1. Background
The development of the inferior vean cava (IVC) is a complex process and the prevalence of IVC anomaly is reported as 0.5%. Among them the prevalence of left IVC is 0.2% - 0.5% (1). The left IVC is typically limited to the infrarenal segment. It meets the left renal vein, anteriorly crosses the aorta, and joins the right renal vein to create a normal right-sided IVC (1). We present a case of an unusual left IVC with intrahepatic venocaval shunts and accompanied situs ambiguous with polysplenia, and it has not been reported yet to the best of our knowledge. IVC anomaly is significant to both radiologists and clinicians in making diagnosis and treatment plans regardless of its symptoms.
2. Case Presentation
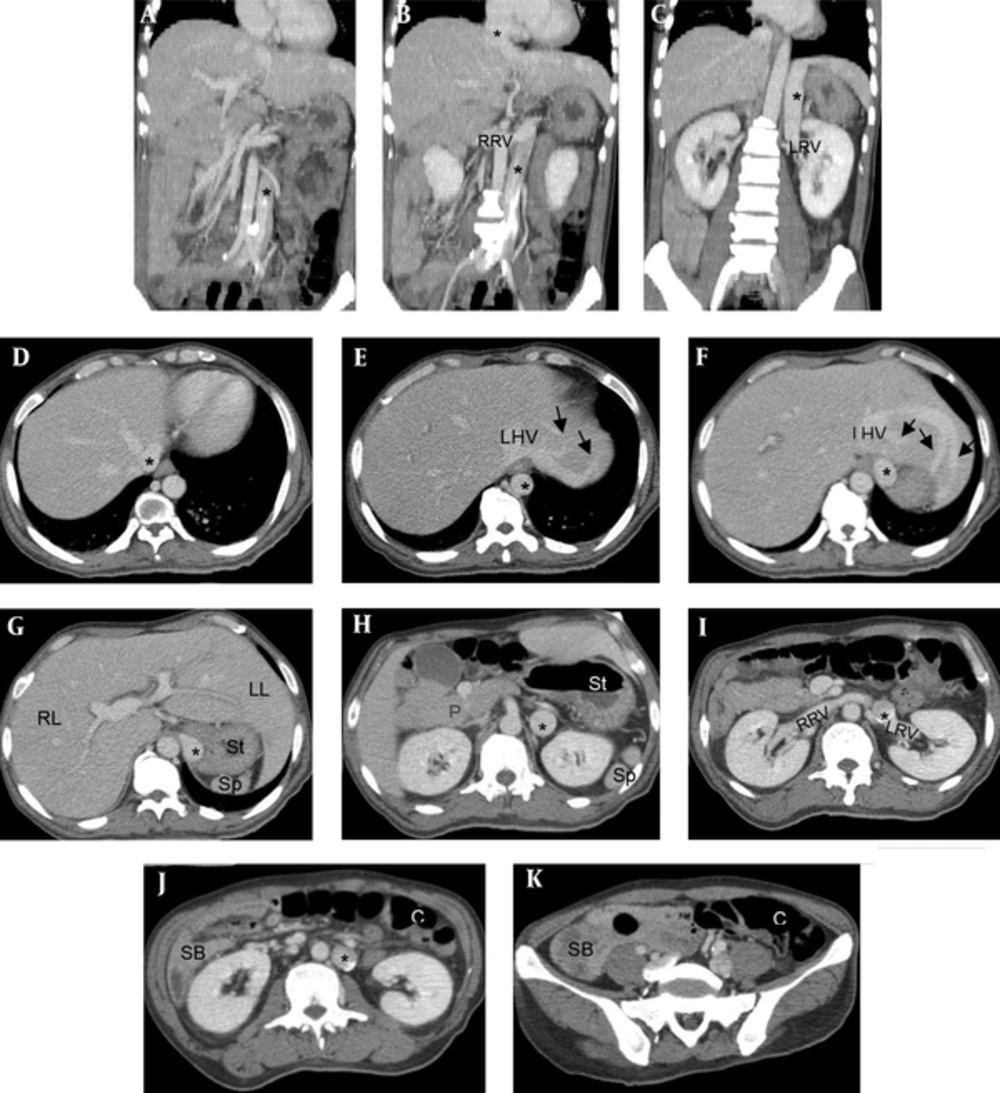
A fifty-three year-old man presented to the emergency department complaining of nausea and vomiting from two days ago and mild confusion. He had a history of type II diabetes mellitus that was being managed with an oral hypoglycemic agent (metformin), and chronic alcohol misuse for ten years. The laboratory findings showed anemia, leukocytosis, and an elevated level of alanine aminotransferase and lactic acid with hyperammonemia and hypoalbuminemia. Contrast-enhanced abdominal computed tomography (CT) scan was performed to evaluate underlying liver disease and causes of gastrointestinal symptoms. CT scan revealed a left infrahepatic IVC including infrarenal, renal, and suprarenal segments coursing straightly upward even after joining the left renal vein until it reached the retrohepatic area. Then it crossed over to the right to form a normal right-sided IVC and entered the right atrium. There were several intrahepatic anastomotic channels between the left IVC and the left hepatic vein (HV). However, abnormal enhancement of the liver related to the intrahepatic anastomoses was not seen on postcontrast images. Besides, situs ambiguous with polysplenia was detected. Centrally-located liver extending to both sides, multiple spleens in the left upper quadrant posterolateral to the stomach, and a truncated pancreas with only a visible pancreatic head on the right side was present. Intestinal malrotation was also detected (Figure 1). Other subsidiary findings were fatty liver and periportal lucency. Thorax CT scan was also performed for further work-up, and it revealed situs solitus with levocardia, a normal anatomic state, with a normal trilobed right lung and a bilobed left lung.
A 53 year-old man with left inferior vena cava (IVC) and situs ambiguous. Coronal (A - C, From the infrarenal to suprarenal segment) and axial (D - K, From cranial to caudal direction). Coronal CT images (A - C) show the left IVC involving infrarenal, renal, and suprarenal segments that courses straightly upward until the retrohepatic area and crosses over to the right side to form a normal right retrohepatic IVC and enters the right atrium. There are several intrahepatic anastomotic channels (arrows in E, F) between the left IVC and the left hepatic vein (LHV). In addition, situs ambiguous with polysplenia is seen on axial CT images: centrally located liver, multiple spleens on the left side, a truncated pancreas with an only visible pancreatic head on the right, right-sided small bowel, and left-sided colon. (*, IVC; C, colon; LHV, left hepatic vein; LL, Lt. hepatic lobe; LRV, left renal vein; P, pancreas; RL, Rt. hepatic lobe; RRV, right renal vein; SB, small bowel; Sp, spleen; St, stomach).
3. Discussion
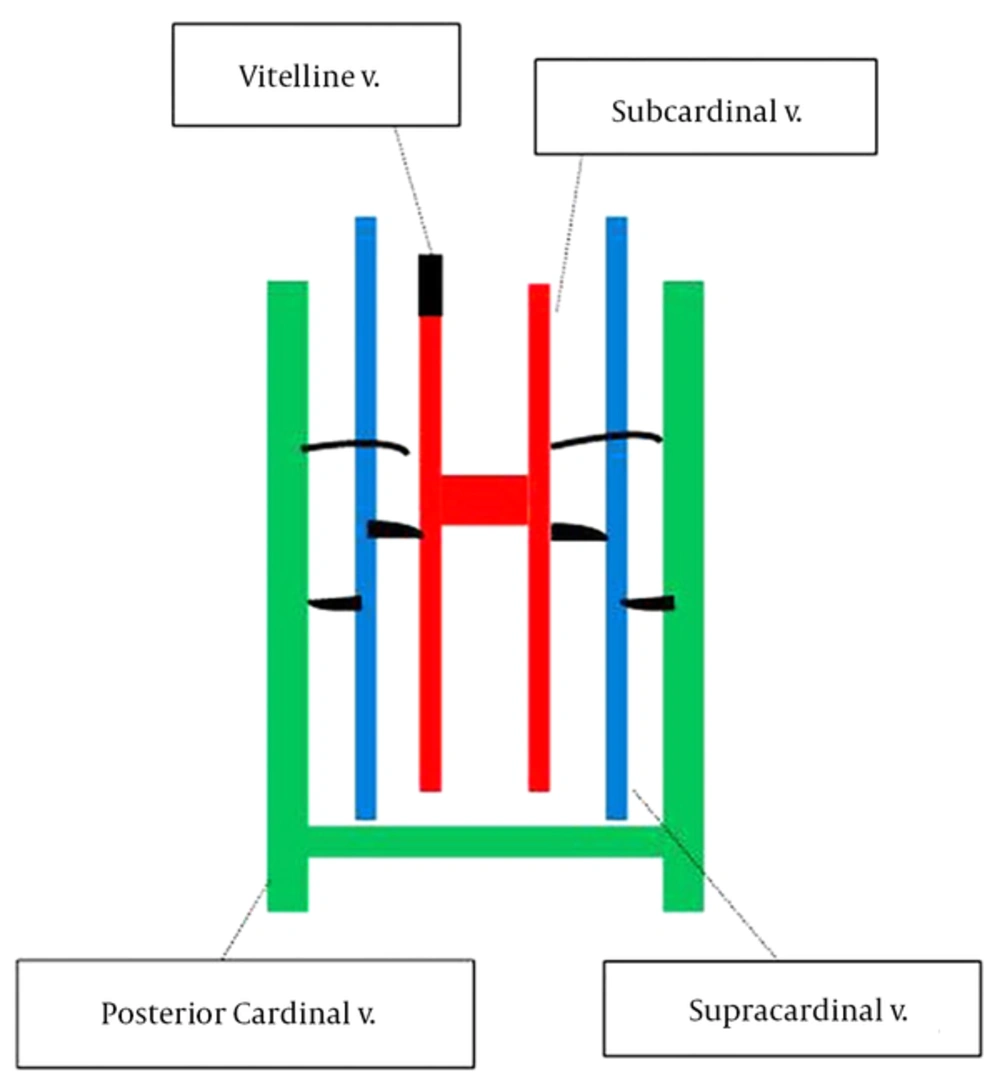
The IVC is formed by three paired embryonic veins; posterior cardinal, subcardinal, and supracardinal veins, which arise in a chronological order between the 4th and 8th week of fetal life (2-4). The relationship between the location of the three veins is shown in Figure 2. Persistence or regression with extensive anastomosis among them result in various patterns of the IVC, and the normal IVC is composed of four segments: hepatic, suprarenal, renal, and infrarenal. The frequently described anomalies are retroaortic/circumaortic left renal vein, double IVC, left IVC, interrupted IVC with azygos/hemiazygos continuation, and circumcaval ureter (2, 3). Among them, the left IVC is formed by regression of the right supracardinal vein and persistence of the left supracardinal vein (1). Typically, the left IVC anteriorly crosses the aorta at the renal hilar level to form a normal right-sided suprarenal IVC (1-4).
Schematic diagram of development of the three pairs of embryonic veins and their locations. The posterior cardinal veins (green) are the earliest to form. Subsequently, subcardinal veins (red) start to predominate. These veins are ventromedial and parallel to the posterior cardinal veins and ventrolateral to the aorta. Supracardinal veins (blue) are the latest dominant system. They are dorsomedial to the regressing posterior cardinal veins, dorsolateral to the aorta, and lateral to the subcardinal veins. (v: vein).
A few cases of unusual pattern of left IVC have been reported, such as crossing over left IVC posterior to the aorta (4, 5) and left IVC with azygos/hemiazygos continuation. There were only four reports on the left IVC that crossed over to the right at the suprarenal level; the left IVC which drained directly into the right atrium in three cases, and interrupted left IVC with hepatic venous continuation in one case (6). However in this case, the left IVC was noted in the infrahepatic level until it reached the retrohepatic area. Then it crossed over to the right and directly drained into the right atrium as seen in previous reports. Also, there were several anastomoses between the left IVC and the left HV. This course is not consistent with typical left IVC and its variants, and it has not been reported yet to the best of our knowledge. In this respect, we presumed the process of its development. With regression of the right supracardinal vein and persistence of the left supracardinal vein, persistent left supra-subcardinal anastomosis, left subcardinal vein, and left subcardinal-hepatic anastomosis may have contributed to the left IVC in renal and suprarenal segments.
As for this case, heterotaxy syndrome with polysplenia was also discovered. Interruption of the IVC with azygos or hemiazygos continuation is the second most common abnormality associated with polysplenia syndrome (6, 7). However, in this case, there were normal azygos and hemiazygos veins, and hepatic IVC.
Congenital anomalies of IVC have become more frequently encountered incidentally since the development of cross-sectional imaging. However, the knowledge about IVC anomalies has clinical significance as follows: they rarely cause symptoms; possible risk factor for lower limb thrombosis, particularly in young adults (2), intermittent celiac artery compression syndrome in IVC anterior to the aorta at the level of the celiac trunk, and compression of the left IVC coursing anterior to the abdominal aorta between the aorta and superior mesenteric artery, so-called nutcracker phenomenon (8); it can be misinterpreted as retroperitoneal lymphadenopathy or mass on cross-sectional imaging (4); it is crucial in planning the surgery and interventions, such as nephrectomy, renal transplantation, aortic aneurysm repair, IVC filter placement, and transjugular intrahepatic portosystemic shunt.
In conclusion, the infrahepatic left IVC with retrohepatic crossing over and intrahepatic venocaval shunts is a unique variant not reported so far. Regardless of symptoms, the knowledge about IVC anomaly is crucial for radiologists and clinicians to avoid misdiagnosis and to plan properly for surgical and interventional procedures.