1. Background
Preeclampsia (PE) is one of the main risk factors for maternal mortality (1). It is a specific pregnancy syndrome characterized by systolic blood pressure > 140 mmHg or diastolic blood pressure > 90 mmHg in two measurements at intervals of at least 4 hours, along with proteinuria (urinary protein content of 300 mg or more per 24 hours) and other signs that may occur in the 20th week of pregnancy and last for six weeks after delivery (2, 3). The risk of infant mortality in preeclampsia is four times higher than normal pregnancies. This pregnancy disorder is dangerous and responsible for 15% of preterm births and affects about 5% to 8% of pregnancies. In developing countries, women die every year due to preeclampsia. This disorder is known as the third leading cause of death worldwide and the second most common cause of maternal death in Iran (4-6). Despite extensive studies in recent years, there is no clear cause for the disease, but in some studies, some characteristics of mothers, including age, history of multiple births, history of miscarriage, multiple pregnancies, previous history of preeclampsia, high body mass index (BMI), nullipara, family history, and other factors, such as diabetes, chronic hypertension, coagulation disorders, renal disorders, hypothyroidism, migraine, maternal RH, vasospasm, cardiovascular damages, and inflammatory indices increase the risk of preeclampsia (4, 5, 7). Every year, 50,000 women worldwide die of preeclampsia and its complications. This disease can lead to some complications, such as heart failure, cerebrovascular injuries, acute renal failure, excessive platelet depletion (thrombocytopenia), and hemolysis in the mother, and in the fetus, it can increase the risk of preterm delivery, intrauterine growth restriction (IUGR), low birth weight, thrombocytopenia, and fetal hypoxia and can cause death in severe cases (8-11).
Platelet changes are one of the major changes in blood factors in pregnancy. Normal pregnancy is characterized by an increase in platelet aggregation and a decrease in the number of circulating platelets. Platelet longevity is decreased, and mean platelet volume is increased slightly during pregnancy. Increased platelet intake in placental uterine circulation has been suggested as an explanation for the decrease in circulating platelet count. Increased intake of uterine-placental circulation has been suggested as an explanation for the decrease in circulating platelet count (platelets in pregnancy).
Some studies have shown that platelets play an important role in the pathogenesis of preeclampsia. Preeclampsia increases platelet activity and platelet consumption and, ultimately, thrombocytopenia, which produces younger platelets by increasing the average volume to compensate for them. Therefore, platelet indices may be a way to predict preeclampsia and resolve this dangerous complication (12, 13). Given the importance of the issue and the differences in the results of published studies, it is important to study the platelet indices of pregnant women as a prognosis for preeclampsia. If platelet counts are associated with preeclampsia, platelet counts can be used as a simple, inexpensive, and affordable way to diagnose preeclampsia and prevent many problems by monitoring pregnant mothers.
2. Objectives
The current study aimed to evaluate the platelet parameters in patients with preeclampsia in comparison with healthy pregnant women who were referred to Ganjavian hospital in Dezful city in 2019.
3. Methods
The present study is a case-control and retrospective study. The research samples were healthy pregnant women and those with preeclampsia who were referred to Dr. Ganjavian hospital in Dezful city in 2019. After obtaining the ethical clearance from the Dezful University of Medical Sciences (IR.DUMS.REC.1398.015), the files of pregnant women without and with preeclampsia who gave birth in 2019 in Dr. Ganjavian hospital were examined. Individuals in the case group (files of patients with preeclampsia) were selected as available samples. Individuals in the control group were randomly selected using random number tables due to a large number of available files and increasing the study's accuracy. Criteria for entering the study in the group with preeclampsia were blood pressure ≥ 140/90, proteinuria of more than 300 mg in 24-hour urine or 30 mg consistently in random urine samples, and gestational age over 20 weeks. Exclusion criteria in the group with preeclampsia included any underlying disease, such as diabetes, chronic hypertension, known platelet disorders, multiple birth, and drug use (heparin or aspirin). Women with preeclampsia with BP ≥ 140/90 with proteinuria > 20 weeks gestation were included in the study. The individuals of the control group were also healthy pregnant women with no pregnancy complications and no history of underlying diseases, such as diabetes, chronic hypertension, known platelet disorders, multiple birth, and drug use (heparin or aspirin). Samples studied in both case and control groups were matched in terms of maternal age (women 18 - 35 years old), gestational age (gestational age of 20 - 41 weeks), the number of pregnancies, having a live fetus at the time of hospitalization, and being Iranian. To do this, first, the patient admission offices in the maternity hospital of the mentioned hospital were examined in the desired time interval, and the details of the patients who had the inclusion criteria were recorded then by referring to the hospital archive unit, the required information, including platelet indices of the case group, such as platelet distribution width (PDW), mean platelet volume, and platelet count were extracted from the CBC test in patients’ files, which was done at the beginning of the hospitalization and the information that was not recorded in these files were obtained during contact with them. The files of 104 people in the case group and 104 people in the control group were selected as available samples, and with the criteria for entering the study from those who were referred to the maternity ward of Dr. Ganjavian hospital. Platelets indices, such as mean platelet volume (MPV), platelet count (PC), platelet distribution width (PDW), as well as hematocrit (Hct), hemoglobin (HB), and white blood cell count (WBC) were compared in these two groups, and the results were recorded and reported.
Data were analyzed using SPSS software version 20 and independent t-test and Mann-Whitney U test at a significant level lower than 0.05.
4. Results
In this study, the files of 104 pregnant women with preeclampsia and 104 healthy pregnant women were examined. Individual information of the studied individuals is presented in Table 1. Samples in the two groups did not differ significantly in terms of the mother's age, frequency of pregnancies, and the number of previous pregnancies. Other demographic characteristics of the women studied are listed in Table 1.
| Laboratory Characteristics | Healthy Group (N = 104) | Preeclampsia Group (N = 104) | P-Value |
|---|---|---|---|
| Age | 30.12 ± 1.92 | 30.42 ± 1.42 | 0.274 |
| Frequency of pregnancy | |||
| First pregnancy | 48 (46.15) | 47 (45.20) | 0.346 |
| Second pregnancy or more | 56 (53.85) | 57 (54.80) | |
| Age of pregnancy | 36.21 ± 1.56 | 36.30 ± 1.49 | 0.286 |
| Hemoglobin | 11.91 ± 1.30 | 10.89 ± 1.09 | < 0.0001* |
| WBCs | 13.57 ± 10.74 | 12.55 ± 4.65 | 0.373 |
| Hematocrit | 34.4 ± 26.52 | 35.63 ± 3.21 | 0.013 |
| Platelet count | 284.52 ± 60.58 | 149.30 ± 55.38 | < 0.0001* |
| Mean platelet volume (MPV) | 10.1 ± 79.24 | 12.98 ± 1 .16 | < 0.0001* |
| Platelet distribution width (PDW) | 12.34 ± 2.11 | 15.72 ± 2.52 | < 0.0001* |
Comparison of Laboratory Characteristics of Pregnant Women with Preeclampsia and Healthy Pregnant Women a
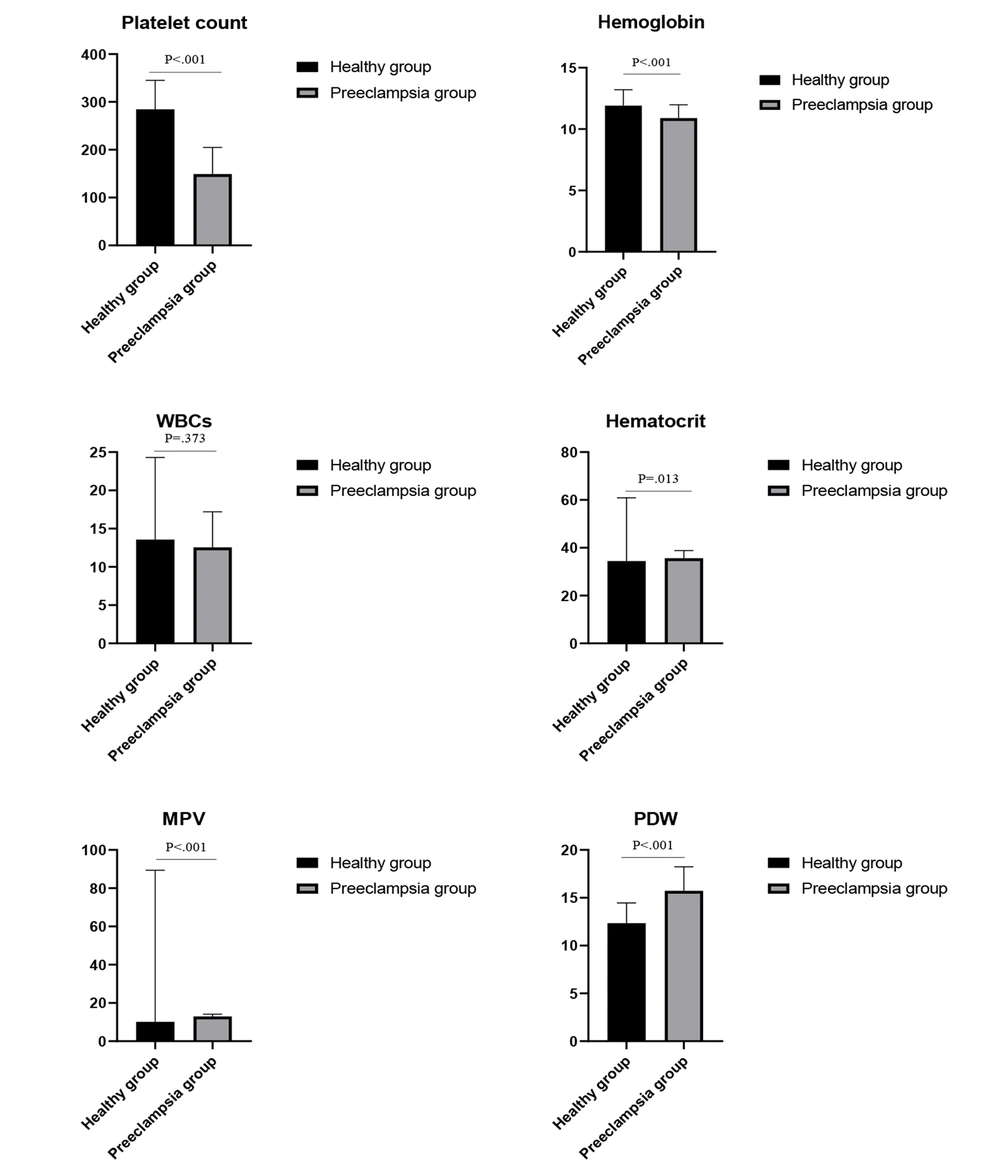
The results showed that there was a statistically significant difference between the mean hemoglobin level in healthy women (11.91 ± 1.30 gm/dL) and those with preeclampsia (10.89 ± 1.09 gm/dL) (P < 0.0001). Also, according to the findings, the individuals of the two groups had significant differences in terms of mean platelet volume and platelet distribution width (P < 0.0001).
Also, the results of the Mann-Whitney U test showed that there was a statistically significant difference between the number of platelet counts in healthy women (284.52 ± 60.58 mcL) and women with preeclampsia (149.30 ± 55.38 mcL) (P < 0.0001) (Figure 1).
5. Discussion
The aim of this study was to investigate the platelet indices, including platelet count, MP, and PDW, in healthy pregnant women and women with preeclampsia in Dezful city. The results showed that the hemoglobin level had a statistically significant difference between the two groups. This finding is consistent with the results of a study by Heydari et al. They examined platelet indices as a predictor of preeclampsia, which its mean was 11.63 ± 1.29 in the case group (and 12.04 ± 1.11 in the control group (8). Also, in the present study, the amount of hematocrit in both the case and control groups had a statistically significant difference. This finding is consistent with the results of Shojaeian et al., who examined the value of hematocrit and hemoglobin levels in predicting preeclampsia (14).
In the current study, the MPV in both studied groups had a statistically significant difference. These results were consistent with the findings of Thalor et al. In their study, they examined the relationship between platelet indices and preeclampsia (15). There was a significant difference in MPV between women with preeclampsia and healthy women in the study by Mannaerts et al. This finding was consistent with the current study (16). In line with the present study, Orgul et al. showed that the MPV and PDW were significantly different between women with preeclampsia and healthy women (17).
Bellos et al. found variations of MPV between women with preeclampsia and healthy women in a systematic review study. In their study, MPV in women with preeclampsia was significantly more than in women without preeclampsia (18), which is consistent with the results of the present study. Also, in the present study, the number of platelets in both groups was statistically different; this finding was also consistent with that of Kashanian et al. Also, in their study, the MPV was significantly different in both preeclampsia and non-preeclampsia groups in the third trimester of pregnancy, which is similar to the results of the present study. In their study, they investigated the value of measuring the mean platelet volume in the first and third trimesters of pregnancy in diagnosing preeclampsia (19). AlSheeha et al. showed a significant difference in the platelet count between two groups of pregnant women with preeclampsia and healthy pregnant women, which was consistent with the current study (20). In the present study, a statistically significant difference was observed in the platelet distribution of women with preeclampsia and without preeclampsia, who had lower platelet counts than healthy pregnant women. These results are consistent with the results of Yang et al. In their study, they examined the importance of platelet distribution as a clear marker in the incidence of preeclampsia (21). However, the results of Zanganeh et al. are not consistent with these results. They did not observe a significant difference between the two groups in terms of platelet distribution. They investigated the platelet counts and indices in healthy pregnant women and those with mild and severe preeclampsia (22). There was also no significant difference in MPV levels between women with preeclampsia and healthy women in the study by AlSheeha et al. (20). The difference in the results may be due to differences in race and geographical areas.
5.1. Conclusions
Platelet counts and platelet indices, including platelet count, MPV, and PD are affected by preeclampsia during pregnancy. These criteria can be used as a predictor of preeclampsia in the pregnancy care system. Also, preeclampsia is one of the most important factors in maternal and infant morbidity and mortality, and early detection of changes in platelet factors during pregnancy can be a predictor in the early detection of women at risk for preeclampsia. More studies seem to be needed using larger sample sizes and more geographical areas.