1. Context
In addition to the respiratory system, COVID-19 induces damage to the gastrointestinal tract and liver. This damage is more severe in patients with a history of virus infection. In COVID-19 patients, the levels of liver enzymes, including alanine aminotransferase (ALT) and aspartate aminotransferase (AST), change abnormally in the stages of disease progression and acute hepatitis. In addition, hepatotoxicity is more pronounced in patients with severe COVID-19, which can be caused by systemic inflammation, liver damage from medications used to treat COVID-19, or pre-existing chronic liver disease. Previous studies suggest that liver damage associated with COVID-19 is usually rare, and damage to this tissue is secondary to pneumonia resulting from the disease and the length of hospitalization (1-4). Therefore, according to the mentioned explanations, the present mini-review study investigated the effect of COVID-19 on hepatic damages and its cellular mechanism of action.
2. Evidence Acquisition
In this mini-review study, initially, the effect of COVID-19 on liver cells was searched in PubMed without restriction. The language of the assessed articles was English. The related components were searched in the Me SH term system and also used in the two groups of COVID-19 and hepatocytes in combination with each other. Therefore, the search syntax was (“2019 novel coronavirus disease”[tiab] OR “COVID19”[tiab] OR “COVID-19 pandemic”[tiab] OR “SARS-CoV-2 infection”[tiab] OR “COVID-19 virus disease”[tiab] OR “2019 novel coronavirus infection”[tiab] OR “2019-nCoV infection”[tiab] OR “coronavirus disease 2019”[tiab] OR “coronavirus disease-19”[tiab] OR “2019-nCoV disease”[tiab] OR “COVID-19 virus infection”[tiab]) AND (Hepatocytes[tiab] OR Hepatocyte[tiab] OR “Hepatic Cells”[tiab] OR (Cell[tiab] AND Hepatic[tiab]) OR (Cells[tiab] AND Hepatic[tiab]) OR “Hepatic Cell”[tiab]). Ultimately, the selected articles were transferred to EndNote (x7) software and the titles and abstracts of them were assessed by the researcher to remove unrelated articles.
3. Results
3.1. Effect of COVID-19 on Liver Biochemical and Histological Variables
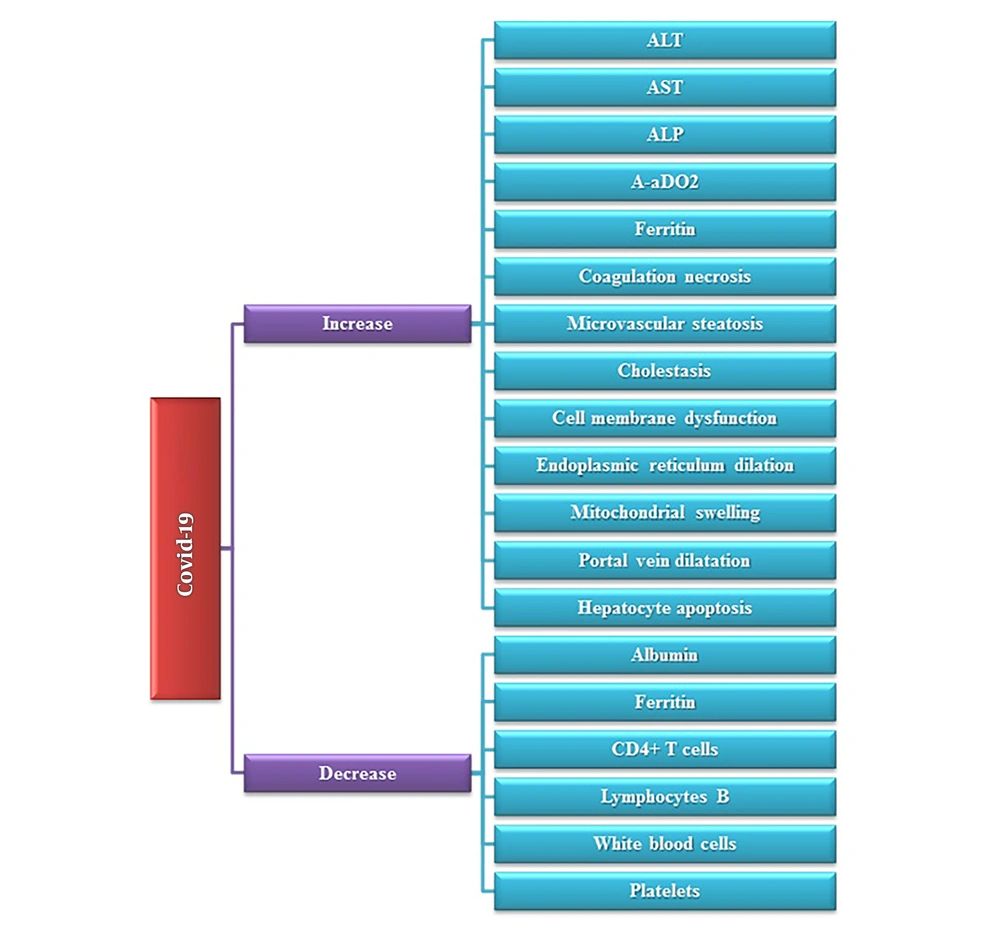
Some studies showed that hepatic AST levels increased in COVID-19 patients admitted to the intensive care unit (ICU) of the hospital. Also, the levels of liver enzymes ALT and AST in patients with COVID-19 increased significantly when compared to the control group. Meanwhile, Alkaline Phosphatase (ALP) had a significant increase in patients with liver damage induced by COVID-19 in a cholestatic assessment study (2). In addition to the increase of these enzymes, some changes in biochemical factors of these individuals, including increased Alveolar-arterial Oxygen Gradient (A-aDO2) and ferritin, or decreased albumin, CD4 + T cells, lymphocytes B, leukopenia (decrease in white blood cells), and thrombocytopenia (decrease in platelets) can be caused by damage to the liver (5, 6). Histologic changes in hepatic tissue caused by COVID-19-induced ischemic injury consist of coagulation necrosis and lymphohistiocytic inflammation of the sinus vein and central vessel endothelium, mild microvesicular steatosis, and duct cholestasis. Activated histocytes, hepatocyte apoptosis, the presence of fibrin microbes in the hepatic sinusoids, extensive dilatation of the portal vein branches, duct thrombosis, port duct fibrosis, and deep vein thrombosis (7-9). Previous studies have shown COVID-19-induced mitochondrial swelling, endoplasmic reticulum dilation, cell membrane dysfunction, and dual or multinucleated cell apoptosis in hepatocytes (Figure 1) (10).
3.2. Factors Affecting Liver Damage Caused by COVID-19
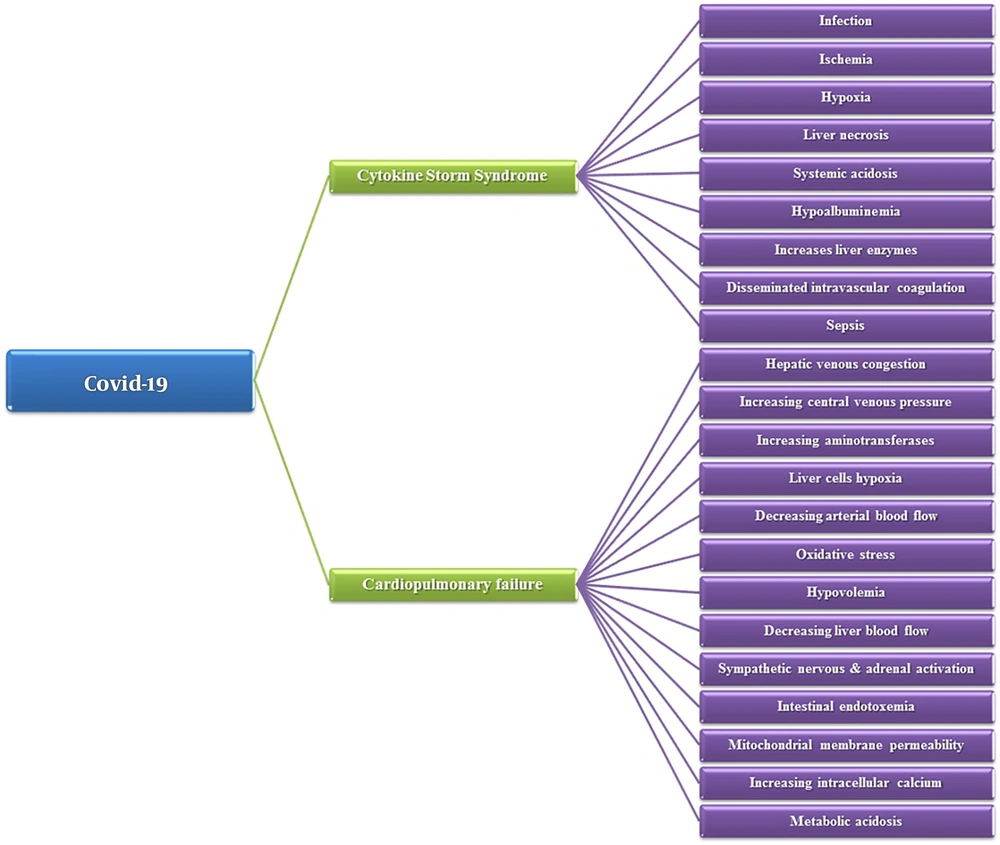
One of the important factors affecting liver damage during COVID-19 is the abnormal coagulation and disruption of fibrinolytic pathways in the blood coagulation process. These disorders occur after the onset of a cytokine storm, inflammation, and toxicity caused by drugs used to treat this disease (1). Cytokine storm syndrome (CSS) is a process in which, pro-inflammatory cytokines increase uncontrollably following the entry of the virus into the cell. In this syndrome, an increase occurs in the levels of interleukins, including IL-6, IL-10, IL-2, and interferon-gamma (IFN-γ), which is directly related to the severity of the disease and the insufficiency of several organs, including the liver. Therefore, instead of protecting the immune system and clearing the body from the virus, this syndrome attacks the immune system uncontrollably, and increased cytokines lead to the exacerbation of infection, ischemia, hypoxia, and necrosis of liver tissue. These disorders are more severe and even more fatal in the elderly due to the greater weakness of the immune system. Moreover, CSS causes disseminated intravascular coagulation (DIC), which induces thrombotic microangiopathy in various organs such as the liver. Another study found that liver damage in COVID-19 could be triggered by a systemic immune response following inflammation, liver ischemia, or hypoxia of liver cells, which ultimately increases liver enzymes and hypoalbuminemia. On the other hand, hypoxia in the liver causes the accumulation of lactic acid in this tissue, and as a result, large amounts of the acid are released into the blood, which upsets the acid-base balance of the body and leads to systemic acidosis in the whole body (3, 11, 12). Another cause of liver damage in COVID-19 is heart failure induced by this disease. In heart failure, systemic arterial pressure suddenly decreases, which leads to decreased hepatic arterial blood flow, hypoxia of liver cells, and increased aminotransferases in this organ. On the other hand, in heart failure, with increasing central venous pressure, hepatic venous congestion, and further predisposes the liver tissue to damage caused by hypoxia were occurred (11). In addition, the oversupply of Kupffer cells, the increase of oxidative stress following hypoxia in the liver, hypovolemia due to cardiopulmonary failure and shock, metabolic acidosis, increased intracellular calcium levels (the most important inducer of cellular apoptosis), changes in mitochondrial membrane permeability, intestinal endotoxemia, and activation of the sympathetic nervous system and adrenal system, which leads to decreased blood flow to the liver, can lead to liver damage during COVID-19 disease. Also, sepsis can be produced by an uncontrolled immune response to infection, cholestasis due to impaired bile metabolism, the toxicity of administered drugs, or inflammation followed by COVID-19-induced liver damage (Figure 2) (13).
3.3. Hepatocellular Mechanism of Action of SARS-CoV-2 in Liver Damage
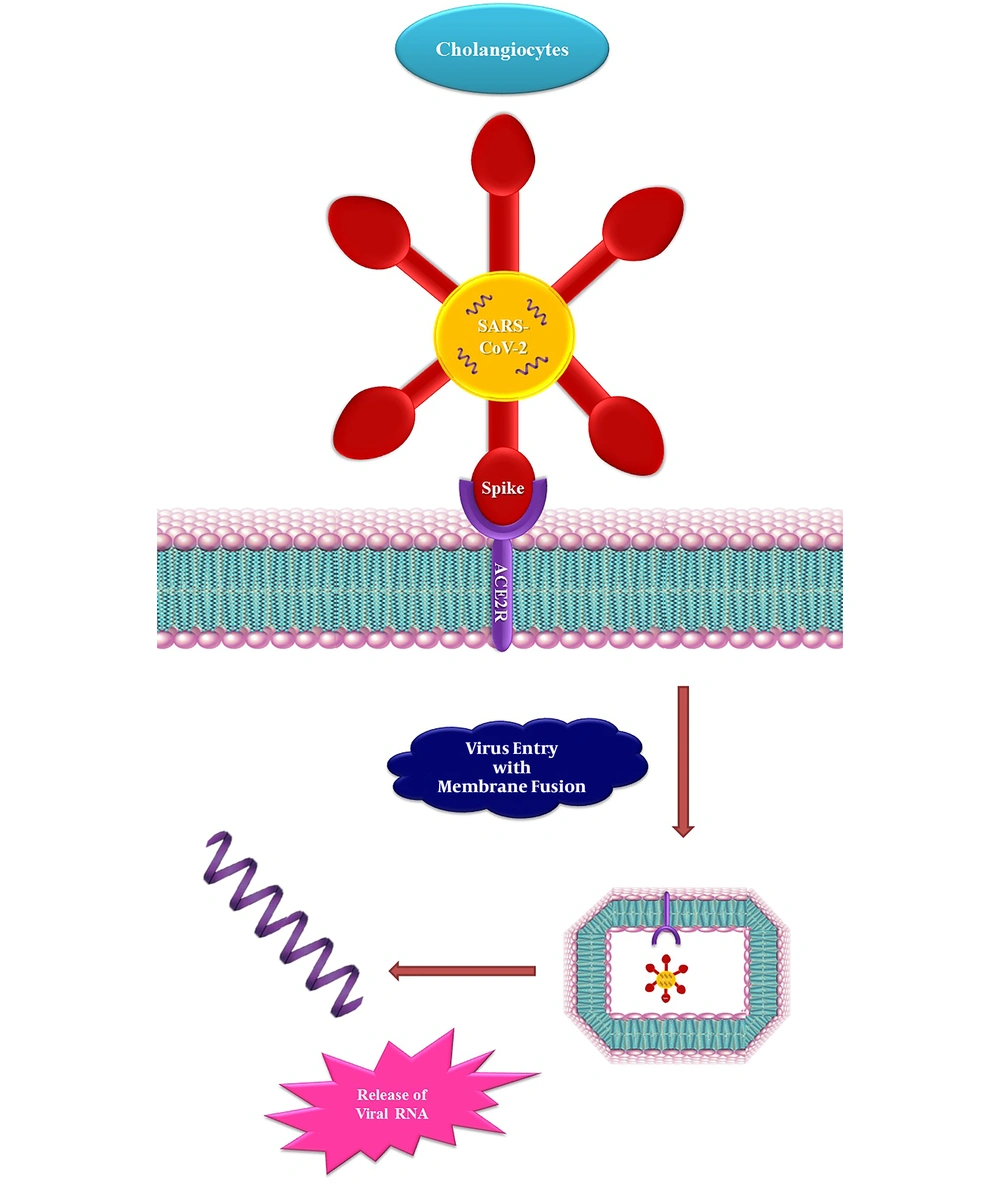
The SARS-CoV-2 virus uses the angiotensin-converting enzyme (ACE2) receptor and membrane proteinase serum (TMPRSS2) to enter the cell (1). This receptor is expressed in bile endothelial cells of the liver, and the SARS-CoV-2 virus can enter these cells and cause damage to them through this receptor. Studies have also shown that the readjustment of ACE2 expression in liver tissue occurs by the compensatory proliferation of hepatocytes from bile duct epithelial cells, followed by hepatic tissue damage resulting from COVID-19 disease (3). Molecular studies have shown that ACE2 receptor expression in collagenocytes increases during infection with SARS-CoV-2. Meanwhile, TMPRSS2 mRNA expression in hepatocytes and cholangiocytes increases by 68% during COVID-19. Thus, ACE2 receptor expression in hepatic endothelial cells is still debated (11, 14, 15). In addition, an immunohistochemical study showed that ACE2 expression is increased in bile duct epithelial cells but not in Kupffer and hepatic endothelial cells. Animal studies also confirm that in mice with acute liver injury, ACE2 expression initially increases but returns to normal after seven days following the compensatory proliferation of bile duct-derived hepatocytes. Thus, SARS-CoV-2 may induce its damage to the liver via the ACE2 receptor on the cholangiocytes (Figure 3) (13).
3.4. Limitation
One of the limitations of this review article is that not all articles were available and they were not free. Also, some articles were written in a language other than English, which required a native translator.
3.5. Future Directions
According to what mentioned in the present study, it can be suggested that future studies focus on the liver and shed light on the mechanisms and pathways of COVID-19 effects on this organ to select effective drugs for the treatment of this disease and use them in clinical studies.
4. Conclusions
In conclusion, COVID-19 leads to liver tissue damage and hepatocyte apoptosis by inducing increased cytokines, ischemia, and hepatic hypoxia following cardiorespiratory failure, coagulation disorders, and intracellular calcium. Moreover, the SARS-CoV-2 virus exerts this effect by binding to and entering through the ACE2 receptor and increasing its expression in cholangiocytes. Therefore, COVID-19 with damage to various parts of liver tissue, including liver sinusoids or Kupffer cells, etc. causes an increase in liver enzymes ALT, AST, ALP, and other factors associated with liver damage, which ultimately leads to hepatotoxicity.