1. Background
Fertility, or the ability to have a child, is considered an accomplishment in reproduction and the beginning of new life for couples. On the other hand, infertility, by disrupting reproduction, has always had many unintended consequences for couples, sometimes treatable and sometimes incurable (1). It is estimated that 9% of couples all around the world have experienced some form of infertility, and 56% of them seek medical care for infertility (2). One of the most important factors in the success of assisted reproductive techniques (ART) is the quality of the embryo generated in the laboratory (3).
Many studies have demonstrated the close association of fetal morphology and quality with implantation rate and clinical fertility; however, a low-quality embryo also has the potential to provide fertility. On the other hand, low-quality embryos may further increase spontaneous abortions and reduce the total rate of pregnancy (4). Some studies indicate that the rate of clinical pregnancy and live birth in high-quality embryo transfer is twice the clinical pregnancy with a poor-quality one. However, there has been a similar chance of conceiving a clinical pregnancy that terminates in a live birth with low- and high-quality embryos (5). Some researchers also believe that in women under 36, the cumulative live birth rate can vary from 40% to 64%, depending on the quality of the fetus (6).
In addition, it has been shown that the simultaneous transfer of two embryos, compared with one embryo, increases the chances for fertility and live birth. Hence, the chance is one-third when one embryo is transferred compared with when two embryos are transferred (7). This is why most embryologists in infertility treatment centers around the world try to increase the number of transferred embryos when the quality of the embryos is low in the cleavage stage. Despite that, the decision to transfer only one high-quality embryo or two high- and low-quality embryos simultaneously is tough, and the question arises whether the simultaneous transfer of a low-quality embryo can reduce the implantation chance of the high-quality one. Some researchers believe that there is a paracrine interaction between embryos before implantation, which can affect the growth of concomitant and juxtaposed embryos (8). Studies have also shown that the simultaneous presence of a low-quality embryo in a culture medium reduces the growth rate and blastulation of other embryos (9).
2. Objectives
the purpose of this retrospective study was to evaluate the effect of the simultaneous transfer of a low-quality embryo on the implantation and growth of a high-quality embryo and ultimately the live birth rate.
3. Methods
The cross-sectional study was approved by the Dezful University of Medical Sciences Ethics Committee (IR.DUMS.REC.1397.005) and performed retrospectively using the referral records of admitted patients in Umm Al-Banin Infertility Treatment Center for IVF/intra cytoplasmic sperm injection (ICSI) procedures from 2013 to September 2020. The required data were extracted from the records and files using relevant checklists. Patients implanting one or two embryos aged 2 or 3 days were included in the study. The records of these patients were classified into four categories:
Group 1: Patients with the transfer of only one grade A embryo
Group 2: Patients with the transfer of two grade A and B embryos
Group 3: Patients with the transfer of two grade A and C embryos
Group 4: Patients with the transfer of two grade B and C embryos
The outcomes included the findings of a chemical pregnancy test (very early miscarriage within the first five weeks of pregnancy), BHCG hormone > 25 IU/L within 14 days after transfer, the number of clinical pregnancies (observation of pregnancy sac in ultrasonography), the number of abortions, the number of multiple conceive fertility and the number of live births (delivery at least 20 weeks after implantation). The quality of embryos was determined as follows: Equal blastomeres without fragmentation (grade A), equal blastomeres with slight fragmentation (grade B), and unequal blastomeres with or without fragmentation (grade C). Additional information in the patient files was also recorded, including the cause of infertility, ova numbers, estradiol levels, transfer date based on cycle, the quality of transferred embryos, chemical pregnancy outcome, clinical pregnancy outcome, abortion numbers, live birth numbers, and multiple pregnancies numbers (pregnancy with more than one fetus). Defective records and lack of accurate information registration were the reasons for the exclusion of the files.
3.1. Statistical Analysis
SPSS version 25 software was used for statistical analysis. The data were analyzed using descriptive statistical parameters, including mean and standard deviation (for quantitative variables) and frequency and percentage (for qualitative variables). The normality of the data was checked by the Kolmogorov-Smirnov test. Also, the Chi-square and one-way ANOVA test was used in the analytical analyses.
4. Results
During the study period (from 2013 to September 2020), 1,422 embryo transfer files of patients who were referred to the Dezful Infertility Treatment Center for IVF/ICSI procedures were registered. Of these, 802 cases met the inclusion criteria for the transferred embryo qualities. The number of people in each group was as follows:
Group 1: 156 patients with one or two grade A embryos (39.20%)
Group 2: 102 patients with two grade A or grade B embryos (25.63%)
Group 3: 64 patients with two grade A or grade C embryos (16.08%)
Group 4: 76 patients with two grade B or grade C embryos (19.10%)
According to Table 1, the age ranges of women and men participating in this study were 18 - 47 and 23 - 59 years, respectively. The mean age of women and men was 32.52 ± 5.10 and 37.59 ± 6.60 years, respectively. The infertility history of the subjects ranged from 1 to 26 years, with a mean of 6.50 ± 4.55 years. The most important causes of infertility in patients included the male factor in 38.19%, ovarian factor in 19.60%, and polycystic ovary in 28.89% of cases. Also, in 25.5% of infertility cases, they were multifactorial. Surprisingly, endometriosis, with a frequency of 1.51% was the least common cause of infertility in the research population. Endometrial thickness ranged from 4 to 11 mm, with a mean of 7.90 ± 1.01 mm.
| Variables | Group 1 | Group 2 | Group 3 | Group 4 | P-Value |
|---|---|---|---|---|---|
| Female age (y) | 32.86 ± 4.72 | 32.44 ± 5.49 | 32.12 ± 4.85 | 32.30 ± 5.56 | 0.74 |
| Male age (y) | 37.25 ± 5.97 | 37.38 ± 7.14 | 38.32 ± 6.46 | 37.96 ± 7.22 | 0.67 |
| Duration of infertility (y) | 6.52 ± 4.26 | 6.56 ± 4.49 | 6.60 ± 4.64 | 6.31 ± 5.24 | 0.97 |
| Cause of infertility | |||||
| Male factor | 31.23 ± 3.29 | 29.34 ± 4.12 | 33.45 ± 2.39 | 34.56 ± 4.38 | 0.75 |
| Female factor | 26.42 ± 2.13 | 24.34 ± 5.70 | 32.72 ± 3.45 | 29.43 ± 3.21 | 0.68 |
| Both | 24.42 ± 3.2 | 32.31 ± 4.3 | 28.56 ± 3.65 | 35.77 ± 4.83 | 0.72 |
| Endometrial diameter (mm) | 7.85 ± 1.04 | 7.92 ± 0.93 | 7.91 ± 0.97 | 7.99 ± 1.03 | 0.83 |
Demographic Parameters of the Study Groups
Concerning the characteristics of the ovarian cycle in patients (Table 2), estradiol levels ranged from 375 to 11632, with a mean of 2955.37 ± 2128.93. The number of recovered oocytes ranged from 1 to 24, with a mean of 6.84 ± 4.43. The number of adult ova in metaphase II ranged from 1 to 20, with a mean of 5.72 ± 3.63, the number of follicles was reported from 1 to 24, with a mean of 6.50 ± 4.28, and the number of embryos ranged from 1 to 20, with a mean of 4.05 ± 2.93.
| Variables | Group 1 | Group 2 | Group 3 | Group 4 | P-Value |
|---|---|---|---|---|---|
| Estradiol level (pg/mL) | 2852.90 ± 2155.22 | 3045 ± 2232.55 | 2731.89 ± 1721.37 | 3233.53 ± 2245.83 | 0.46 |
| Oocyte number | 6.55 ± 4.31 | 6.73 ± 4.41 | 7.39 ± 4.49 | 7.13 ± 4.47 | 0.56 |
| Mature oocyte (MII) | 5.43 ± 357 | 5.74 ± 3.76 | 6.29 ± 3.69 | 5.82 ± 3.51 | 0.45 |
| Follicle number | 6.28 ± 4.26 | 6.65 ± 4.31 | 6.71 ± 4.11 | 6.57 ± 4.47 | 0.86 |
| Embryo number | 3.64 ± 2.86 | 4.21 ± 3.09 | 4.39 ± 2.80 | 4.40 ± 2.93 | 0.15 |
Characteristics of the Ovarian Cycle of the Study Groups
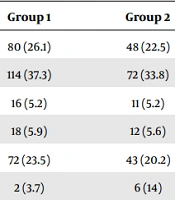
Table 3 compares fertility outcomes for the simultaneous transfer of embryos with different qualities. Accordingly, the formation of the embryo's heart was observed in 31 (36.05%), 25 (29.07%), 17 (19.77%), and 13 (15.12%) cases in groups 1 to 4, respectively. These differences were not statistically significant (P = 0.47). Fertility results based on pregnancy hormones accounted for 43 (34.68%), 37 (29.84%), 24 (19.35%), and 20 (16.13%) cases in groups 1 to 4, respectively, showing no statistically significant differences (P = 0.25). The identified frequencies of chemical abortions in groups 1 to 4 were eight (36.36%), five (22.73%), six (27.27%), and three (13.64%), respectively (P = 0.13), while the frequencies of clinical abortions in these groups were four (25%), eight (50%), one (6.25%), and three (18.75%), respectively (P = 0.27); there was no significant difference between these groups. The live birth cases were as follows: Group one 25 (33.33%), group two 24 (32%), group three 15 (20%), and group four 11 (14.67%) (P = 0.26). Multiple pregnancy cases were five (33.33%), six (40%), two (13.33%), and two (13.33%) in groups 1 to 4, respectively. The chi-square test showed that the observed differences were not significant (P = 0.79).
| Pregnancy Outcome | Group 1 | Group 2 | Group 3 | Group 4 | P-Value |
|---|---|---|---|---|---|
| Clinical pregnancy | 80 (26.1) | 48 (22.5) | 27 (27.8) | 35 (18.8) | 0.2 |
| Biochemical pregnancy | 114 (37.3) | 72 (33.8) | 34 (35.1) | 49 (26.3) | 0.09 |
| Chemical abortions | 16 (5.2) | 11 (5.2) | 7 (7.2) | 7 (3.8) | 0.66 |
| Clinical abortions | 18 (5.9) | 12 (5.6) | 1 (1) | 9 (4.8) | 0.27 |
| Live births | 72 (23.5) | 43 (20.2) | 23 (23.7) | 28 (15.1) | 0.12 |
| Multiple pregnancies | 2 (3.7) | 6 (14) | 3 (13.6) | 3 (10.7) | 0.78 |
Pregnancy Outcomes and Complications in the Study Groups
5. Discussion
The referral of many patients to infertility treatment centers, which is estimated up to about 15% of the general population, requires planning to provide the necessary conditions for the best possible services in the laboratories of infertility treatment centers. One of the main goals of assisted reproduction methods is to produce embryos with the highest quality, which has always been a challenge for experts in this field (10). Our study was designed based on the following questions: What should embryologists do with a low-quality embryo? Should they remove or keep it? Although a low-quality embryo still has a chance of survival, the concern is that in low- and high-quality embryo transfer, the low-quality embryo may harm the high-quality one. Hence, the present retrospective study was performed to evaluate the success rate of fertility regarding the simultaneous transfer of embryos with different qualities in IVF candidates. Intra cytoplasmic sperm injection was designed and implemented. Out of 1,422 available samples, 802 cases with qualified characteristics in terms of embryo quality and other factors were entered into the study. The grade A and B embryos were considered high-quality embryos, and low-quality embryos were labeled grade C embryos.
The findings indicated that the fertility rate, clinical and chemical abortions, and live and twin birth rates were not significantly different between the groups. Hill et al. evaluated the fertility rates for transmitted embryos with different qualities. In their retrospective study, 4,640 patients who had in vitro fertilization were analyzed, and the findings revealed that the transfer of the second embryo with lower quality had no negative impact on the live birth rate, which is consistent with the present results. However, this study showed that the transfer of the second, low-quality embryo increased the live birth rate by 10% and the multiple birth rate by 15% (11). However, in the current study, the rate of live birth and multiple births did not show a significant difference between the groups. Aldemir et al. showed that the live birth rate was higher in patients who received two high-quality embryos than in groups that received two embryos of different qualities (12), which is inconsistent with the present results that indicated no significant effect due to the simultaneous transfer of two high-quality embryos, i.e., grade A-A and A-B embryos.
Li et al. assessed the impact of low-quality embryos on high-quality embryos in concomitant transfer cases and approved no significant difference in pregnancy and live birth rates between patients in the two study groups, but the pregnancy rate for twins and multiples was significantly higher in cases of concomitant low/high-quality embryo transfer (13). There was no significant difference concerning the birth rate of multiples between different groups. Similarly, in a study by Oron et al., no differences were observed concerning abortion rates and pregnancy complication rates for the mother and the fetus (5). In contrast, Tao et al. stated that the transfer of a low-quality embryo would harm the high-quality embryo (14). Two other researchers also investigated the issue, and both confirmed that low- and high-quality embryo transfer could reduce implantation and fertility rates. However, these researchers did not report any differences in terms of clinical pregnancy rates, live birth rates, abortion rates, abnormal pregnancy rates, or multiple pregnancies, which is consistent with the current findings (15, 16).
5.1. Conclusions
The findings showed that pregnancy outcomes, including fetal heart formation, hormonal indices, multiple birth rates, chemical, and clinical abortions, and live birth rates, were not significantly associated with the simultaneous transfer of embryos with different qualities. Accordingly, the fertility success rate is not possibly affected by the simultaneous transfer of embryos with different qualities in IVF/ICSI candidate patients. However, due to the lack of sufficient studies, further research is recommended at other infertility treatment centers to obtain more accurate results by comparing achievements.