1. Background
In today's competitive world, in order to survive, be profitable, and achieve their goals, organizations must use the available resources in an optimal way and with high efficiency. Hospitals are among the important organizations in society and pursue the goal of improving the health level of society by providing health services. Today, providing intensive care to patients with acute health conditions is a vital part of health systems. However, the high costs of intensive care units (ICU) have limited their development, especially in low-income countries (1). The management of hospital affairs is one of the main requisites for hospital functioning, and hospital managers are always trying to improve the quality of services, boost efficiency, and reduce costs. Therefore, hospital management is a solution to increase the capacity of the hospital to standardize hospital affairs, increase supervision, and improve workflow and performance in the health sector (2). Process management is underpinned by 3 key factors: guaranteeing and maximizing the safety of patients and professionals, improving clinical practice, and streamlining processes to make them more efficient (3-5). Increasing the efficiency of processes involves analyzing how different hospital workflows are managed. Although this event primarily concerns patient flow, it also includes internal and external communication flow and the integral logistic flows of materials and equipment (6, 7).
The emergency department is one of the important places in a hospital where patients with critical conditions who need urgent measures are admitted. Therefore, any improvement in the processes of the emergency department can not only reduce hospital costs but also upgrade health services in terms of quality and speed of delivery, which are of paramount importance in relation to emergency services (8).
Lean thinking is an attitude that pursues productivity promotion, continuous value creation, and cost minimization through the identification and elimination of waste sources. This approach increases performance using a set of techniques to identify and eliminate various wastes of productivity (9). By applying this approach, a new organizational image is presented, which defines the organization as a set of processes with the aim of creating values for the customer. According to the lean process, there is a need to identify and eliminate activities that do not have added value in the design, production, logistics, and customer-related processes (10). The lean management approach is based on two foundations: eliminating waste and improving processes. The former relies on continuous improvement, optimization of human resources, productivity, and zero inventory, aiming to reduce waste. The second pillar, i.e., process improvement, is intercalated with elements like contingency management, strategic thinking, error elimination, process optimization, and fast decision-making. With the implementation of the lean management system, the organization becomes more resistant to environmental turbulences and crises, and by identifying and eliminating processes without added value, lean management improves productivity and increases the organization’s flexibility and innovation in facing external issues (11). Although the lean system was originally created to maximize the performance of manufacturing organizations, it is also applicable to improve the performance of non-manufacturing organizations.
Regarding the capabilities of this approach, many health service provider organizations have now started to establish a lean management system. The following requirements set by healthcare institutions are considered: (1) process management (i.e., coordinating a large number of resources; human, technological, material, and healthcare, which must match the demands of patient waiting lists and hospital resource management); and (2) service provision to a large number of patients in public hospitals with existing resources, requiring maximizing the efficiency of medical teams to meet unlimited demands. Amid the post-pandemic era in 2023 and after surviving the COVID-19 pandemic, it is even more necessary for healthcare centers to have planning tools to optimize the efficiency of their resources, which requires knowledge and appropriate management (7).
Ebrahimipour et al. investigated the role of implementing lean management in improving hospital processes and reported a 0.4% decrease (from 6.4 to 6%) in the rate of discharge with personal consent and a 4% increase in overall patient satisfaction (12). Montazeralfaraj et al. identified the opportunities to promote emergency processes using value flow mapping in Imam Reza (AS) Hospital of Birjand. The required data were collected through observations and interviews. The elapsed time for each procedure in the emergency department was measured from registration to discharge. The results showed that the total time spent in the emergency room was 6.209 minutes on average, of which 6.143 minutes (50.68%) were spent waiting for services (13). Saidi-Mehrabadet al. evaluated the performance speed of a hospital’s emergency room in Tehran based on lean principles and Goodson’s performance evaluation model. It was found that this approach was able to identify the factors interfering with cleansing emergency centers in the shortest time possible and helped save time and prevent the wastage of resources by eliminating them. The implementation of the rapid performance evaluation program can help increase the quality of services and improve performance in emergency departments, especially where there are limited medical, instrumental, and human resources. This is important as emergency departments are directly related to the survival of humans (14).
2. Objectives
The sources of futile hospital activities have been identified in none of the studies conducted in Iran so far. In addition, no localized framework has been designed to establish a lean management system in Iranian hospitals. The specific characteristics of a hospital require a suitable framework to identify and eliminate activities that lack customer values. In this research, after examining emergency processes and identifying various types of waste, a framework was presented to establish lean management in the emergency department of the hospital.
3. Methods
The present qualitative-applied study was conducted in 2021 in order to provide a lean management framework in the hospital emergency department. First, by reviewing the relevant literature, the types of waste and the set of requirements and solutions related to the establishment of the lean management system in organizations, mainly industrial organizations, were identified. In this way, research articles and books related to lean management were used (15-27). In the second step, industry and management experts’ opinions and consultation were sought to determine the requirements of establishing the lean management system and localize them to suit the hospital environment. In the third stage, through interviews with hospital managers, the status of each of these requirements and the types of waste in the emergency department were identified (Table 1). The first and second columns of the table show the types of losses and their states, respectively. Wastes were regarded as activities that did not create value. The content of this table was set by modeling similar research in the industry and using the opinions of the interviewed experts.
| Waste Explanation | Examples |
|---|---|
| Waste of waiting | |
| Waiting for the technician's request and arrival before the patient's admission | The information system does not alert the radiology technician that the emergency department has sent a request for a radiological examination or that the patient has been referred. |
| Delay in referrals | The length of the patient's stay is prolonged due to delays in referral by the staff of emergency and psychiatric departments; Staff are waiting for the result. |
| Delay in triage | During peak hours, the number of patients exceeds the capacity of a triage nurse. |
| Waiting for the doctor/nurse | Patient waiting for evaluation. |
| Waiting for inpatient beds | The patient is waiting for beds in the emergency department to be emptied. |
| Other delays | Update delays; Delays caused by patient transfer |
| Displacement loss | |
| Unnecessary and inappropriate patient transport | Patients were transferred from one department to another upon the preferences of staff. |
| Long transportation | Long distances between service departments |
| Loss of inventory | |
| More or less than the required inventory | Oversupply of inventory to ensure availability; Inventory is unavailable or has expired. |
| Useless documents | Unnecessary patient forms |
| Unnecessary resources | Non-optimal allocation of nurses to shifts |
| Sequential or multiple tests | Ordering tests for more than one patient at the same time |
| Loss of movement | |
| Doctor/nurse’s localization | Nurses’ looking for a doctor (or vice versa) or patients - Employees’ going to different wards for photocopying. |
| Patient movements | After triage, even if there is an open bed, the patient is returned to the waiting room. |
| Transfer of administrative personnel | Long distance between administrative process steps |
| Loss of service (error, service more than required, service less than required) | |
| Unnecessary first visits | In some cases, the first visit only includes the request for a radiological examination, and therefore, it is useless for the patient to wait for it. |
| Over-triage | Unnecessary triage |
| Unnecessary activity | Radiology admission |
| Unnecessary tests | Unnecessary inspection orders |
| Redundant information | Registering the same information several times |
| Lack of services between departments | Many patients are referred to the wrong department due to non-specific symptoms or are forced to provide information. |
| Bed availability | Lack of empty beds, unnecessary bed occupation |
| Medication errors and inappropriate treatments | Antibiotics for viral infections, unnecessary surgical procedures, medication errors |
| Communication problems | Communication problems |
| Waste in the process and methodology | |
| Ambiguity in responsibilities | Lack of a clear definition for roles and responsibilities. |
| Absence of replacement processes | Patients’ demands and numbers exceeding the available capacity. |
| Lack of coordination | Overlapping evaluations |
| Repeated reviews | The doctor/nurse performs tests or administers medications separately; Re-evaluation of the patient by different staff |
| Lack of standard protocols | No standards for using hallways for patient; assignments (doctors’ self-assignment of patients); Lack of standard procedures for handoffs |
The research community included management specialists, experts and managers working in the hospital, and statisticians. Purposeful sampling was employed to select 15 people (4 experts working in the field of health and treatment, 8 experts in the field of management and industrial engineering, and 3 statisticians). Of these, 7 experts in the field of management and industrial engineering and 2 of the hospital managers accepted the invitation and participated in the interview. The focus-group discussion technique was used to conduct the interviews (a total of six 90-minute interviews). All the interviews were conducted in the interviewees’ workplaces and lasted 40 minutes on average. These interviews were conducted in a semi-structured and in-depth manner. In order to analyze the interviews, the qualitative content analysis method was used. The answers of the interviewees were recorded by the 2 interviewers in parallel, and in the next step, they were converted into individual files by software assistance. Table 1 describes different types of waste (activities without added values) and their examples.
In this research, measures were undertaken to ensure 4 data rigor criteria, including credibility (validity), trustworthiness (reliability), confirmability (lack of bias), and transferability. According to the solutions proposed in scientific articles to realize each of these 4 features (28, 29), selective solutions were used. For example, in order to confirm the reliability of the data, 2 people who had no conflict of interest on the subject were interviewed in parallel. Also, in order to achieve transferability, the data were collected in full detail and in a clear and unambiguous manner. In order to ensure verifiability, notes, and documents related to the interviews were saved for subsequent reviews. The NVIVO10 software was used to code and store all interview documents. In order to confirm the credibility of the study, during all stages of data collection, the topic and aims of the research were clearly explained to the interviewees, and the accuracy of the interviewers’ opinions (self-review) was confirmed during the process. Also, the answers of different interviewees were matched with each other. Ethical considerations were observed in all steps of the research.
4. Results
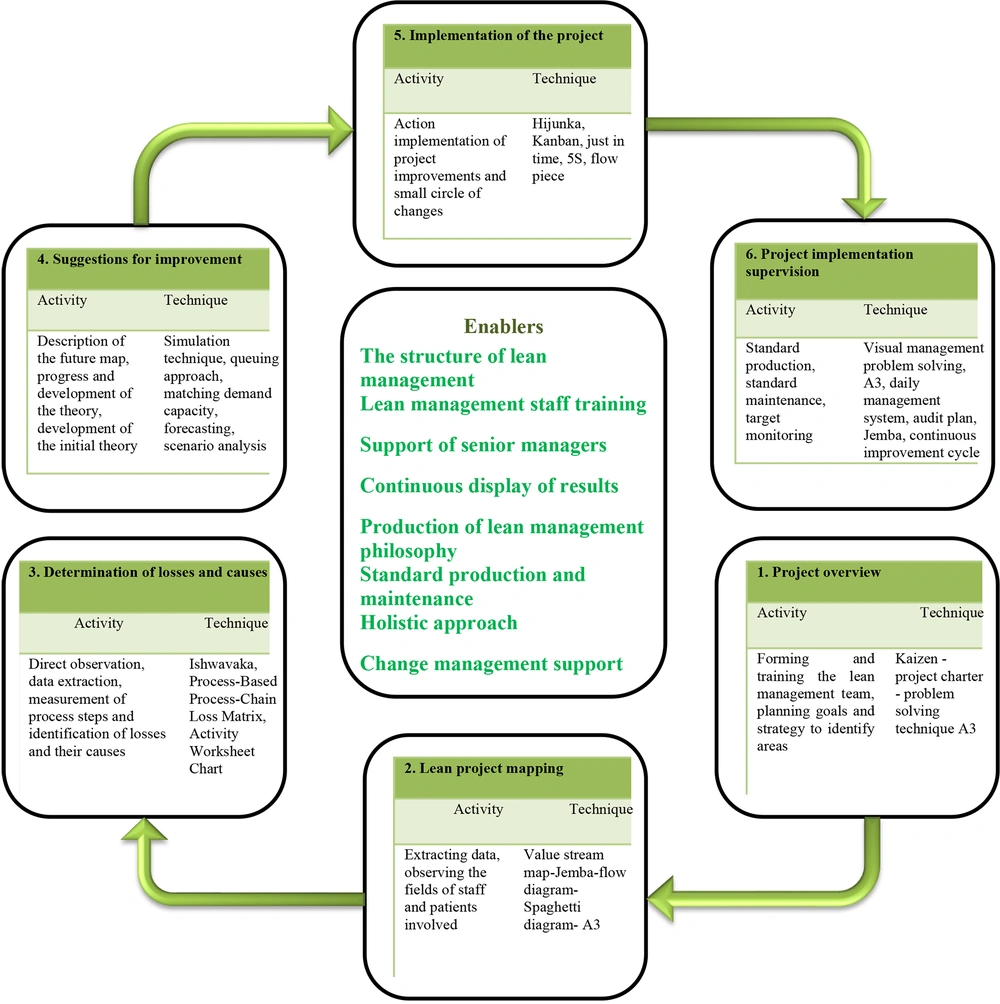
The findings derived from the interviews were summarized, classified, and presented in Table 1. In order to achieve our main goal, which was to provide a framework for the implementation of lean management in the hospital emergency department, various techniques and tools used to implement lean management mentioned in previous articles were identified (Table 2). In the next step, regarding available lean management techniques and based on the opinions of the experts interviewed with regard to the solutions and requisites of a lean management framework in the emergency department, key effective factors required for the successful implementation of lean management in the emergency department were characterized. According to the lean management philosophy, a set of hard and soft methods are needed, and hard tools (i.e., the value stream map and flowcharts) should be implemented in combination with soft measures (i.e., continuous improvement, leadership support, and employee participation).
| Activity | Implementation Techniques and Tools |
|---|---|
| Team training | Holding meetings and educational workshops |
| Planning | Using a project charter |
| Mapping | Process input suppliers and output applicants; Problem solving techniques (A3); Value stream mapping |
| Gathering information | Flowcharts; Spaghetti diagram; Gemba |
| Losses and their causes | Ishikawa Problem-solving techniques (A3); Techniques of asking five "whys"; Lost matrix; Root-cause analysis |
| Suggestions for improvement | Process-oriented process chain; Chart activity worksheet; Process planning, preparation, process implementation; Simulation techniques; Queuing approach, demand-capacity matching, forecasting, scenario analysis |
| Implementation | Rapid process improvement workshops; H Heijunka; Kanban; Just in timeOne piece flow5S |
| Control | Balance chart; Poke yoke Problem-solving techniques (A3); Visual management; Daily management system; Control chart; Audit programs; Gemba; Data-driven improvement cycle; Continuous improvement cycle |
In this study, 6 types of waste were identified in the sections of waiting, transfer, inventory, movement, additional measures, errors, and process defects (Table 1). Deming’s cycle model was used in order to provide a framework for establishing a lean management system. The Deming cycle is a repetitive 4-step process that moves towards further improvements in each iteration. The 4 stages of the Deming cycle include planning, performing, checking, and acting. The first and most important phase of this cycle includes planning, which encompasses determining goals, predicting ways to achieve them, and pledging commitment to perform certain activities to achieve these goals. In the check & review process, we compared the results obtained with the set goals. If necessary, necessary corrections (i.e., completing and editing) were made to both activities and goals. If everything in the previous steps was correct, the fourth step begins, including taking action and correcting plans and programs (35). This general model is the basis of many transformation models, and the current study’s model was also presented based on this framework with some changes and corrections. Based on previous studies in other organizations, the set of measures that should be taken to establish a lean management system in hospital emergency departments was as follows (31-33): gathering a multidisciplinary team for the lean project, supporting the senior management team (including all stakeholders in the lean project team), implementing small and simple changes, creating a culture of desire for change and improvement, elaborating the principles and techniques of lean management in the organization’s control system, developing a structured method for lean project implementation, focusing on the process flow, training employees on lean management, establishing effective communication between all stakeholders, adopting a systemic and holistic approach, creating and maintaining standards, nurturing and expanding the lean management philosophy, employing a continuous improvement approach, mapping processes clearly and precisely to present the proposed framework.
These measures were divided into 7 positions based on the Deming cycle, including a set of activities as enablers, which were placed in the center of the model. The other 6 areas included sets of executive steps for lean management system implementation in the model environment as a repeating cycle. Each of these areas includes a set of executive and relevant activities and techniques. The 6 steps of the proposed model included the setting of project generalities, lean project mapping, determination of losses, determination of improvements, implementation of improvement proposals, and final control. The repetitiveness of the model cycle means that every time the actions are repeated and implemented by checking and controlling the results and taking corrective measures, a new cycle starts from the implementation step. In fact, a continuous and endless process toward improvement is formed. Figure 1 presents the framework proposed for implementing lean management in an integrated format. As shown in this figure, various lean management tools employed are given in the second column of Table 2. Facilitating and empowering factors, such as employee training, support senior managers, multipurpose decisions, etc., are placed in the model’s environment, allowing for the successful realization of the lean system. In the center of the model, the enablers that increase the probability of the hospital’s success in implementing lean management are given, and managers need to pay attention to these enablers and strengthen them.
5. Discussion
Hospitals, like any other organization, have various sources of waste in their activities. In this research, six categories of waste in hospitals were presented with related examples. After identifying waste sources and according to lean management implementation projects in other organizations, different activities required for the establishment of the lean management system in a hospital emergency department were identified and compiled. Finally, based on the Deming cycle, the proposed framework for the establishment of the lean management system was provided. The framework proposed included a central core (called enablers) and a recurring cycle in the model environment. The repetitive cycle consisted of 6 activities, for which, in each iteration, different wastes were identified in the hospital’s activities. Then, actions were taken to solve them through the proposed technique. The enablers at the center of the framework increase the likelihood of the project’s successful implementation and better outcomes. As can be seen in the model, the first stage comprises planning and setting goals and resources, creating and training the team, and reviewing the current situation. These activities provided the possibility of defining the boundaries of the project, determining its goals and their feasibility according to time and resource limitations, and focusing on the improvement process. The use of lean management tools allowed identifying waste sources in the hospital during admitting and treating a patient. Defining problems and implementing improvements allowed for the development of new workflow standards that significantly shortened the time spent on activities not directly related to patient care. The most important waste was paper-work medical documentation and its shift toward electronic forms allowed for better use of human capital resources (36).
In the second stage of the project, vital processes and analysis of related information were performed. The project team analyzed the obtained map to identify losses and activities with no added values, determined the types of losses, and tracked their root causes. The waiting time was one of the main wastes in the emergency room. Also, the waste of inventory, actions beyond the requirement, unnecessary transfers, and errors in services were also among other types of waste. In addition, the lack of standard protocols when performing procedures in the emergency department was observed to extend the waiting time, medical errors, and repetition of unnecessary tasks. In the next steps, improvement measures were presented and implemented, and finally, in the last stage, the implementation process was monitored.
The emergency department provides urgent diagnostic-therapeutic care for patients who have been injured due to accidents and incidents or whose illness has suddenly worsened. In the emergency department, minutes and seconds are important for saving the patient’s life (37). Waiting time can be known as one of the important wastes of the emergency department because it is closely related to the patient’s health. In fact, waiting time to receive services is an important indicator for evaluating the efficiency of emergency departments (38). The lean approach is a value-added system that reduces costs and wastes to continuously improve the quality performance of the healthcare organization. Also, reducing the costs associated with health care services is on the agenda, if possible, besides improving their quality (39).
The innovation of the present research was to identify different types of waste in the executive activities of the hospital emergency department, on the one hand, and also to provide an executive framework for the implementation of the lean management system. Of course, by implementing the proposed framework in hospitals and checking its function, improvements can be made to the proposed model. The most important limitation was communication difficulties caused by the coronavirus pandemic in the country.
5.1. Conclusions
The framework developed in this study (Figure 1) presents the lean system implementation cycle in the hospital emergency department following six steps, through which and by focusing on the enablers of the lean approach, hospital managers will be able to systematically move through a repetitive cycle to identify and eliminate their waste sources. In this direction, it is necessary to attract the participation of all nurses and doctors in the implementation of the project. In each step, the activities and techniques suggested in the model should be implemented depending on the conditions of the organization. For this purpose, it is recommended to definitely use the services of an external consultant with professional knowledge regarding lean management system implementation. The implementation of quality management techniques, including lean management, in a healthcare system can lead to greater satisfaction of clients, improve the performance and efficiency of employees, and reduce the waste of resources and costs. Applying the lean system in the health sector can lead to reducing costs, increasing the flexibility of centers against changes, and ultimately, continuous development through review and improvement processes, elimination of defects, correction of errors, and ceasing processes that do not create added value. This approach helps hospitals define and understand customer values and design new processes accordingly. The implementation of the lean management framework established in this study in the hospital can increase the efficiency of operations and reduce losses in various sectors, including human power, consumables, equipment, and funds. In fact, all resources should be used in the path of value production. In addition to increasing performance efficiency, the implementation of lean management will bring satisfaction to clients and employees. Designing standard procedures based on the lean approach’s prescriptions for each process in the health system can reduce waiting time, implementation errors, and rework. In this article, a framework was offered for implementing the lean management system in the hospital emergency department. The use of the lean management system in industrial factories has been able to reduce production costs to a great extent by eliminating waste, a function that can be achieved in the healthcare sector as well by increasing the quality of healthcare services. The framework presented here provides hospital managers with practical techniques for the implementation of the lean system. Considering the high capability of the lean management approach in identifying and eliminating waste sources and improving performance efficiency, it is suggested that the importance and impact of this approach be taught to hospital managers and experts in the form of articles and training courses.