1. Background
Although new technologies in screening tools are being utilized increasingly, second trimester sonographic examination for risk assessment of chromosomal abnormalities is still an important component of prenatal evaluation. Screening for structural malformations, or for Trisomy 21, Trisomy 18 and open neural tube defects are the most important functional area of second trimester detailed ultrasound. The sensitivity of genetic sonogram in the detection of Down syndrome varies widely in low and high-risk populations (1-3).
2. Objectives
In our study, we have evaluated the second trimester ultrasound findings of the fetuses with Down syndrome before termination of their pregnancies.
3. Patients and Methods
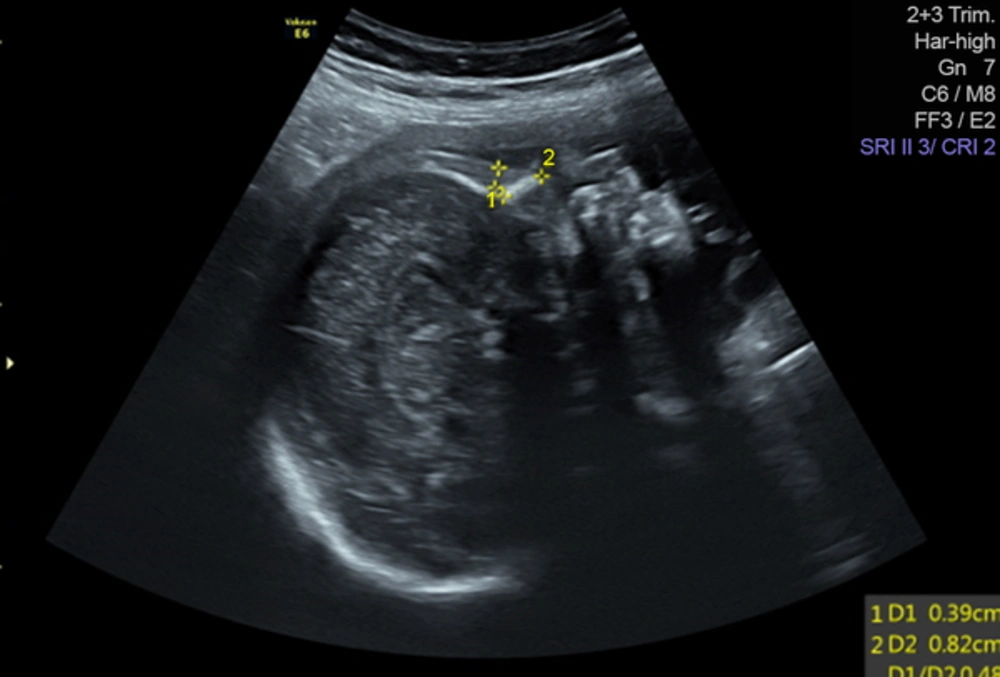
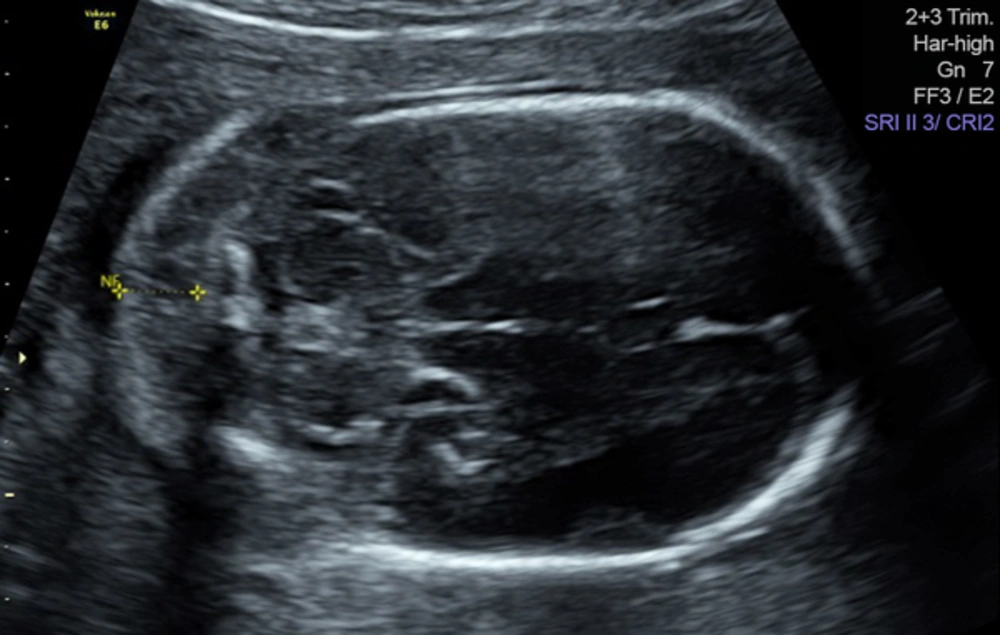
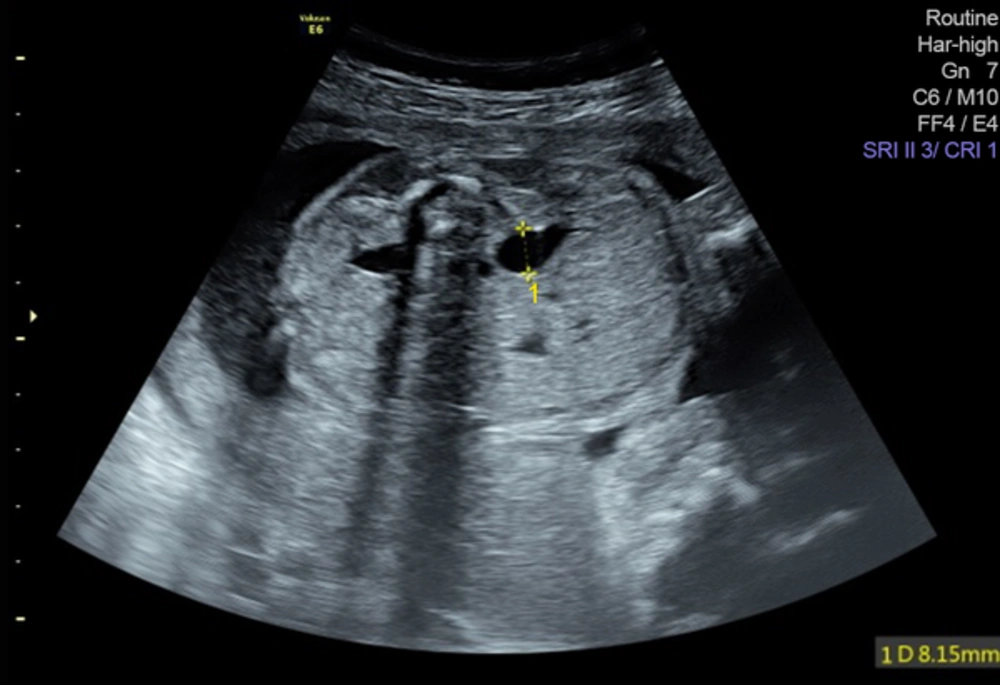
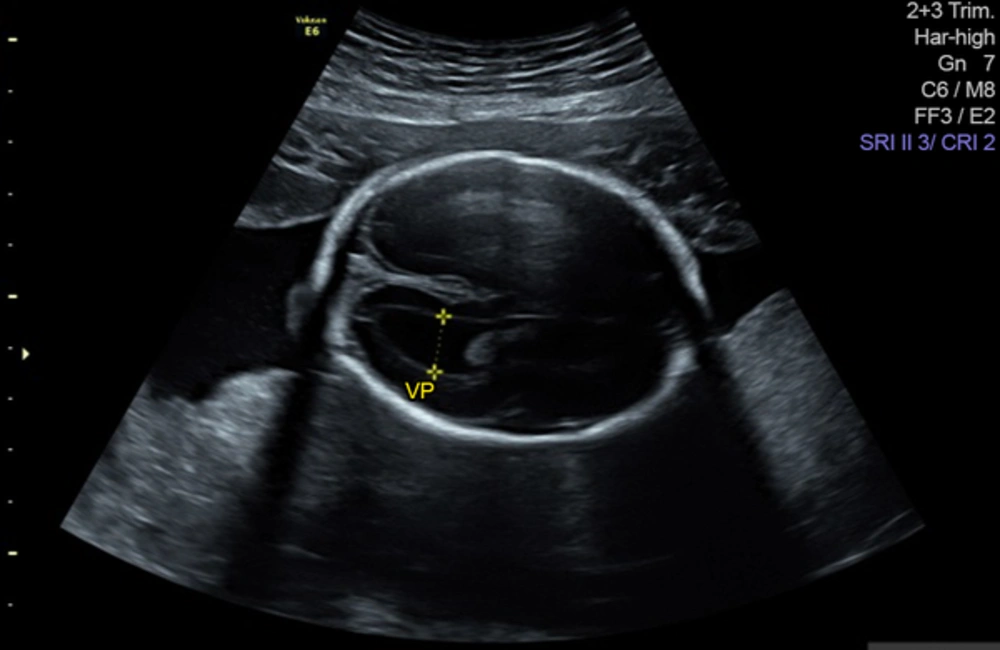
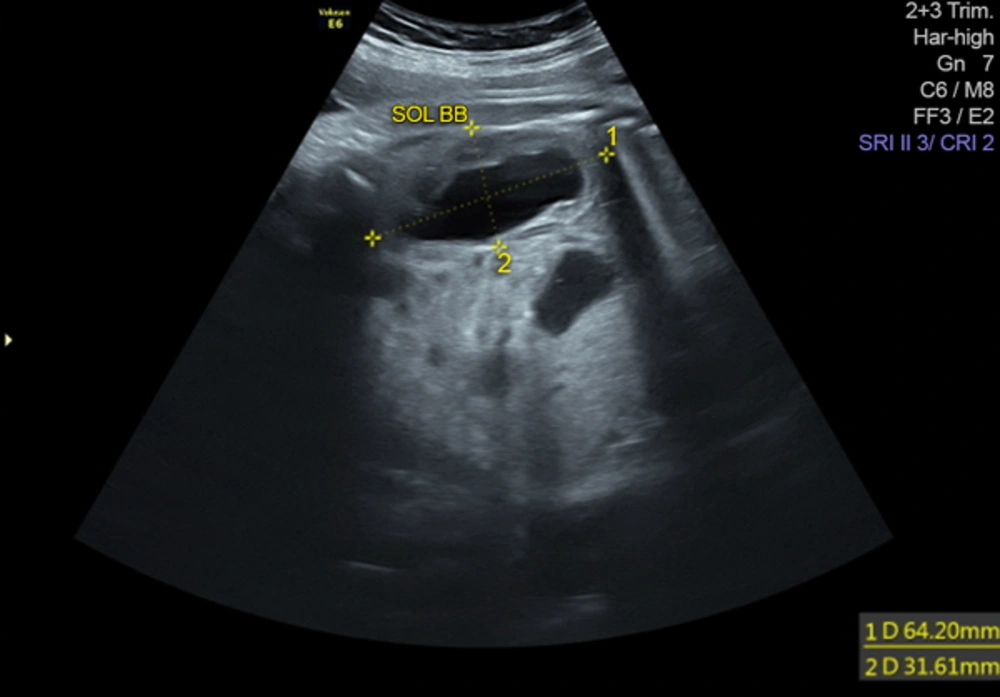
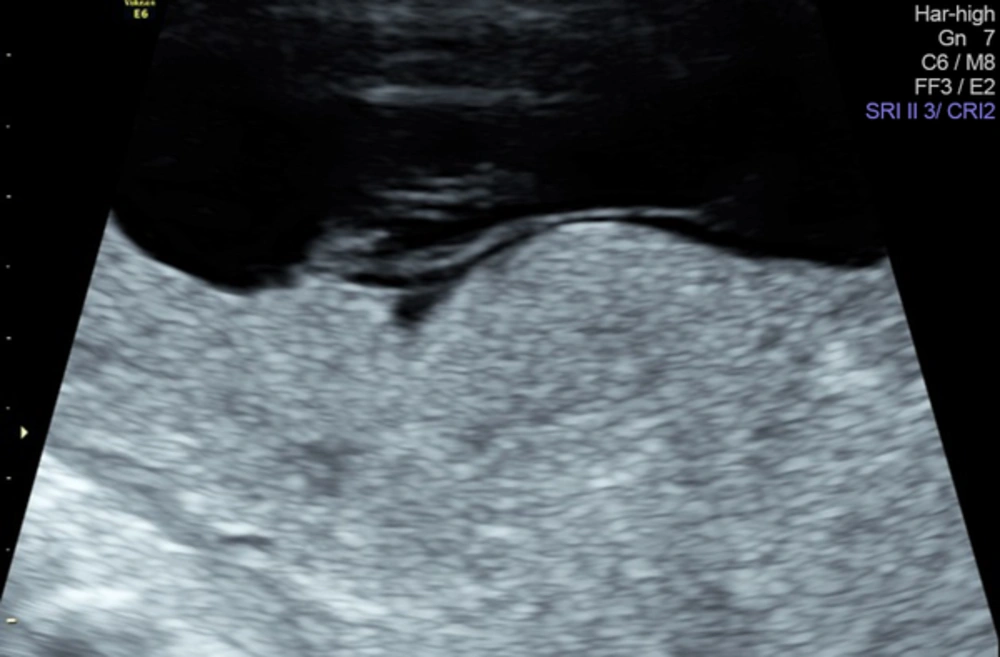
We have retrospectively evaluated 781 patients who underwent invasive procedure for fetal karyotyping at the maternal fetal unit, medical faculty of Trakya University between November 2011 and November 2015. High risk in screening tests (> 1/270), nuchal thickness (> 3 mm), nuchal fold thickness (> 6 mm), major structural malformation, and two minor markers were the indications for karyotyping. The study was approved by the local ethics committee. Cases with the result of trisomy 21 were included in the study. These patients were divided into groups according to the indications for karyotyping. Positive combined test, positive triple test, positive quadruple test and pathologic sonographic findings were the groups. Nuchal thickness > 3,0 mm, nuchal fold thickness > 6 mm, cystic hygroma and major structural anomalies were classified in the ultrasound group (Figures 1 - 4).
Second trimester sonographic findings of the fetuses were analyzed. The fetuses that were terminated in the first trimester were excluded from the second trimester sonographic findings group. Major structural malformations and second trimester Down syndrome markers (hyperechoic bowel, echogenic intracardiac focus, nuchal fold, pyelectasis, hypoplastic nasal bone, choroid plexus cysts, short femur-humerus, aberrant right subclavian artery, and sandal gap were evaluated (Figures 5 and 6).
Sonographic examinations were performed by two experienced operators in the prenatal diagnosis unit using a Voluson 730 Expert machine (Voluson 730; General Electric, Tiefenbach, Austria) fitted with a 2 - 7 MHz convex abdominal probe. All ultrasound examinations were checked again by two extensive experienced operators who had a professor degree in perinatology.
Statistical analyses was performed by the NCSS 2007 (NCSS; Utah, USA) pocket program. Univariate analysis (UA) comparisons were made using Students T Test for continuous variables and Fischers exact test for categorical variables. Definitive statistics for numeric variables was presented in median (min-max) and in percentage and frequency for categorical variables.
4. Results
Trisomy 21 was detected in 26 (3.3%) patients. The median (min-max) maternal age of trisomy 21 cases was 31.9 (17 - 41) years. Karyotype indications were; the risk at combined test in 13 patients (50%) (combined test group), the risk at triple test in five patients (19.2%) (triple test group) and risk at quadruple test in two patients (0.7%) (quadruple test group). Ultrasound findings those of which necessitated karyotyping in the remaining six (23%) patients were accepted as abnormal ultarsound group. The patients in the abnormal ultrasound group had no screening test except one case which had “low risk” according to both combined and triple tests.
Trisomy 21 was detected in four (15.3%) patients by chorion villus biopsy at the first trimester. Thus, second trimester ultrasound was performed in the 22 out of our 26 women. However, there were sonographic findings in only 16 (72.7%) patients. Six (27.2%) fetuses had no minor or major anomaly at the detailed ultrasound examination. The frequency of major cardiac anomaly was 22.7%. Choroid plexus cyst and aberrant right subclavian artery were the single findings at the second trimester ultrasound exam in two fetuses with Down syndrome (Table 1).
| Case No | Indication for invasive test | Sonographic findings |
|---|---|---|
| 1 | Combined test | Hyperechoic bowel, echogenic intracardiac focus, cardiac anomaly (18 w) |
| 2 | Quadruple test | Echogenic intracardiac focus, shortened nasal bone (19 w) |
| 3 | Combined test | Shortened nasal bone, hyperechoic bowel (16 w) |
| 4 | Triple test | ARSA (20 w) |
| 5 | Ultrasound | Unilateral talipes , uncompleted chorioamniotic fusion (27 w) |
| 6 | Quadruple test | Shortened nasal bone, prenasal thickness, flattened nasal bridge (21 w) |
| 7 | Nuchal thickness | Nuchal thickness (14 w) |
| 8 | Triple test | Nuchal fold thickness, echogenic intracardiac focus (21 w) |
| 9 | Combined test | No finding (16 w) |
| 10 | Combined test | Atrioventriculer septal defect (18 w) |
| 11 | Combined test | Nuchal fold thickness (18 w) |
| 12 | Combined test | Nuchald fold thickess, hyperechoic bowel (19 w) |
| 13 | Combined test | Nuchal thickness (14w) |
| 14 | Combined test | Nuchal thickness (14w) |
| 15 | Triple test | No finding (19 w) |
| 16 | Combined test-triple test | No finding (19 w) |
| 17 | Triple test | AVSD, hyperechoic bowel (20 w) |
| 18 | Combined test-triple test | No finding (18 w) |
| 19 | Combined test-triple test | Choroid plexus cyst (19) |
| 20 | Ultrasound | Nuchal fold thickness, mild ventriculomegaly, echogenic intracardiac focus (20 w) |
| 21 | Combined test | No finding (16 w) |
| 22 | Ultrasound | Nuchal fold thickness, overriding aorta, sandal gap |
| 23 | Combined test | Absent nasal bone, bilateral pyelectasis, choroid plexus cyst (18 w) |
| 24 | Nuchal thickness | Cystic hygroma (16 w) |
| 25 | Nuchal thickness | Cystic hygroma (13 w) |
| 26 | Triple test | No finding (19 w) |
Abbreviations: ARSA, aberrant right subclavian artery; AVSD, atrioventricular septal defect; W, week.
Second trimester ultrasound was available in 11 patients in the combined test group. Ultrasound revealed pathologic findings in 9 (81.1%) of these 11 patients (Table 1).
Second trimester ultrasound detected pathologic findings in three (3/5, 60%) women in the triple test group. Likewise, all fetuses in the quadruple test group had sonographic findings in the second trimester ultrasound (2/2, 100%).
In six women, sonographic findings consisted the karyotype indication (23%). There were no available screening test in five patients in this group. Increased nuchal translucency in the first trimester, nuchal fold thickness, ventriculomegaly, cardiac anomaly in the second trimester necessitated karyotyping in these cases. One case in the ultrasound group had both of combined test and triple test. In this patient, the results of both tests were in the low risk area, but talipes equinovarus and delayed chorioamniotic fusion were observed at 27 weeks of gestation. Cordocentesis revealed trisomy 21 (Figure 7).
5. Discussion
Second trimester genetic ultrasound in low risk patients may improve the performance of first and second trimester screening tests. It may reduce the false positivity and increase the detection rates of Down syndrome (1). In a large, prospective, single-center cohort study it has been shown that after accounting for gestational and maternal age, all pregnancies with nuchal fold, short humerus, echogenic bowel, echogenic intracardiac focus, pyelectasia and aneuploidy associated anomalies had a significantly increased risk for Down syndrome (2).
In another study, the most common sonographic markers for Down syndrome were observed as nuchal thickening, hyperechoic bowel, shortened extremities and renal pyelectasia. Sensitivity of sonographic screening Down syndrome was 69% with a false positive rate of 8% when multiple sonographic markers and structural abnormalities were detected together (3). Although these studies have pointed out the significance of the second trimester ultrasound, in cases that have high risk in the triple test, avoiding amniocentesis based on normal sonographic findings may miss nearly half the cases with Down syndrome (4).
The sensitivity of genetic ultrasound for Down syndrome ranges between 62.5% and 82% (5, 6). In our series, 72.2 % of the cases had sonographic findings in the second trimester ultrasonography. In 2001, it was reported that nuchal thickness was the most common (37.2%), sonographic finding in the cases with Down syndrome. Short femur and echogenic intracardiac focus were the commonly seen anomalies following nuchal fold (7). Nuchal fold thickness was also the most common second trimester finding of our series. However, nuchal fold thickness was followed by hyperechoic bowel and echogenic cardiac focus in our series. The risk of trisomy 21 increases by the increasing number of markers. In a large series, two or more markers were detected in nearly one third of the fetuses with trisomy 21 (7). Likewise, nineteen out of 22 cases in our study had multiple markers.
Recently published meta-analysis of 48 studies gave the likelihood ratios of the sonographic markers for Down syndrome. The pooled positive likelihood ratios were 5, 83 for echogenic intracardiac focus; 27, 52 for ventriculomegaly; 23, 30 for increased nuchal fold; 11, 44 for hyperechogenic bowel; 7, 63 for mild hydronephrosis; 3, 72 for short femur; 4, 81 for short humerus; 21, 48 for aberrant right subclavian artery and 23, 27 for absent and hypoplastic nasal bone (8). Aberrant right subclavian artery follows ventriculomegaly and increased nuchal fold in this meta analysis. Two of our cases had only one sonographic finding; namely, aberrant right subclavian artery and choroid plexus cyst. A recently published meta-analysis found that the prevalence of aberrant right subclavian artery in Down syndrome fetuses was 23.6%, whereas it was 1.02% in euploid fetuses. It was concluded that there is no sufficient evidence to recommend karyotyping in cases with isolated aberrant right subclavian artery. Conclusively, fetal karyotyping was advised to cases with high background risk and with additional markers (9).
The most interesting case in our study was the one with delayed chorioamniotic fusion who had negative screening tests in the first and second trimester. Cordocentesis was performed at the 27th week of pregnancy due to unilateral talipes and delayed chorioamniotic fusion. The association between the delayed fusion of the chorion /amnion and Down syndrome was previously reported in a case report and case series. These studies concluded that delayed fusion of chorion and amnion is an indication for karyotyping when an additional abnormality is found (10, 11). In our case, talipes was the additional finding.
Delayed chorion and amnion in fetuses with Down syndrome might be part of a developmental delay in malformed pregnancies. But the sample size was so small and more data are needed to clarify the significance of this sign.
Six patients (27.2%) with Down syndrome had no marker at the second trimester ultrasound examination. Thus, although we studied in a series with limited number of women we can assert that one in three patients with Down syndrome revealed no detectable sonographic finding according to our current knowledge.
In Conclusion, this point is especially important in borderline cases. To avoid amniocentesis based on normal genetic sonogram in patients with a high-risk score on screening tests would not be a judicious option. It should be kept in mind that second trimester ultrasound is not strong enough to exclude the diagnosis of Down’s syndrome.