1. Background
The high prevalence of colorectal cancer (CRC) and its increasing incidence can be a major problem in cancer management (1). The incidence of rectal cancer is estimated to be 35% of total CRC incidence in the European Union (2). The lung is the most common extrahepatic site of distant metastasis from CRC with an incidence of 10% (3, 4). Lower rectal tumors have a higher incidence of lung metastasis owing to systemic venous drainage of this portion as opposed to the venous drainage of the colon through the portal system (3, 5). It has been hypothesized that, in the absence of hepatic metastasis, it is uncommon for colonic tumors to spread to the lung (6). When pulmonary metastasis is diagnosed, a patient no longer undergoes unnecessary colorectal surgery and is given alternative treatment (5). The precise staging like the tumor, node, metastasis (TNM) staging system is important for deciding upon CRC treatment protocol (2, 7) and lung evaluation is helpful in determining metastasis in staging. The low incidence of pulmonary metastasis, the cost of the CT scan, exposure to radiation and uncertainty of treatment due to the prevalence of unspecified lesions limits the clinical value of routine preoperative chest CT (CCT) (7).
2. Objectives
The current study was undertaken to compare the efficacy of chest X-ray (CXR) and CCT in preoperative staging of colon and rectal cancer.
3. Patients and Methods
3.1. Patients and Imaging Studies
In a cross-sectional study, 377 patients with new histopathological diagnoses of CRC referring to Taleghani hospital, a tertiary care referral center for gastrointestinal diseases in Tehran, Iran, were included for preoperative screening between 2014 and 2017. CRC cases with T0 values were excluded. The patients underwent both CXR and CCT without contrast. The data on liver metastasis and paraaortic lymphadenopathy were gathered by abdominal CT scan with contrast. PA digital radiography was taken in the upright position. A CT scan of the abdomen was performed on a 16-slice scanner (Toshiba Aquillion) after intravenous contrast injection (visipaque 320; 90 mL; 3 mL/sec) in the portal venous phase with a slice thickness of 1 mm, 120 kVp, 250 mAs and reconstruction of 0.8 mm. The images were revised by a radiologist with 15 years of experience in thorax imaging. The CXR findings were classified as normal/benign or suspicious and the CCT findings were classified as normal/benign, indeterminate or suspicious nodules. The interval of CXR and CCT reporting was 10 days to prevent recall bias. Patients with suspicious nodules in CCT underwent diagnostic procedures such as a CT-guided biopsy, bronchoscopy and thoracotomy depending on the location of lesions and status of the patients or were followed with chemotherapy treatment.
3.2. Ethical Statement
All patients were followed up with a detailed description of the purpose of the research and written consent was obtained. Patient names were not included in the study and coding was used to classify the information. The benefits of participation in the plan were to undertake an important step in the staging of the tumor before surgery which has a significant effect on the treatment process. The cost of participation in the scheme was free. Possible complications included exposure to radioactive radiation, sensitivity and nephropathy by contrast media. The likelihood of contrast-induced nephropathy is about 2% and can be prevented by evaluation of glomerular filtration rate (GFR) and hydration of patients with borderline GFR (8).
3.3. Classification of Lesions
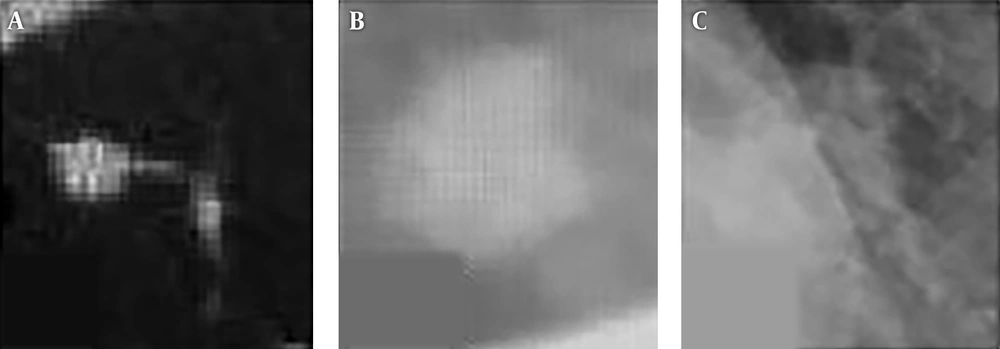
A benign nodule was defined as a small uncalcified nodule showing no changes when compared with the prior CT (9). An indeterminate nodule is defined as a nodule that shows no calcification and was less than 5 mm in size when a prior CCT is not available (10). A suspicious nodule is defined as having a smooth margin, monogonal shape and diffuse scattered distribution (11) (Figure 1).
3.4. Statistical Analysis
Descriptive statistics were used to summarize the variables. The variables recorded included age, gender, CXR and CCT findings, paraaortic lymphadenopathy and liver metastasis. Linear regression was used to correlate the liver metastases, paraaortic lymphadenopathy and pulmonary metastases. IBM SPSS Statistics for Windows version 24.0 (IBM Corp. Released 2016, Armonk, NY: IBM Corp) was used for analysis. A P value of less than 0.05 was considered statistically significant. The data was expressed as mean and percentile. The Cohen kappa test was used for agreement between CXR and CCT. The McNemar test was used to compare the sensitivity, specificity and accuracy of the chest CT group and the CXR group in comparison with pathology.
4. Results
4.1. CCT and CXR
Of the 377 patients enrolled in this study, 59.7% of patients were male and 40.3% of patients were female. Patients with colon cancer were more prevalent (65% vs. 35%) than those with rectal cancer and had higher staging according to TNM scoring (P < 0.01). The distribution of TNM staging in colorectal patients was 3 (8%) patients for stage 1, 94 (24.9%) patients for stage 2, 91 (24.1%) patients for stage 3 and 189 (50.1%) for stage 4.
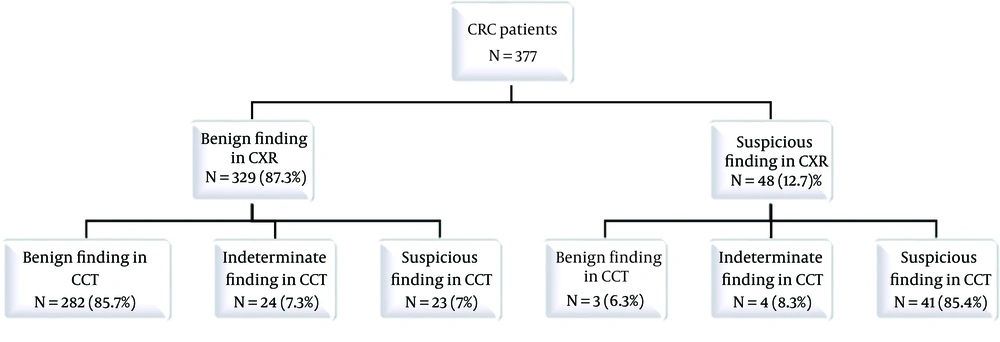
Their demographic characteristics are shown in Table 1. In the CXR group, 329 (87.35%) of patients were diagnosed as having normal or benign findings and 48 (12.7%) of patients showed suspicious nodules. In the chest CT group, 285 (76%) of patients were normal/benign nodules, 28 (7%) had indeterminate nodules and 64 (17%) had suspicious nodules (Figure 2). Patients who had pulmonary metastases on the pre-operative chest CT underwent diagnosis (Table 2).
| Variable | No. (%) |
|---|---|
| Age | |
| Mean | 57 |
| Median | 58 |
| Range | 17 - 91 |
| Gender | |
| Male: Female | 1.48: 1.0 |
| Location | |
| Rectum | 132 (35) |
| Colon | 245 (65) |
| AJCC stage based on TNM | |
| 1 | 3 (0.8) |
| 2 | 94 (24.9) |
| 3 | 91 (24.1) |
| 4 | 189 (50.1) |
| Liver metastases | |
| Yes | 139 (36.9) |
| No | 238 (63.1) |
| Paraaortic adenopathy | |
| Yes | 73 (19.4) |
| No | 304 (80.6) |
Abbreviations: AJCC, American joint committee on cancer; CRC, colorectal cancer; TNM, tumor, node, metastasis
| Patients (N = 59) | |
|---|---|
| CT guided biopsy | 17 |
| Bronchoscopy | 7 |
| Thoracotomy | 3 |
| Routinely followed-up with chemotherapy | 25 |
| Expired before diagnostic procedure | 7 |
4.2. Comparison Between CCT and CXR
The measure of agreement between CXR and CCT was good (0.64, P < 0.01) (95% confidence interval (CI) = 0.58 - 0.69). Detecting malignant lesions by CCT was higher than CXR since the sensitivity of the chest CT group was 96.2% and that of the CXR group was 76.9% in comparison with pathology. The accuracy was 96.2% in the chest CT group and 85.9% in the CXR group. There was no difference in specificity between groups (96.2% vs. 95%). There was moderate agreement between TNM staging and rate of malignant nodules in the CCT group (0.50, P < 0.01) (95% CI = 0.492 - 0.508).
Among these patients, 21 (5.5%) had isolated pulmonary metastases, 40 (10.6%) had simultaneous hepatic metastases and 35 (9.2%) had extra pulmonary and hepatic seeding. Significant discrepancy was detected in the incidence of isolated hepatic metastasis between the colon and rectal group (P < 0.01). On logistic regression analysis, liver metastasis could increase the risk of pulmonary metastasis in colon (P = 0.02) and rectal cancer (P < 0.01), but there was no correlation between paraaortic lymphadenopathy and lung involvement in colon (P = 0.69) and rectal cancer (P = 0.90).
5. Discussion
Most guidelines agree that the chest should be imaged for staging of CRC, but there is disagreement about the exact type of imaging modality (11). The National Comprehensive Cancer Network has recommended CT rather than plain film radiographic imaging of the chest (12). The main reason for the use of CT for staging is early diagnosis of pulmonary metastases with high sensitivity of 51% to 73% and specificities of up to 74%, which increases the rate of resection of pulmonary metastasis (4, 11). CCT is competent for identifying nodules of 2 - 3 mm, whereas CXR identifies lesions 5-10 mm in size (13). Early detection and resection of pulmonary metastases from CRCs may result in 5-year survival rates above 50% in carefully selected patients (7).
Some studies have argued that routine CCT should not be a part of preoperative staging because pulmonary metastasis has a low incidence and CCT occasionally influences the treatment plan and has a risk of radiation exposure (7, 13, 14). In addition, an indeterminate nodule can change pulmonary staging, but does significantly effect on patient’s clinical course (11). The low positive yield and low positive predictive value of CCT when healing with a negative CXR brings the usefulness of routine CCT under question (15). In this research, although CXR did not reveal any pulmonary metastatic lesions in 23 (7%) patients, the measure of agreement between CXR and CCT was good (0.64, P < 0.01) and CCT changed TNM staging in only eight (2%) patients.
One main problem of staging with chest CTs is in the finding of indeterminate lesions which have a low risk of malignancy (10%-20%) and are usually difficult to determine (7, 11). Small nodules are often seen on chest CTs and are usually benign (7). The number of indeterminate lesions in this study was 17%, while most studies estimate it about 20% - 30%. Heterogeneity in studies and the lack of agreement in the definition of ILL confirms this (4). Radiologist experience and improvements in scanning technologies will increase the identifying such lesions (16). A small proportion of indeterminate lung lesions develop into definite metastases (< 30%), mostly in node positive disease. This is a clue not to delay treatment of indeterminate lung lesions (17, 18).
Kim et al. reported that lymph node involvement is a risk factor for pulmonary metastatic disease and concluded that, without involvement of the liver or lymph node, a chest CT should not be routinely suggested (13). However, this study demonstrated no correlation between paraaortic lymphadenopathy and lung involvement. According to the data of this research, liver metastasis and a high American joint committee on cancer (AJCC) stage base on the TNM increases the risk of pulmonary metastasis.
In conclusion, although this study was limited by the short-term follow-up, our results suggest that CCT for preoperative staging in CRC patients, especially at stages 3 and 4 in TNM staging and for liver metastases. Further studies to evaluate the effect of CCT findings on long term surveillance and its cost benefit are recommended.