1. Introduction
Pericardial cysts are rare. These uncommon benign congenital anomalies are located in the middle mediastinum. The estimated incidence is 1:100,000. Their diameter is usually from 1 - 5 cm (1). These benign cysts are located at the right cardiophrenic angle in 70% of cases, left cardiophrenic angle in 22% of cases and rarely in the posterior or anterior superior part of the mediastinum in 8% of cases (2). Most of pericardial cysts (> 50%) are asymptomatic (1, 3) and have a benign natural course. Some cysts have symptoms such as dyspnea, chest pain, or persistent cough. Hemoptysis, fever, and pneumothorax (3) are unusual presentations. Although it occasionally presents with symptoms related to compression of adjacent structures, pericardial cysts usually have no symptoms and are almost always diagnosed incidentally.
In this case report, we describe a patient with a pericardial cyst. Presentation and the course of illness were unusual and the cyst was one of the largest cysts that has been reported to date. Pericardial cysts are not common and giant pericardial cysts are rare and only data of 12 cases were available from 2000 to 2014 in PubMed, and we will review available published articles in the literature. With improvement of technology and CT scan we are able to diagnose this benign congenital anomaly before surgery.
2. Case Presentation
A 24-year-old man presented to the emergency department with dyspnea and persistent cough. In physical exam, no abnormality was found. His past medical history was normal. Such an episode occasionally presented in the past year. There was no recent weight loss, cough, sputum production, exposure to tuberculosis, joint pain, or rash. The electrocardiogram (ECG) was normal.
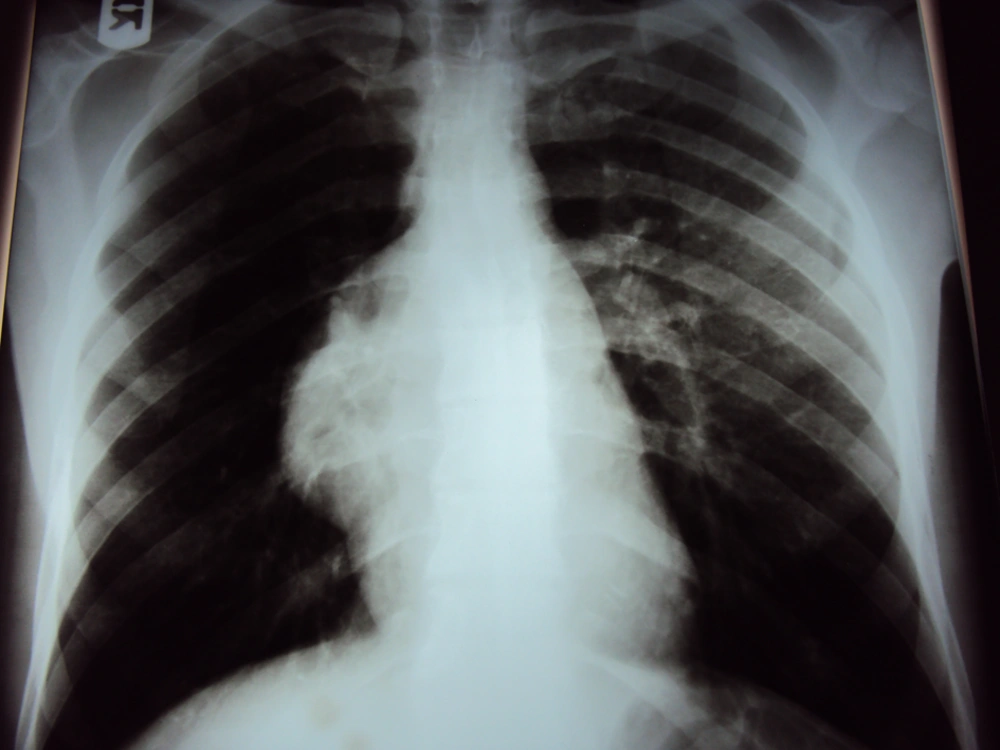
Chest X-ray showed a large opacity obscuring the right heart border (Figure 1). His trans-thoracic echocardiogram showed an echo-lucent space next to the right atrium at the right cardiophrenic angle. His echocardiogram was normal, and no pericardial effusion was found. The apical four-chamber view of the transthoracic echocardiogram showed an echolucent space next to the right atrium at the right cardiophrenic angle, consistent with a pericardial cyst. The right and left ventricular chamber size and function were normal, and there was no valvular heart disease
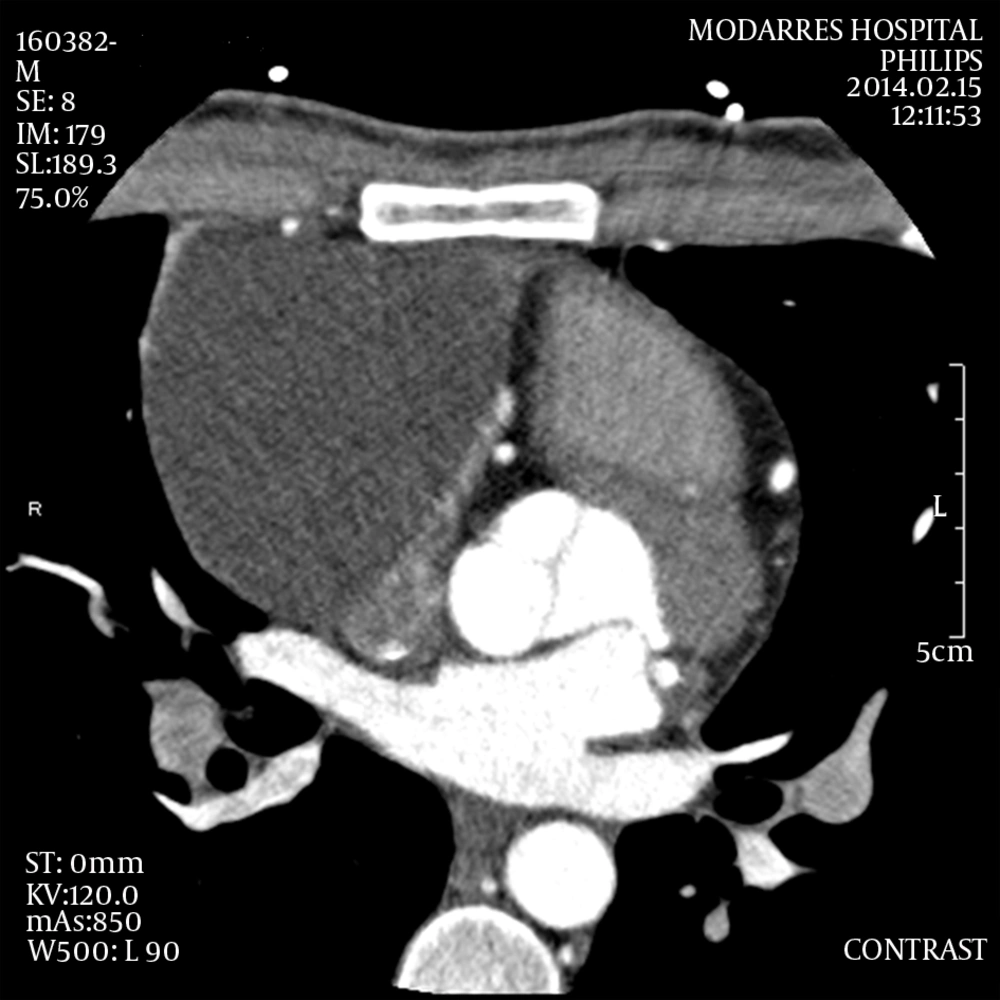
Then computed tomography (CT) was recommended. CT revealed no pleural effusions, and a large fluid collection at the right pericardial border (Figure 2).
Extensive work-up for infectious and inflammatory causes, including blood cultures, viral antibodies, sputum acid fast bacilli’s (AFB), PPD testing, and collagen vascular disease markers was negative.
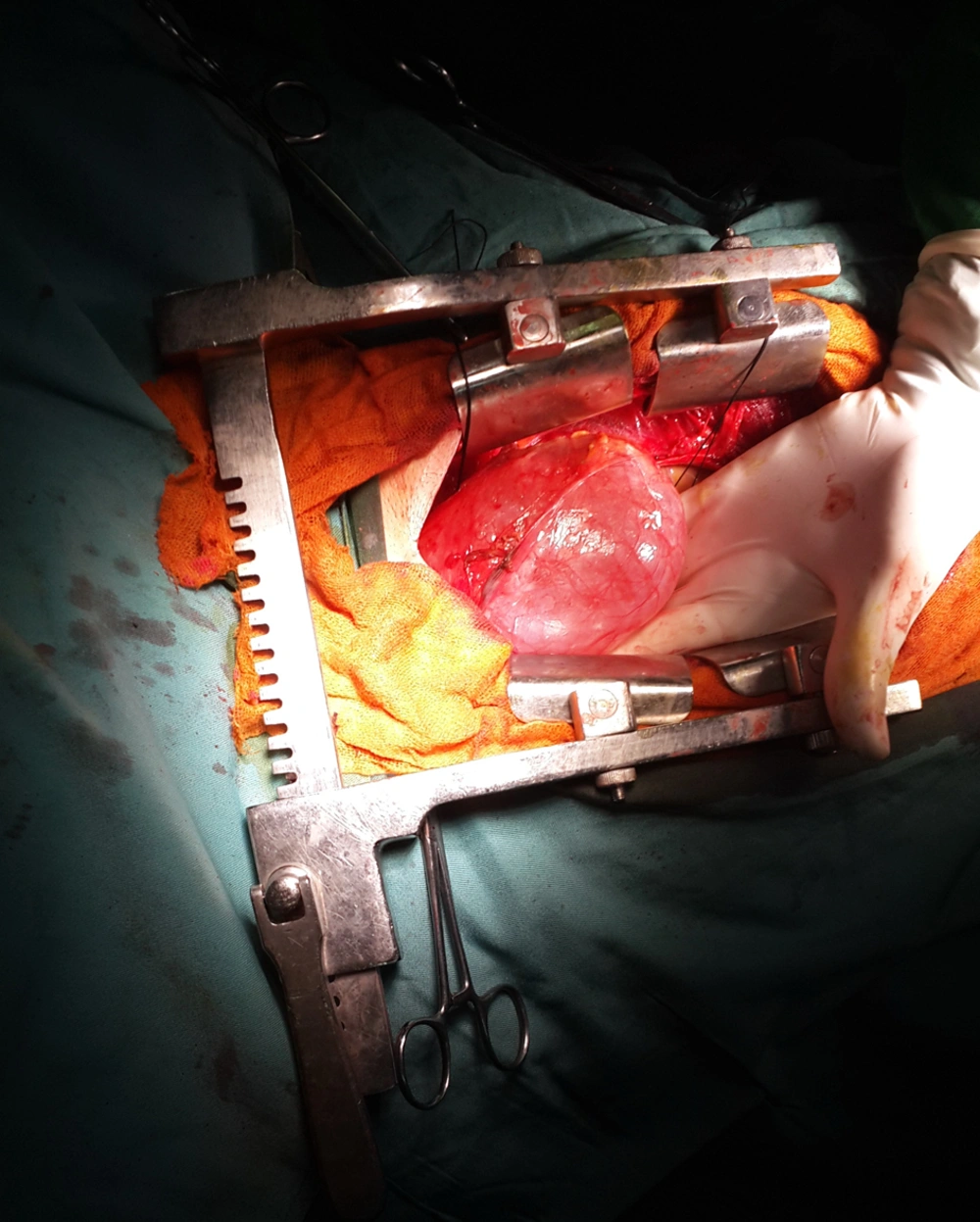
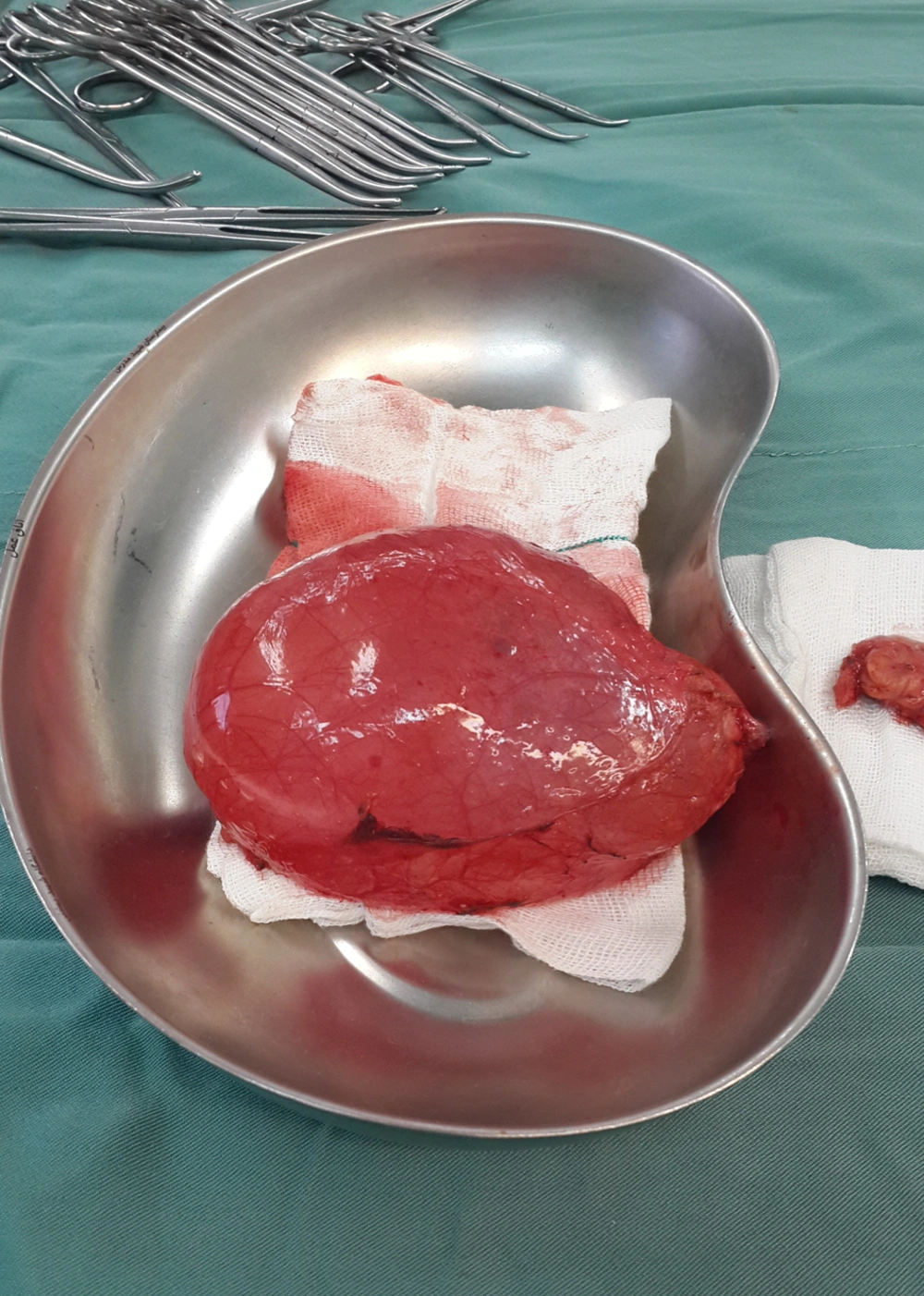
The patient was referred to a cardiac surgeon. After midsternotomy, the pericardium was opened. No fluid or pathologic finding was seen in the pericardium. On the right side and outside the pericardium, a huge pericardial cyst measuring approximately 13 × 8 × 5 cm in diameter was found and totally excised (Figures 3 and 4).
After 5 days, the patient was discharged uneventfully. Pathologic report confirmed the diagnosis. The patient remains symptom-free in the 12 month follow-up visit.
3. Discussion
The incidence of pericardial cysts is about 1 per 100,000 (1). Pericardial cysts are uncommon benign congenital lesions in the middle mediastinum (1, 4).
Most of the masses in the middle mediastinum (61%) are cysts (1, 5). Pericardial cysts and also bronchogenic cysts are the second most common masses after lymphomas (1). Other cysts in the mediastinum are bronchogenic (34%), enteric (12%), thymic and others (21%) (1, 4).
Pericardial cysts (or benign mesothelial cysts), are uncommon lesions that are often found incidentally. There is no sex predilection (6). Their formation may result from failure of fusion of one of the mesenchymal lacunae that form the pericardial sac (6). On histologic examination, the cyst wall is composed of fibrous tissue lined by mesothelium, like normal pericardium, with mild chronic inflammation (6).
Most of them are asymptomatic (50% - 75%) and found incidentally during routine chest X-ray or echocardiography (2). Additional diagnostic methods include trans-thoracic echocardiography, CT scan and magnetic resonance imaging (MRI). The frequency of follow up imaging has not been established yet (7). Contrast-enhanced CT scan has been the modality of choice for diagnosis and follow-up (3). On CT scan, the pericardial cyst is thin-walled, sharply defined, and an oval homogeneous mass. Their attenuation is slightly higher than water density (30 - 40 HU). Pericardial cysts do not enhance with intravenous contrast (7). Pericardial cyst calcification or rupture occurs rarely (4).
The diagnosis usually is suspected following abnormal findings on chest radiography, showing bulging of the right heart border. Additional diagnostic modalities that may find pericardial cysts include transthoracic echocardiography, CT, and MRI of the chest (3, 5, 8).
The age distribution is not well defined. Twenty reported cases of pericardial cysts in literatures presented before the age of eighteen (1), but most of the articles reported older patients.
Pericardial cysts are usually unilocular, smooth, and smaller than 3 cm in diameter (5). Cyst size varies from 2 to 28 cm (1). In our patient, the cyst size was 13 × 8 × 5 cm in diameter that is one of the largest cysts we have found in the literature (9) (Table 1).
| Reference | Publication Year | Age, y | Gender | Size, cm | Location | Presenting Symptom | Treatment |
|---|---|---|---|---|---|---|---|
| Present study | 2015 | 24 | Male | 13 × 8 × 5 | Right side | Dyspnea and persistent cough | Surgical excision with median sternotomy |
| Simsek et al. (10) | 2014 | 28 | Male | 6.4 × 9 | Right side | Fever, sore throat, dry cough, pleuritic chest pain | Conservative management |
| Hamad et al. (11) | 2013 | 30 | Male | 11.2 × 7.4 | Right side | Weight loss(15 Kg), palpitation,chest pain | Surgical treatment |
| Forouzandeh et al. (12) | 2012 | 71 | Female | 8 × 5 | Right side | Dyspnea, cough, fever | Video-assisted thoracoscopic excision |
| Celik et al. (13) | 2012 | 54 | Male | 6.5 × 4.7 | Left side | Acute coronary symptom | Surgical resection and bypass operation(CABG) at the same time |
| Kaklikkaya (9) | 2011 | 39 | Male | 22 × 15 × 7 | Left side | Several episodes of left pleuritic chest pain | Left side thoracotomy |
| Kumar et al. (14) | 2011 | 5 | Male (child) | 10 × 9.5 × 9 | Right side | Chest pain, cough, fever | Surgical excision with median sternotomy |
| Thanneer et al. (15) | 2011 | 22 | Female | 21.5 × 11.4 × 14.2 | Behind the heart in posterior mediastinum | Syncope | Needle aspiration |
| Matono et al. (16) | 2010 | 38 | Male | 12 × 10 | Right side | Asymptomatic and excised because of rapid growing after 20 years | Video-assisted thoracoscopic excision |
| Neizel et al. (17) | 2010 | 59 | Female | Approximately 5 × 5 | intrathoracic mass behind the heart | Atrial flutter and presyncope | Excision with surgery |
| Pereira et al. (18) | 2008 | 73 | Female | 14 × 10 × 7 | Right and anterior and left side of heart | Retrosternal pain | Referred for surgery but was not operated |
| Nina et al. (19) | 2007 | 44 | Female | 13 × 9.5 | Right side | Progressive exertional dyspnea, right side chest pain, dry cough | Right side thoracotomy |
| Dernellis et al. (20) | 2001 | 27 | Female | 15.6 × 12.2 × 5.6 | Right side | Asymptomatic | Surgical removal (the reason for referral for surgery was not mentioned) |
Summary of Published Giant Pericardial Cyst Case Reports
CT scan with contrast has been the diagnostic modality of choice to follow asymptomatic patients with pericardial cysts (1). However, no studies have shown the superiority of contrast CT over MRI and echocardiography for diagnosis or follow-up. On CT scan, pericardial cysts are thin-walled, sharp, oval homogeneous masses. Their attenuation is slightly higher than water density (30 to 40 HU) (2). Their enhancement with intravenous contrast is poor (2).The frequency of follow-up imaging has not been defined.
Management of pericardial cysts depends on their symptom. If the patient is asymptomatic, serial echocardiography is enough, but if the patient is symptomatic or reveals an increase in the size of the cyst or has solid component in the cyst cavity in the serial follow-up,a cyst resection has been the most favored approach [with thoracotomy or sternotomy or video-assisted thoracic surgery (VATS)] (3, 5). Aspiration is another method, but one-third of the patients have shown recurrence.
Non-operative strategy may be selected for high-risk patients. The longest reported follow-up lasted twenty five years. Cyst aspiration is another therapeutic option. One literature review reported that about 30% of the patients had recurrence after percutaneous drainage at three years. Sclerosis has been reported to decrease recurrence rate after aspiration (5).
Morbidity and mortality are low. Surgery has been demonstrated as the only definitive curative treatment (1).