1. Introduction
The World Health Organization defines myxofibrosarcomas as a spectrum of malignant fibroblastic lesions with myxoid stroma that stain positively for vimentin and exhibit a high degree of pleomorphism, and possess a distinctively curvilinear vascular pattern (1). Myxofibrosarcoma is the most common soft tissue sarcoma in the elderly and occurs in the lower extremities (77%), trunk (12%), mediastinum or retroperitoneum (8%). However, myxofibrosarcoma of the head and neck is uncommon with a 2% to 4% incidence (2), and to the best of our knowledge, there is no information in the literature regarding myxofibrosarcoma in the parapharyngeal space. We present a rare myxofibrosarcoma case of the parapharyngeal space.
2. Case Presentation
A 73-year-old man presented with foreign body sensation in the oral cavity and left otalgia for three months. Fine needle aspiration for soft palate swelling was performed at another hospital but revealed only blood on cytology. However, the soft palate swelling subsequently enlarged, and as a result, the patient visited our hospital. Physical examination revealed a non-tender, left soft palate swelling without mucosal color change (Figure 1). Laboratory results were of no diagnostic importance.
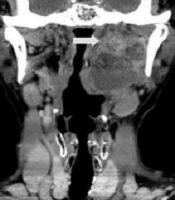
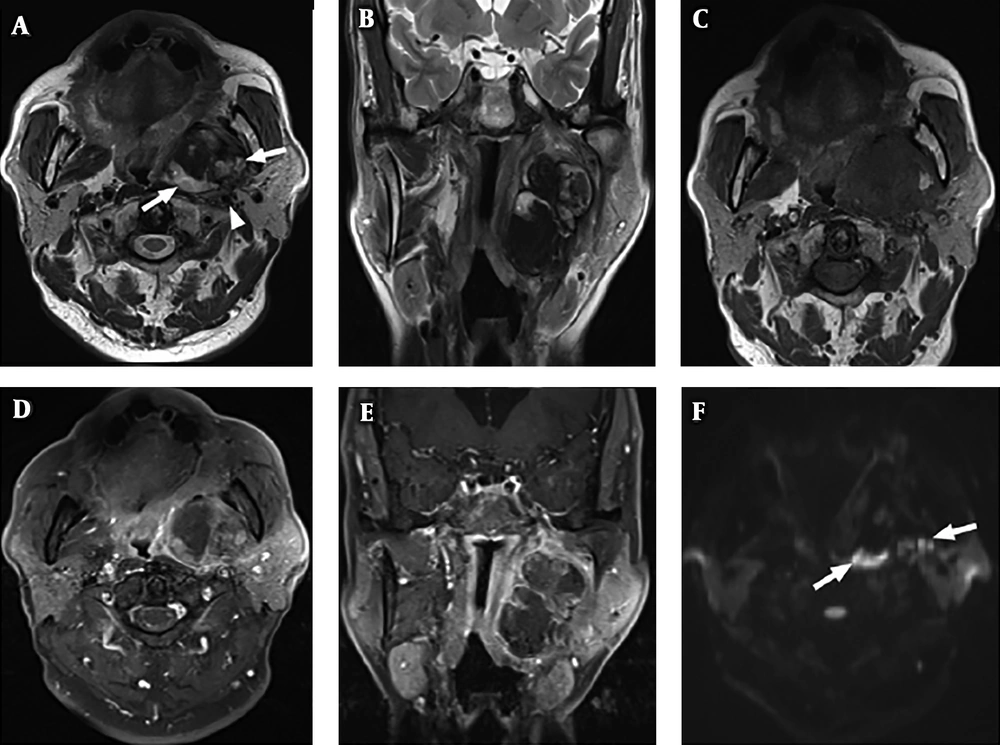
Contrast-enhanced computed tomography (CT) performed to evaluate the soft palate swelling revealed a partially ill-defined, cystic and solid mass in the left parapharyngeal space with a diameter of 4.7 × 3.7 × 6.7 cm (Figure 2). There was no evidence of adjacent bony erosion or destruction. Magnetic resonance imaging (MRI) performed for further evaluation showed that the mass involved the compartment of left parapharyngeal space and masticator space (including medial and lateral pterygoid muscles) with a medially displaced pharyngeal wall. The interface of the lateral aspect of the mass with the parotid gland deep lobe was indistinct. The solid portion of the mass exhibited heterogeneous high signal intensity (SI) on T2-weighted images (T2W images) (Figure 3A and B) that abutted the left internal carotid artery and left internal jugular vein with posterolateral displacement and compromised left internal jugular vein due to a mass effect. The mass showed ISO SI on non-enhanced T1-weighted images (T1W images) (Figure 3C) with heterogeneous enhancement on contrast-enhanced T1W images (Figure 3D and E). In the peripheral enhancing portion of the tumor, subtle diffusion restriction was noted on diffusion weighted images (DWI) (Figure 3F). There was no evidence of lymphadenopathy or distant metastasis. The preoperative differential diagnosis of a prestyloid parapharyngeal mass with T2 high signal intensity and heterogeneous enhancement included parotid gland origin tumor such as pleomorphic adenoma and neurogenic tumor. However, because the peripheral enhancing portion of the mass showed diffusion restriction, the possibility of malignancy could not be ruled out.
Magnetic resonance imaging. A and B, Axial and coronal T2W images demonstrate a heterogeneous high signal intensity mass (arrows) in the left parapharyngeal space. The internal carotid artery (arrowhead) is displaced posterolaterally. C, Non-enhanced axial T1W image shows ISO signal intensity of the mass. D and E, Axial and coronal T1W images with fat suppression after gadolinium administration show heterogeneous enhancement of the mass. F, Diffusion weighted images (DWI) shows diffusion restrictions (arrows) in the peripheral solid portion of the mass.
The patient was planned for complete resection of the mass. He underwent resection of mass via transoral robotic surgery using the da Vinci Xi System (Intuitive Surgical, Sunnyvale, CA) under general anesthesia. The superior and lateral aspects of the mass were located in the masticator space with severe adhesion to the surrounding soft tissues, including the left medial pterygoid muscle. It was difficult to perform complete resection due to severe adhesion to surrounding soft tissues and the complex nature of the space.
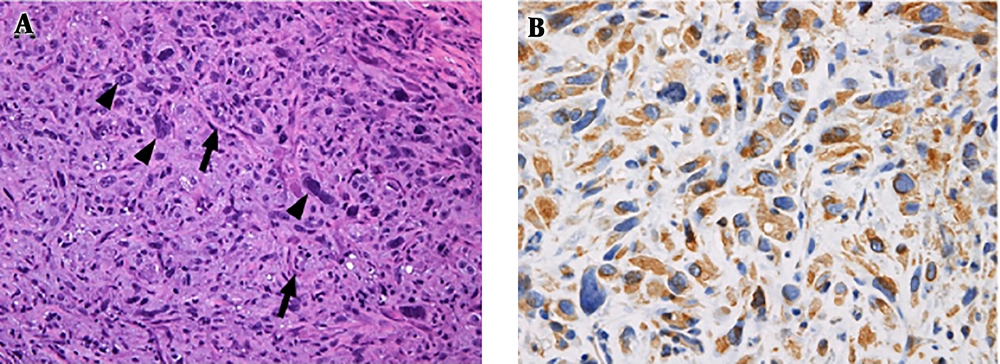
Two specimens of the mass were obtained through the surgery and the specimens grossly demonstrated yellowish white soft tissues, weighed 10.0 and 6.6 grams, and were of dimensions 5.5 × 4.8 × 0.4 cm and 2.5 × 2.2 × 1.6 cm, respectively. Histopathologic examination revealed spindle cell proliferation in a myxoid background, seven mitotic figures per 10 high-power fields (HPFs), abnormal mitosis (Figure 4A), and tumor necrosis of extent > 50 %. The tumor was graded as grade 2 according to the French Federation of Cancer Centers Sarcoma Group (FNCLCC) classification. Immunohistochemistry demonstrated tumor cells were positive for vimentin (Figure 4B) and smooth-muscle antigen (SMA) and weakly positive for epithelial membrane antigen (EMA). The tumor cells were not immunoreactive with desmin or S100, a protein used as a marker for epidermal differentiation. The pathologic diagnosis was myxofibrosarcoma.
A, Histological examination (hematoxylin and eosin stain, × 200) reveals cellular atypia with nuclear pleomorphism (arrowheads). Curvilinear, thin-walled blood vessels (arrows) are prominent in myxoid areas. B, Immunohistochemistry (× 400) demonstrates tumor cells stained positively for vimentin.
Postoperative radiation therapy was planned, but mass recurrence was noted on CT images taken for radiation therapy (RT) planning. Accordingly, reoperation was performed rather than RT. Subsequently, postoperative radiotherapy was administered at a dose of 22 Gy in 11 fractions and 30 Gy in 7 fractions. However, the patient died of disease with loco-regional and distant metastasis five months later.
3. Discussion
Myxofibrosarcoma is a malignant mesenchymal tumor that usually occurs in the trunks or extremities of elderly patients (3), but is uncommon in the head and neck area. The present case was of high grade myxofibrosarcoma according to the FNCLCC classification and occurred in the parapharyngeal space. Although complete tumor resection followed by adjuvant radiotherapy remains the mainstay treatment for myxofibrosarcoma, complete resection of the tumor in this case was difficult due to severe adhesion to surrounding soft tissues and the anatomical complexity of the parapharyngeal space. This cautions tumor origin, location, extent, and anatomical relationships be determined by CT and MRI before surgery to enable decision-making regarding the optimum surgical approach for safe and radical mass removal. The parapharyngeal space can be divided into the pre- and post-styloid compartments, based on the tensor-vascular-styloid fascia (4). The contents of the prestyloid compartment include the minor or ectopic salivary gland, branches of the mandibular division of the trigeminal nerve, internal maxillary artery, ascending pharyngeal artery, and pharyngeal venous plexus, whereas those of the poststyloid compartment include the internal carotid artery, internal jugular vein, cranial nerves IX-XII, cervical sympathetic chain, and glomus bodies (4).
In the present case, posterolateral displacement of the carotid sheath structure indicated the mass arose from the prestyloid parapharyngeal space. Of the various neoplastic lesions encountered in the prestyloid parapharyngeal space, the most common neoplasms are salivary gland origin tumor, predominantly pleomorphic adenoma (5). Pleomorphic adenomas are usually observed as well circumscribed and homogeneous masses with strong enhancement on gadolinium-enhanced T1W images, although larger tumors may be heterogeneous. Usually, these tumors show low to ISO signal intensities (SIs) on T1W images and high SIs on T2W images. Neurogenic tumors are the second-most common neoplasms in the prestyloid parapharyngeal space. Most schwannomas are fairly homogeneous soft tissue masses. However, as with pleomorphic adenoma, necrosis and hemorrhage can occur. Typical schwannomas usually have a target sign (low central and high peripheral SI) on T2W and gadolinium-enhanced T1W images. A solitary parapharyngeal space neurofibroma is rare, representing less than 5% of all parapharyngeal space neoplasm (6), and may show significant fatty degeneration. Rarely, malignant peripheral nerve sheath tumors, soft tissue sarcomas of fatty, muscular, or fibrous origin, and Castleman's disease involve the prestyloid parapharyngeal space. Malignant peripheral nerve sheath tumors usually have the same imaging findings of schwannoma, but rarely, have invasion margins that suggest their invasiveness (7). Rarely, the possibility of soft tissue sarcoma with muscle or parapharyngeal space origin or conglomerated metastatic adenopathy should also be considered. Myxofibrosarcoma exhibits low attenuation on CT images and low to intermediate SI on T1W images. Solid and myxomatous components have high SIs on T2W images and the myxoid component has higher SI (similar to that of fluid) (8). Hyperintense T2-weighted signals in myxofibrosarcoma are due to the high intracellular water contents of myxoid cells. Nodular enhancement is frequently shown in solid components (8). Myxofibrosarcoma frequently displays an infiltrative growth pattern on T2W and gadolinium-enhanced T1W images (9), which distinguishes it from pleomorphic adenoma or schwannoma. Although malignant peripheral nerve sheath tumor also can infiltrate surrounding soft tissues, it usually has a perineural spread growth pattern, which distinguishes it from myxofibrosarcoma in the parapharyngeal space. Clinical features and imaging findings are nonspecific, and rarely in the head and neck area, so accurate preoperative diagnosis may be difficult. However, in case of myxoid tumor with an infiltrative growth pattern in the head and neck space, we can consider the myxofibrosarcoma as a differential diagnosis.
Most patients with a typical benign prestyloid parapharyngeal mass complain of oropharynx foreign body sensation. Of course, this patient also complained of oropharynx discomfort, but he had severe left otalgia. In benign tumors, large size usually compresses surrounding structures and can feel pressure, but it is not easy to involve pain. Therefore, it is necessary to suspect a malignant tumor if the patient accompanies pain. In addition, the cystic lesion of the anteroinferior portion of mass in the image was well dissected from the surrounding tissue. However, the solid mass lesion with an unclear border with the medial pterygoid muscle was not easily dissected during surgery, and a result of frozen biopsy was margin positive. Recurrence also occurred at this site. Image and operative findings were consistent. Therefore, sufficient analysis about image findings was required before surgery. The diagnosis may be challenging, but the identification of tumor origin, location, extent, and anatomical relationships on MR images could be helpful to establish preoperative treatment plans.