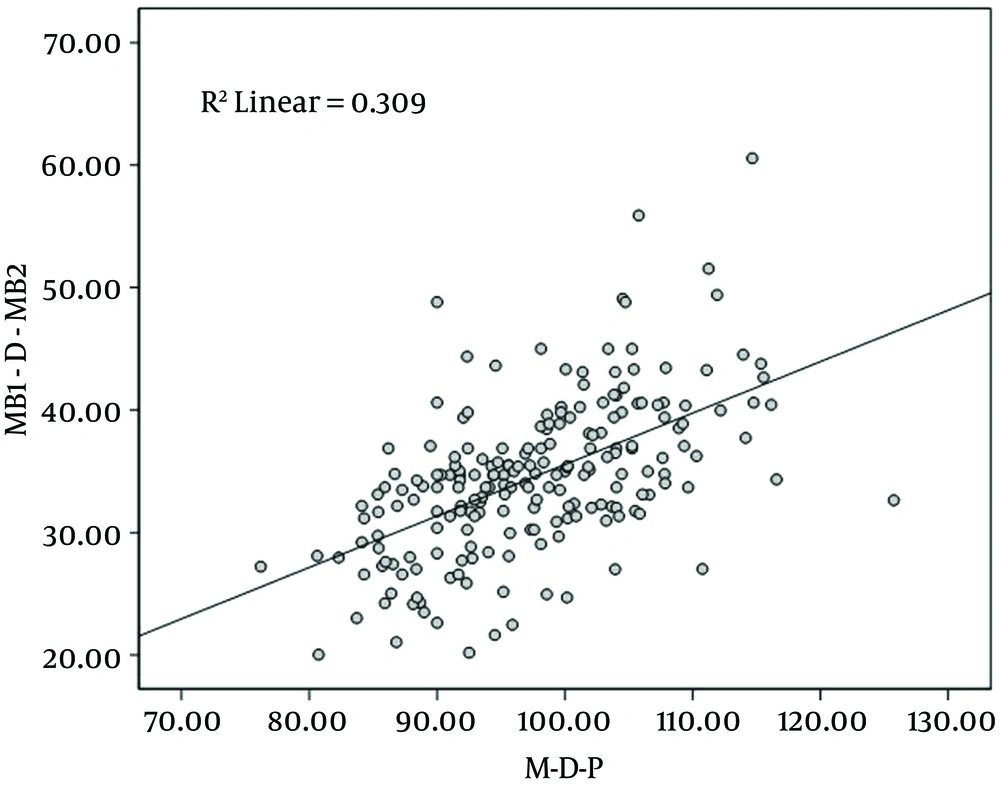
The ∠MDP and the ∠MDMB2 were also detected and evaluated in the current study. The maxillary first molar teeth with MB2 canals had a statistically significant higher ∠MDP than the teeth without MB2 canals (Table 2). A moderately positive correlation was found between the ∠MDP and the ∠MDMB2 (Figure 2). To predict the ∠MDMB2 values in the multiple regression model, it was shown that the ∠MDMB2 increased by 0.420 degrees when the ∠MDP increased by 1 degree (Figure 2), and this could be formulated as Y∠MDMB2 = 0.420×∠MDP (r2 = 0.309).
| N | ∠MDP, Mean, Degree | Std. Deviation | P | r | |
|---|---|---|---|---|---|
| MB2 Absence | 262 | 93.8606 | 11.29781 | 0.001 | 0.556 |
| MB2 Presence | 205 | 97.6326 | 8.37563 |
Abbreviation: MB2, second mesiobuccal canal.
5. Discussion
One of the most important factors that leads to the failure of root canal therapy is the inability to effectively treat all canals in the root canal system (4). Failure to find and obturate the MB2 canals in permanent maxillary first molars has been proven to pose the greatest challenge to adequate endodontic treatment, and it will likely result in the failure of the treatment as a whole (9, 34). In fact, the evidence to date suggests that more MB2 canals are found in laboratory studies (approximately 70%) than in clinical practice (approximately 40%) (35), although microsurgical instruments such as magnifying loupes and dental operating microscopes are commonly used to increase the detection rate of MB2 canals in clinical situations (9). Three-dimensional imaging of teeth with MB2 canals prior to endodontic treatment may help to increase the success rate of root canal therapy. While micro-CT facilitates endodontic studies in the laboratory (36), CBCT scans may be useful in clinical settings due to advantages such as lower radiation dose (37-39), higher resolution (39), and isotropic voxels (40). In a pilot study, Blattner et al. (4) assessed CBCT scans’ ability to accurately confirm or disconfirm the existence of MB2 canals in maxillary first molars. They found that CBCT scanning is a reliable method of detecting MB2 canals. In light of these studies as well as continuing technological advancements, researchers have focused on producing more accurate CBCT scans with better quality imaging of MB2 canals, which will facilitate the diagnosis of previously untreated MB2 canals. The results of the present study showed the detection rate for MB2 canals to be 44%, which is approximately consistent with the results of previous clinical studies (7).
The prevalence and factors affecting the identification of MB2 canals in maxillary molars have been examined in many studies (11, 41). However, little research has been conducted on MB2 canal localization in relation to the main MB canal (5, 42). Researchers found the mean distance of the MB2 canal and the mean distance of the MB2 orifice from the main MB orifice to be 2.31 mm and 1.82 mm, respectively. Gorduysus et al. (7) and Zhang et al. (43) noted that the location of MB2 canals did not only vary in relation to the main MB canal, but rather that the palatal canal orifice could be used as another reference point. Zhang et al. (43) reported that MB2 canals are located less than 1 mm mesially to the MB-P line and 2 mm palatally from the MB orifice. Moreover, Gorduysus et al. (7) investigated the location of MB2 canals and found these measurements to be 0.69 mm mesially and 1.65 mm palatally. These linear measurements of the abovementioned reference points suggest that the determination of the MB2 canal may be related to the success or failure of root canal treatment. As the linear measurements can vary from tooth to tooth, it was hypothesized that there may be an angular relationship between the reference points in the present study. The possible correlation between the existence of MB2 canals and the angles formed by the reference points, including the mesiobuccal, distal, and palatal orifices (∠MDP), was investigated in the present study. Since an ∠MDP greater than 90.95 degrees points to the existence of MB2 canals, clinicians can use this information to predict whether MB2 canals are present. The results will therefore contribute to the literature and facilitate the clinical identification of MB2 canals in maxillary first molar teeth.
The relationship between the ∠MDP and the ∠MDMB2 was also investigated in this study. According to the results, there was a strong positive relation between the ∠MDP and the ∠MDMB2. It was found that the ∠MDMB2 increased by 0.420 degrees when the ∠MDP increased by 1 degree (Figure 2). These results offer the opportunity to use the ∠MDP in order to predict the ∠MDMB2. To the best of our knowledge, only one study has previously been performed in relation to the ∠MDP (14). Here, the authors indicated that in teeth with an ∠MDP greater than 140 degrees, the MDMB2 orifice will be located closer to the line connecting the MB orifice with the palatal orifice (14). In the present study, it was suggested that the MDMB2 orifice could be found more easily via angular evaluation. This also supported Han et al.’s suggestion (14).
There were some limitations to the present study. First, the presence of MB2 in relation to the angles and, second, the reliability of the CBCT scans regarding the determination of accessory canal orifices could not be checked in this retrospective study, since it was not based on clinical or in vitro conditions. Finally, it was assumed that CBCT observations of a 4th canal are 100% reliable, although the teeth were not checked clinically or histologically. For that reason, the measurements in the present study may be varied according to the accuracy of the CBCT scans. In the light of these limitations, further studies are needed.
Bearing in mind the limitations of the present study, it could be concluded from the results that if the ∠MDP is more than 90.95 degrees, the possibility of MB2 canals in the endodontic cavity should be investigated. Due to the positive correlation between the ∠MDP and the ∠MDMB2, the localization of MB2 canals may be performed easily with reference to the main MB canal. Further studies on the localization of MB2 canals are needed in order to achieve a more reliable method.