1. Background
Pilonidal disease is one of the most prevalent surgical problems that involve mostly young patients in their active years of life. This condition was originally thought to be congenital but is now believed to be acquired, in accordance with the theories of Karydakis and Bascom (1). The pathological process is believed to be insertion of hairs into subcutaneous tissue and the resultant chronic foreign body reaction (1), and its most prevalent anatomical location is the sacral region. Pilonidal disease has two main clinical features: pus-draining fistulas or abscess with or without prior fistula. The diagnosis is clinical and by detecting fistula or abscess formation in the sacral area (2, 3). The main problem is patients that are referred with unknown pain or suspicious asymptomatic orifices in the sacral region. Abscess formation with no prior problem, and our experience of asymptomatic sacrococcygeal sinuses, lead us to suggest that pilonidal disease may be asymptomatic before classical presentation. Further, in some patients with unexplained pain in the sacral region, pilonidal disease may be the main cause. Diagnosis of unclear stages of pilonidal disease seems to be confounded by a lack of standardized diagnostic tools for the disease.
2. Objectives
There is a shortage of studies on imaging tools (4, 5) for its accurate diagnosis. Such tools could be beneficial in patients suspected of having pilonidal disease or in those requiring confirmation of recurrence. In this study we tried to evaluate diagnostic power of ultrasonography for clinically diagnosed pilonidal disease patients since we assume that they share a common pathology with asymptomatic and recurrent disease.
3. Patients and Methods
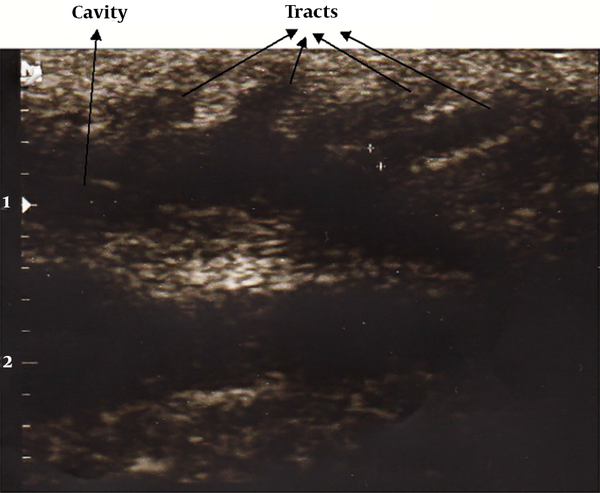
This was a diagnostic study in a group of patients with confirmed pilonidal sinus and a control group without any sign of the disease. The inclusion criterion for the patient group was obvious pilonidal sinuses in the sacrococcygeal area confirmed by an experienced surgeon (sign of visible sinus orifices and discharge from them). Exclusion criteria were: presence of abscess in the inter-gluteal region; any infection or cellulitis in the mentioned area; any congenital malformation in the sacral region; prior pilonidal sinus surgery; recurrent disease and final pathologic results other than pilonidal disease. The control group was selected from age- and sex-matched patients who were admitted to the same hospital for another surgical problem not related to the sacral region. After obtaining written informed consent, all the patients in both groups underwent superficial tissue sonography with a linear 10 - 12-MHz ultrasound probe. The sonographer was completely blind to the involvement of the patient, but to ensure the blindness, an ultrasonography gel mixed with methylene blue was applied to the sacral area by another team member. The variables recorded by ultrasonography were: presence of tracts in subcutaneous tissue; number of tracts; presence of cavities in the sacral area; two-dimensional size of cavities; and presence of hair in the cavities or tracts. Detection of subcutaneous tracts or cavities with or without hair inside them was taken as a positive result for pilonidal disease involvement. Excision of pilonidal sinus with or without repair was performed for all patients in the pilonidal sinus group and the resected tissue was sent for pathologic examination for confirmation of diagnosis. Study design was conducted based on STARD checklist. The study was confirmed by Tehran University of Medical Sciences ethics committee.
4. Results
The pilonidal disease group comprised 50 patients (42 male, 8 female), with a mean age of 26 ± 6.7 years (range: 16 - 44 years). Similarly the control group consisted of 50 cases (36 male, 14 female), with mean age of 28.9 ± 8.9 years (range: 14 - 57). Ultrasonography detected pilonidal disease in 48 of the 50 patients with confirmed pilonidal sinus (sensitivity = 96%; 95% confidence interval [CI]: 0.86 - 1.00). All 50 patients without signs of pilonidal disease were diagnosed as disease free by ultrasonography (specificity = 100%; 95% CI: 0.93 - 1). Positive predictive value of test was estimated to be 100% (95% CI: 0.93 - 1.00) and negative predictive value was 96% (95% CI: 0.87 - 1.00).
Indeed, based on statistical analysis the likelihood ratio of positive and negative tests were 48.96 (95% CI: 7.03 - 341.20) and 25.0 (95% CI: 6.43 - 97.20) respectively. Ultrasonography detected sinus tracts in 36 (72%) patients with pilonidal disease, among whom 20 patients had one tract, 12 had two tracts and 4 had three tracts. Hairs were detected in 32% of the patients (Figure 1). Subcutaneous cavities were detected in 96% of the patients, with a mean size of 284.5 ± 305 mm² (range: 15 - 1200 mm2) (Figure 1). Pathologic examination of the resected tissue confirmed pilonidal disease in all of patients who underwent surgery.
5. Discussion
After a long history of debate, there is now a consensus among experts about the acquired nature of pilonidal sinus disease (1). The most accepted theory of the pathology of pilonidal disease is that of Karydakis (1). According to this theory, hairs enter the subcutaneous tissue through a tract and make a cavity, which results from foreign body reaction, and another tract leads to expulsion of the hair from the cavity. None of these features is mandatory for the pathological diagnosis of pilonidal disease. Standardization of paraclinical tools for diagnosis of this disease have continually been ignored because of the ease of clinical diagnosis. Yet pilonidal disease in fact may not exhibit typical presentation at some stages during its course. This is demonstrated by sudden presentation of abscess without previous signs of the disease, and patients with clear evidence of sinus tracts upon examination and imaging without clinical symptoms. Indeed some patients have unaccountable sacral pain that may be caused by primary stages of pilonidal disease, and some have suspicious signs of recurrence after previous surgery. Making a definite diagnosis in these patients is only possible by paraclinical means. Only a few investigations have focused on imaging tools for diagnosis of pilonidal disease but none have used ultrasonography especially for this purpose (4, 5) and most researchers have focused on therapeutic procedures for the disease (6-10).
Ultrasonography findings among patients with clinically obvious pilonidal sinus support this theory that there is not uniform structural findings among patients presenting with this disease. Most of them had detectable cavities in the imaging but tracts were not a constant finding among them. This may be explained by pathologic nature of disease that some tracts may be closed after cavity formation but the cavity and other tracts remain and produce the related symptoms (7).
The excellent sensitivity and specificity of ultrasonography for diagnosis of pilonidal disease in the present study with clinically evident cases, make this method a useful diagnostic tool even in complicated or unclear cases since there is no difference in pathologic mechanisms of disease between these two categories. On the other hand, based on our results, ultrasonography is able to detect cavities and tracts with a powerful resolution that is very helpful for surgeons in mapping the lesions before the surgery and intraoperatively. As with other diagnostic applications of ultrasonography, this particular application will require operators to acquire sufficient experience before they can diagnose pilonidal disease.
One important limitation in our study is the patient selection method. In a diagnostic test study, we should include the patients based on a suspicious clinical scenario that is aimed to be diagnosed; then, the group will undergo the under study test and gold standard. Finally, some patients will be positive for disease and some will be negative. Here we have enrolled clinically obvious patients in the case group and healthy subjects as control group. This design will falsely increase the diagnostic indices. In our study, as the percentage of clinically suspicious patients for pilonidal disease is very low, we couldn’t wait for enrolment of only suspicious patients. Future studies on clinically suspicious patients will better determine the diagnostic indices of ultrasonography for diagnosis of pilonidal disease and determining of its anatomical characteristics.