1. Background
The incidence of developmental dysplasia of the hip (DDH), which refers to a hip with an abnormally shaped and sized acetabulum and femoral head, varies significantly within racial groups by geographic location. Left-sided hip dysplasia is more common in patients with unilateral DDH. The risk factors for DDH include female sex, breech presentation, family history, oligohydramnios, and first-born status. Ultrasound screening is recommended for babies at risk (1, 2). Severity of DDH ranges from a subtle form to subluxation and hip dislocation. The preferred method for the diagnosis of DDH is ultrasound examination between 6 weeks and 6 months of age. X-ray imaging is required for babies with significant femoral head ossification, which occurs at approximately 6 months of age. Ultrasound examination is recommended between 4 - 6 weeks for babies with high risk. Since physiological hip dysplasia is common in neonates, ultrasound evaluation is not recommended before 4 weeks of age to avoid false positive results.
Early diagnosis has a crucial role in the treatment of DDH, and acetabular alpha angle measurement using the Graf method is the preferred method. However, reliable measurements using this approach depend on obtaining a standardized coronal plane ultrasound image that shows a flat horizontal iliac wing, bony and cartilaginous acetabular roof, labrum, and os ischium. In normal hips, an alpha angle greater than 60 degrees is expected. An alpha angle between 50 and 59 degrees is accepted as mild dysplasia, 43 - 49 degrees as moderate dysplasia, and less than 43 degrees as severe dysplasia.
Probe orientation is key to obtaining the correct measurement of the alpha angle but is it still possible to misdiagnose DDH, despite having images that meet the standard Graf plane criteria (flat iliac wing, labrum, acetabular roof, and os ischium). Because of the complex anatomy and varying probe orientations, there is a risk for improper measurement; dysplastic hips can be detected with normal alpha angles and vice versa (3).
Prognosis is very good in patients who are treated timely, and the preferred initial treatment method is closed reduction. This procedure has a high success rate, however, open reduction may be needed for unsuccessful closed reductions. In its subtle form, DDH may not be diagnosed until adulthood, and osteoarthrosis development may be seen in these patients (4).
Computed tomography (CT) is not a preferred method for the diagnosis of DDH, being reserved for post-reduction evaluation of dysplastic hips and for follow up. If a child is in a spica cast, for example, it is difficult to evaluate hips on radiographs, so CT can provide valuable images of the infant hip because of the ability to view the positioning in the axial plane; hence it is useful to confirm an adequate reduction (5). Using low-dose scanning techniques, estimated as low as 1 mSv, it is possible to achieve an adequate radiation dose for hip radiography (6). The relationship between the femoral head and the acetabulum is the subject of the CT evaluation in these patients, so a detailed CT assessment of iliac bone has not been described in previous studies.
2. Objectives
In this study we aimed to determine imaging features of DDH before 20 months of age using CT after closed or open hip reduction by evaluating mean cortical thickness of the acetabulum, acetabular surface and marginal irregularity, acetabular subcortical sclerosis, and shallowing by comparing DDH hips to normal hips from a control group.
3. Patients and Methods
3.1. Patients
The ethics committee approval was received by the university review board, and informed consent was waived. We retrospectively evaluated all patients aged 2 - 20 months who underwent hip CT examination between March 2013 and August 2016 from our institution’s picture archiving and communication system. We included postreduction CT images of DDH patients who had either an open or closed reduction that was also confirmed in the electronic medical records. CT scans were performed within 24 hours after reduction. We excluded patients with low quality CT images due to motion and metallic artefacts, patients for whom CT was performed because of hip trauma, and patients with neuromuscular diseases, dislocated hips, and type 2 Arnold-Chiari malformations. History of hip trauma and known skeletal or joint diseases were excluded in both patients and control groups.
The control group included patients who were referred for abdominal CT because of suspected abdominal disease or vertebral anomalies. CT images that did not fully cover the hip joints were not included in the study.
CT images of 102 consecutive patients with DDH (90 females, 12 males; age range 1 - 20 months; mean age, 11.7 months) and 51 age-matched controls (26 females, 25 males; age range 1 - 20 months; mean age, 11.2 months) were included in our study. Control group was consisted of with the reference/diagnosis of hepatoblastoma (n = 3), Wilm’s tumor (n = 5), diaphragmatic hernia (n = 3), meningomyelocele (n = 5), bowel perforation due to needle ingestion (n = 2), intestinal malrotation (n = 5), post traumatic liver laceration (n = 4), midgut volvulus (n = 4), colonic duplication (n = 2), colonic perforation due to necrosis (n = 3), Meckel’s diverticulitis (n = 2), falling from height (n = 2), vertebral segmentation anomalies with meningocele (n = 2), acute abdominal pain (n = 6) and ureter stone (n = 3).
3.2. Computed Tomography Imaging
Multidetector computed tomography scans were performed using a 64-detector row scanner (Aquilion; Toshiba, Tokyo, Japan) with the following parameters: 80 kV, variable mA (sure exposure), 0.5-mm section thickness, 0.35 s per rotation, and 1.1 beam pitch. Examinations were performed in the supine position with craniocaudal scanning.
3.3. Computed Tomography Evaluation
CT examinations were evaluated by two independent radiologists each with 12 years of experience (musculoskeletal and pediatric radiology). Images were interpreted in chronological order and the earliest examination was interpreted in patients with two or more CT images. Evaluation of acetabula was performed using a digital imaging and communications in medicine (DICOM) viewer (OsiriX MD 9.0, Pixmeo SARL, Berne, Switzerland) on coronal sections.
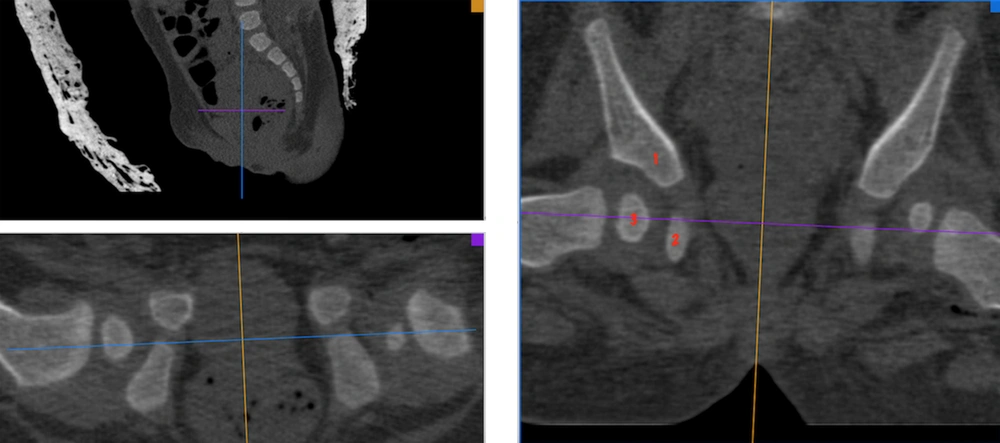
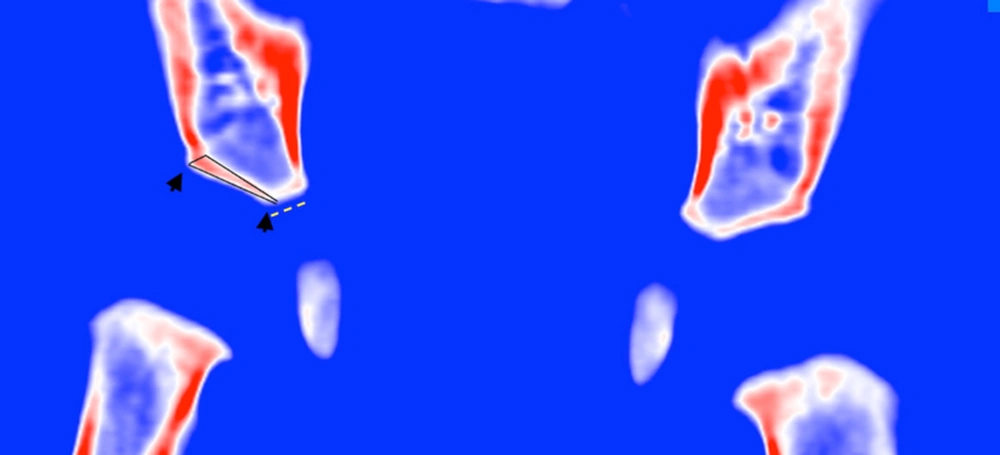
Transverse CT images of DDH patients and controls were used to generate three-dimensional (3D) multiplanar reformatted images. Bone window and colour look-up table images were used for evaluation. To measure from nearly same exact position, interpretations were made from a coronal reformatted image that included the central part of femoral head, ischium pubis, and central part of acetabulum (Figure 1). CT images were used for measurement of the acetabular cortical bone thickness, acetabular surface irregularity, subcortical sclerosis, shallowing, and shape abnormalities.
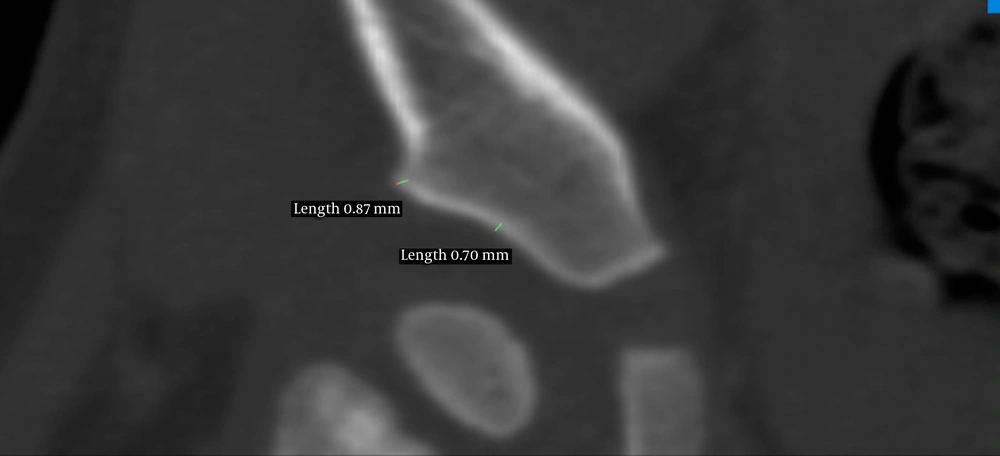
The radiologists measured cortical thickness of acetabulum, thickness of iliac bone, and noted the condition of the acetabular surface - margin irregularities, acetabular shallowing, and subcortical sclerosis. For measurement of the cortical thickness, cursors were placed in the dense cortical bone borders of the iliac bone at the central part of acetabulum and the superior acetabular margin (Figure 2). In patients with bilateral DDH, the severity of dysplasia on each side was interpreted by evaluating acetabular shallowing and the severity of marginal flattening. Iliac bone thickness at the level of the inferior acetabular margin was measured and the thicker side was considered more dysplastic.
3.4. Statistical Analysis
After the validation of normal distributions using Shapiro-Wilk test, Student’s t-test was performed to assess differences in the cortical thickness of dysplastic and normal hips. All values are expressed as mean ± standard deviation, and a P value of 0.05 was considered significant.
Interobserver agreement was calculated using kappa statistics for the presence of acetabular surface irregularity, subcortical sclerosis, shallowing, and shape abnormalities. Dysplatic hips and normal hips were investigated separately for each patient. The kappa values were interpreted as follows: values between 0 and 0.2 represent poor agreement, 0.21 and 0.40 fair agreement, 0.41 and 0.60 moderate agreement and 0.61 and 0.80 substantial agreement. A value above 0.80 is considered excellent agreement.
For the thickness of the acetabular cortex and iliac bone thickness agreement was measured using the differences in the values provided by the two observers. Significant difference existed among the values measured by the two radiologists regarding thickness of the acetabular cortical bone thickness and iliac bone thickness at the level of the inferior acetabular margin. The interobserver variability for acetabular cortical bone thickness and iliac bone thickness was analyzed by calculating the intraclass correlation coefficient. Statistical analyses were performed using GraphPad Prism 7 for Mac (GraphPad Software, San Diego, CA).
4. Results
Ninety of 102 DDH patients were girls (88%). Mean age was 11.7 ± 0.6 months (range 2 - 20 months) in DDH patients and 11.2 ± 0.9 months (range 2 - 20 months) in the control group.
Forty-four patients (43%) showed unilateral DDH and 58 (56%) had bilateral DDH. Of the 44 unilateral DDH patients, 11 were right-sided (25%) and 33 were left-sided (75%). Of the 58 bilateral DDH patients, the right side was more dysplastic in 33 patients (56 %), and the left side was more dysplastic in 25 patients (43 %).
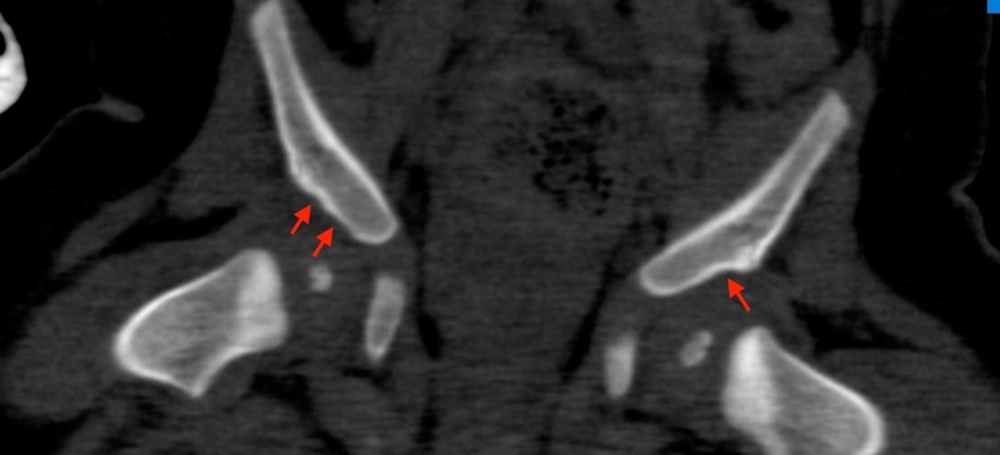
Acetabular margin irregularity was present in all the patients with unilateral DDH and 55 of 58 (94%) patients with bilateral DDH. Six of 55 patients with bilateral DDH who had marginal irregularity showed one-sided marginal irregularity and/or flattening. In DDH patients, the acetabular margin was flattened on the dysplastic side (Figure 3), whereas it was sharp edged in the normal hips of the control group.
Acetabular surface irregularity (Figure 4) was present in 37 of 44 of the unilateral dysplastic hips (84%). In 58 patients with bilateral DDH, 49 showed bilateral acetabular surface irregularity (84%), 4 showed irregularity on only one dysplastic side (6%), and there was no irregularity in 5 patients (8%).
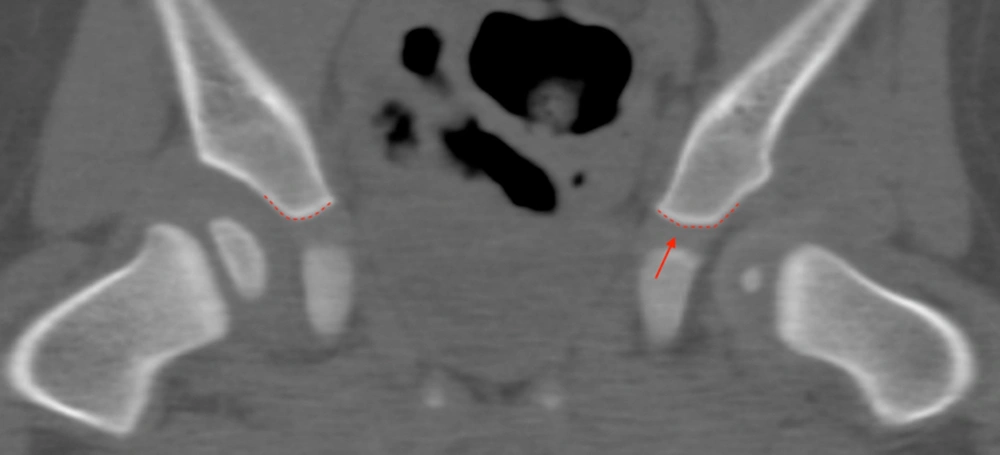
Thickening on the inferior part of the ilium that forms acetabulum, which causes shallowing compared to the normal side, was seen in 41 of 44 of the unilateral DDH patients (93%). In these patients, there was also smooth angulation on the inferior margin (Figure 5).
There was no significant difference between the cortical thicknesses of left and right hips of controls (Table 1). In the 44 patients with unilateral DDH, the mean cortical thickness measured from the central part of acetabulum on the coronal reformatted images was 0.86 ± 0.03 mm and 0.65 ± 0.03 mm on the normal and dysplastic sides, respectively (P = 0.0001) (Table 2). This difference was more distinct at the marginal (acetabular rim) cortical thickness, measuring 1.11 ± 0.06 mm and 0.70 ± 0.04 mm on the normal and dysplastic side, respectively (P = 0.0001). The acetabular cortex was thinner in the more dysplastic side of the hip in patients with bilateral DDH.
In patients with unilateral DDH, 37 of the 44 patients (84%) had a shallow acetabulum on the dysplastic side. Fifty of 58 patients with bilateral dysplastic hips showed bilateral shallow acetabula (86%), 4 had a shallow acetabulum on only one dysplastic side (6%), and there was no shallow acetabulum on 4 of these hips (6%).
Subcortical sclerosis was present in 19 of the 44 unilateral dysplastic hips (43%). Bilateral subcortical sclerosis was present in 17 of the patients with bilateral dysplasia (29%); there was no sclerosis in 26 of these patients (44%), and 8 had subcortical sclerosis on the more dysplastic side (14%).
For agreement in the interpretations of acetabular surface irregularity, subcortical sclerosis, shallowing, and acetabular rim irregularity the values were 0.82, 0.79, 0.76 and 0.94, respectively, between radiologists. For acetabular cortical bone thickness and iliac bone thickness, respectively, interobserver agreement rates were 0.78 and 0.94. The lowest agreement was noted for the presence of acetabular shallowing, while the highest agreements were noted for the presence of acetabular rim irregularity and measurement for the iliac bone thickness.
5. Discussion
Ultrasound is the preferred method for the evaluation of DDH in infants between 6 weeks and 6 months of age. Alpha angle measurement using the Graf method is the accepted diagnostic method, however, variations in probe orientation can result in significant changes in the measured alpha angle. Thus, it is possible to generate many acceptable images with different alpha angles, which can result in different Graf categories for the same hip (3).
To our knowledge, there is no study in the literature investigating CT findings for the primary diagnosis of DDH. Most of the studies focusing on DDH and CT are related to the post-reduction assessment of hips (7). We investigated CT for its possible supportive role in the diagnosis of DDH.
Acetabular cortical thicknesses did not reveal a significant difference between left and right hips in the control group. Acetabular margins (rim) were sharp edged or had a beak-like appearance in normal hips and there was no acetabular surface irregularity and shallowing in the control group.
Most of the patients with DDH were girls in our study (88%), which is consistent with previous studies. In a study by LeBa et al., DDH was found to be more common in females (83%) (8).
Bilateral DDH was more common than unilateral DDH in our study. This finding is consistent with some previous studies, (9) but the bilateral occurrence rate is not clear since previous studies have reported varying results (10).
All the unilateral DDH patients showed acetabular bony margin irregularity and flattening. In addition, 94% of bilateral DDH patients showed either focal or diffuse acetabular bony margin irregularity and flattening. Hence, acetabular marginal irregularity and flattening was the most frequent and reliable finding in the diagnosis of DDH in our study. This part of hip is also visible on ultrasonography, so it can be a reliable finding in the diagnosis of DDH. Marginal irregularity and flattening were seen even in 2-month-old babies. Therefore, acetabular margin evaluation might be an important part of ultrasonography screening in babies at risk. A sharp angled or beak-like acetabular rim is highly suggestive of a normal hip.
Another frequent finding was seen in the inferior part of the acetabulum in patients with unilateral DDH. A shallow acetabulum, caused by a thicker ilium compared to the normal side in these patients, was seen in 93% of the dysplastic hips. There was also a smooth angulation on the inferior margin compared to the normal side. This finding cannot be evaluated with ultrasonography; therefore CT imaging might be needed for patients suspected of having this condition. To our knowledge, this finding was not reported before in literature.
In normal hips, a triangular shaped acetabular cortex without any irregularity was seen. The acetabular cortex was thicker in the superolateral aspect and thinner in the inferomedial aspect of the acetabulum in normal hips. The lateral aspect of normal hips showed a sharp beak-like margin (Figure 6). In dysplastic hips, the triangular shaped acetabular cortex was not seen in most cases, rather, the cortex was irregular with focal thinning, and the superolateral aspect of the acetabulum was irregular and flattened in the coronal reformatted images.
Coronal reformatted CT image. Color clut image of normal hips of a 3 month-old baby. Normal hips with a sharp angled or beak like acetabular margin is seen (arrows). Acetabular cortex with triangular shape, thickest at superolateral aspect and thinnest at inferomedial aspect showing gradual decrease in thickness (black lines).
In patients with unilateral DDH, the mean acetabular cortical thickness of the dysplastic hips was significantly lower than that of the normal side in the central part and the acetabular margin. Cortical thinning might be related to an insufficient vascular supply of the iliac bone on the dysplastic hip side. In a study by Meng at al., decreased femoral head perfusion was showed in children with DDH (11). In patients with bilateral DDH, acetabular cortical thickness was somewhat lower in the most severe dysplastic side, however, this difference was not significant. Cortical thinning was most prominent in the acetabular margins of the dysplastic hips.
Acetabular surface irregularity was seen in 82% of the dysplastic side in patients with unilateral DDH, and 91% in bilateral DDH. The youngest baby with surface irregularity was 2 months old. In the control group, most of the hips had a regular acetabular surface, although a minimal smooth undulation was present in a small number of them. Sometimes dysplastic hips showed minimal irregularity, which can be difficult to view on ultrasonography. Further studies are needed to evaluate the visibility of surface irregularities with ultrasound examination.
The relationship between a shallow acetabulum and an underdeveloped femoral head in the development of hip dysplasia is well known. In our study, a shallow acetabulum was seen in 84% of the unilateral dysplastic hips and in 86% of the bilateral dysplastic hips. It is difficult to identify a shallow acetabulum in 2-month-old babies because of physiologic dysplasia; in these age group, the acetabula of normal hips are also shallow in appearance.
Subcortical sclerosis was not a frequent finding in our study, and we saw no cases of it in 2 or 3-month-old babies. The youngest baby with subcortical sclerosis was 4 months old.
In conclusion, our study demonstrates that acetabular marginal irregularity and flattening is an important finding in the diagnosis of DDH when combined with bone thickening in the inferior part of ilium. CT cannot be recommended as an initial modality in the diagnosis of DDH, but extra attention should be given to marginal irregularity of acetabulum during ultrasound imaging. To know the changes related to DDH in the acetabulum will help in the diagnosis of DDH in patients older than 6 months old with a pelvic CT scan due to diseases other than DDH.