1. Introduction
Uterine cavernous hemangioma is an extremely rare vascular tumor with less than 60 reported cases since 1897 that was described for the first time. They can be congenital in association with congenital disease including Kasabach-Merritt syndrome, hereditary hemorrhagic telangiectasia, Maffucci syndrome, Klippel-Trénaunay syndrome and, tuberous sclerosis (1) or acquired which is more common and probably due to hormonal or physical changes (2). Although the prevalence of these tumors is not clear among pregnant and non-pregnant women, they have been reported more commonly during pregnancy. This could be related to hormonal alterations and physical changes in the uterine during this period, which causes more symptoms. The definitive diagnosis of uterine hemangioma is by histologic examination. Neither clinical symptoms nor imaging findings could give a discrete diagnosis. Although in most cases ultrasonography is the first modality to evaluate the pelvic abnormalities, magnetic resonance imaging (MRI) could give more information before surgery. However, there is limited data about uterine hemangioma MRI features. To our knowledge, there is only one other study that focuses on the magnetic resonance features of the uterine cavernous hemangioma (3). Here we describe the MRI findings of a uterine hemangioma that was primarily misdiagnosed as uterine sarcoma.
2. Case Presentation
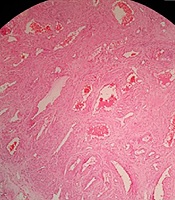
The patient was a 40-year-old premenopausal woman who presented with abnormal uterine bleeding (AUB) as menometrorrhagia for the past several months. A cervical polyp was found in the physical exam and was resected. The pathology revealed adenocarcinoma in situ (AIS). Cervical and uterine parameters were normal in the physical exam. Laboratory findings only demonstrated mild anemia. The ultrasound examination only reported some small uterine fibromas and global enlargement of myometrium without any changes in its echogenicity, calcification or focal lesion. Then the patient underwent MRI with a 1.5T system (General electric medical system, USA), using an 8-channel coil. The MRI revealed a large mass in the upper portion of the endocervical canal with invasion into the myometrium and uterine serosa was reported compatible with cervical adenocarcinoma. Then the MRI was reviewed again by a second radiologist with a specialty in gyneco-oncology. The second opinion was a circumferential edematous change (high T2 signal) in the lower half of the myometrium which extended to the serosa and upper endocervical canal and resulted in the lobulated uterine serosal surface. This region showed no hemorrhage on T1 weighted images and showed enhancement similar to myometrium but with only mild restriction in diffusion-weighted imaging (DWI). Multiple low signal strands from the inner myometrium to serosa on T2 weighted, and postcontrast images were detected. Endometrial cavity, cervical stroma and serosa were normal. According to all findings, a low-grade sarcoma was proposed (Figure 1).
A 40-year-old woman with abnormal uterine bleeding for several months. MRI shows diffuse involvement of the lower uterine segment by cavernous hemangioma. In coronal (A), axial (B) and sagittal (C) T2 weighted images, the lesion shows high T2 signal that results in lobulated uterine contour (white arrows). T1 weighted image shows no hemorrhage (D). Diffusion-weighted imaging (DWI) (E) and apparent diffusion coefficient (ADC) map (F) show mild restriction. Post contrast images (G,H) show significant enhancement and linear low signal strands in the lesion (black arrows).
The patient underwent a total abdominal hysterectomy, which was sent for frozen section study. No cervical lesion was found in macroscopic and microscopic examination of the entirely submitted cervix but on gross inspection, an elevated lesion with relatively soft consistency measuring 1.5 × 1 cm in area and 0.3 cm in height was seen in the upper portion of the endocervical canal-lower uterine segment which was reported in frozen section study as vascular lesion/hemangioma (Figure 2A). After fixation, additional sections were prepared from the endomyometrium. In microscopic examination, a view of large irregular vascular channels filled by erythrocytes and fibrin, with infiltration between myometrium up to subserosa was noted (Figure 2B and C) and the cavernous hemangioma was confirmed by the permanent pathology result.
3. Discussion
Uterus cavernous hemangioma is a rare disease with a wide range of differential diagnosis including arteriovenous (AV) malformation, angiomyoma, and hemangioendothelioma (1). Also, there is a case report which suggests similarities of imaging between cavernous hemangioma and degenerated myoma (3). This entity sometimes presents as a uterine mass and sometimes involves myometrium diffusely. Although other studies have reported cases of uterine and cervical cavernous hemangioma, the data about the imaging finding and role of imaging in preoperative diagnosis is still unclear. Due to its rarity, a high clinical suspicion is needed to think about the disease before pathologic findings.
As usual, it is believed that cavernous hemangioma in other parts of the body including the liver, intracranial, and intraosseous are isointense or hypointense on T1 weighted and isointense to hyperintense on T2 weighted MRI depending on the amount of venous stasis in the lesion. They have high signal intensity after contrast enhancement (4-6). Obviously, calcification, hemorrhage and necrosis can alter the signals.
Almost always ultrasound is the first modality of imaging in gynecological problems. Careful examination during ultrasound may show a thickened uterine wall with hypoechoic space. Color Doppler imaging usually demonstrates low-velocity flow, or no obvious flow within these spaces. These sonographic features have been specifically described by three case reports with diffuse cavernous hemangioma of the myometrium during pregnancy (7-9).
Kobayashi et al. described CT findings of uterine cavernous hemangioma in a 19-year-old woman as a 10 cm mass with numerous small calcifications (3). They found that in T2 weighted images, high-signal intensity with focal areas of low-signal intensity could be seen, which in contrast medium on T1 showed poor enhancement (3). In another study, Lee et al. described a case of cervical cavernous hemangioma mimicking degenerated fibroma. In contrast to the study conducted by Kobayashi et al. (3), there was no specific imaging characteristic for cavernous hemangioma due to multiple calcifications and massive hemorrhages within the mass. Non-enhanced CT only helped to detect the small size of calcifications. Hemorrhage could be seen as hyperintensity on T1 and hypointensity on T2 weighted images. Whereas, the heterogeneous high-signal intensities on T1 and T2 weighted images were interpreted as extensive necrosis. Sagittal T2 weighted images showed a beak-like mass arising from the anterior wall of the uterus (10). Probable characteristic findings in these three cases were calcification, necrosis, and hemorrhage, which can be seen in degenerated myoma and leiomyosarcoma that put these two entities in the differential diagnosis of cavernous hemangioma.
Our case presented as diffuse enlargement of most of the myometrium that extended to the serosa and resulted in the lobulated border of uterine contour with high T2 signal and significant enhancement similar to the myometrium. Because of the pathology report of AIS in the resected cervical polyp, these MRI features were first misdiagnosed as cervical cancer with myometrial and para-uterine invasion. However, regarding normal hysteroscopic and physical exam, no hypoechoic space in the ultrasound exam (which is typical for hemangioma), and a normal cervical stroma and parametrium in MRI, the second radiologist’s opinion was a diffuse myometrial pathology as sarcoma. Although the features were not typical, based on only mild restriction of the lesion in DWI and the mentioned feature, low-grade sarcoma was proposed.
Leiomyosarcoma, as the most common uterine sarcoma, may present as a massive mass with rapid enlargement and an irregular border. The mass shows high to intermediate signal intensity on T2-weighted images, with hyperintense hemorrhagic changes on T1-weighted fat-suppressed images. On DWI, uterine leiomyosarcoma shows restricted diffusion (unlike our case) (11). Nodular borders, hemorrhage, “T2 dark” areas, and central unenhanced areas are suggested as a differentiating feature of leiomyosarcoma from atypical leiomyomas (12).
MRI features of degenerated leiomyoma depend on the degree of hyaline degeneration, myxoid portions, calcification, fatty, cystic, or hemorrhagic components of the tumor. Calcified or hyaline degeneration shows hypointensity on T1- and T2-weighted images. On the other hand, myxoid and cystic degeneration shows high signal intensity on T2-weighted images with minimal and no enhancement, respectively. Red degenerative leiomyomas have heterogeneous hyperintensity on T1- and T2- weighted images (11).
In conclusion, we reported a case of uterine cavernous hemangioma with no typical imaging feature of this pathology that has ever been reported and was misdiagnosed as low-grade sarcoma. The present case highlights additional imaging features of this pathology that should be kept in mind as diffuse involvement of uterine myometrium with a lobulated border of uterine contour, an edematous signal in MRI, without endometrial involvement and mild restriction in DWI. Although the case did not have any hypoechoic areas in the ultrasound exam, multiple scattered linear low signal strands in the lesion in MRI could be a feature of diffuse cavernous hemangioma. More numbers of cases are needed to evaluate the specificity of this finding in future research.

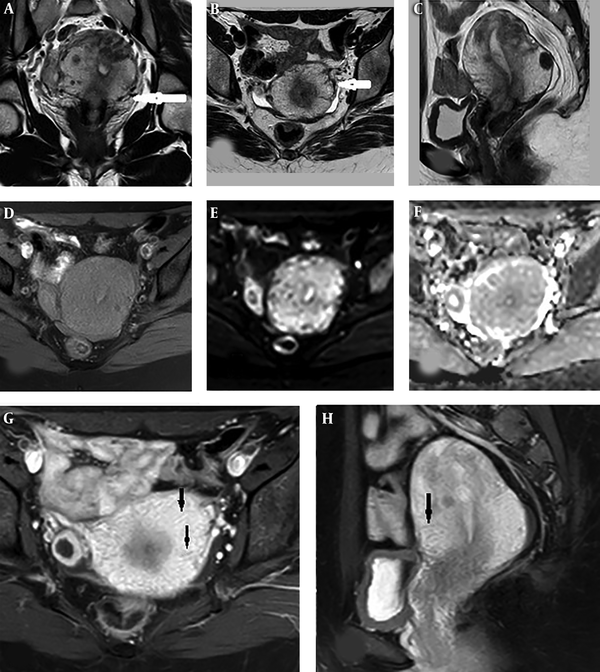
![A, Irregularly shaped vascular spaces [hematoxylin-eosin stain (magnification, ×10)]. B and C, Dilated irregular vascular channels, filled by erythrocytes and fibrin, with infiltrating between myometrium [hematoxylin-eosin stain, (magnification B: ×10. C: ×40)] A, Irregularly shaped vascular spaces [hematoxylin-eosin stain (magnification, ×10)]. B and C, Dilated irregular vascular channels, filled by erythrocytes and fibrin, with infiltrating between myometrium [hematoxylin-eosin stain, (magnification B: ×10. C: ×40)]](https://services.brieflands.com/cdn/serve/31518/17e21fbcd1172612e74a559fa8c460440d6102b7/iranjradiol-17-3-99416-i002-preview.png)