1. Background
Iran is located in the Middle East with a population of more than 79.92 million people, including 39.42 million females and 40.49 million males. Iran is ranked 18th in the world in terms of population (1) In the last few decades, the country has undergone rapid demographic, economic, and social changes. Also, the population growth rate in Iran has decreased, which has caused a change in the age structure. The age group of 20-29 years has become the main age group of Iranian people (2).
According to the World Health Organization (WHO), in the coming decades, we will see changes in the epidemiological patterns of global diseases, and psychiatric disorders will become more prevalent (3). The WHO estimates that one in four families will have at least one member with a psychiatric disorder, and this will impose the most global burden of disease (4). Psychiatric and common disorders impose a huge burden globally, and global burden disorders state an estimated 28.62% of the total disability-adjusted life years in 2013 in the world (5).
Comprehensive studies on the epidemiological status of psychiatric disorders in Iran have been conducted from 1999 to 2015. In the first national study of psychiatric disorders in Iran conducted by Noorbala et al., 21% of the population over the age of 15 had a psychiatric disorder (1). The results of a similar study showed that the prevalence of psychiatric disorders was 23% (6). The latest study, conducted in 2015, showed that a total of 23.4% of the subjects were suspected of psychiatric disorders; in this study, the prevalence of mental illnesses varied in various provinces (7). In a review study published in 2020, the prevalence of psychiatric disorders in Iran was 31% in studies using screening tools and 21% in studies conducted with clinical interviews (8). Also, a review of studies on the prevalence of mental illnesses showed that the prevalence rate varies across Iran (1, 9).
The prevalence of psychiatric disorders in some parts of Iran is as follows: 21.5% in Tehran, 23.8% in Gilan, 23.7% in Kashan, 19.9% in Isfahan, 17% in Rudsar, 16.6% in Gonabad, 14% in Semnan, and 12.5% in Meibod (10). Also, according to previous studies, the prevalence of various types of psychiatric disorders is different (10-12). Epidemiologic studies in the field of psychiatric disorders play a vital role in determining the mental health of the community and subsequent policy-making and planning (13). Effective planning to provide mental health services in Iran needs fundamental demographic information, the prevalence by the type of disease, and the survey of the country’s health status (3). To make policies and strategies for the control and prevention of psychiatric disorders, the prevalence of various types of diseases in each specific community should be determined (2). For instance, data on the prevalence and incidence of psychiatric disorders assist in the identification of those needing treatment and aid in facilitating access (5).
There is little information about the possible impact of social, economic, and health developments on people's mental health status. Addressing the health needs of people requires current information in diverse areas (6). The results of a study on the mental health status of people over the age of 15 in Lorestan province showed that more than one-third of the subjects were suspected of psychiatric disorders. Also, the prevalence of psychiatric disorders increased from 19.7% in 1999 to 36.3% in 2015. The prevalence of patients suspected of anxiety and somatization symptoms was higher than the prevalence of depression and anti-social disorders (12). Similar results were obtained in other regions of Iran (12, 14, 15). However, with social alterations in recent years, there is a potential change in the structure of society in terms of mental health. Population-based studies of psychiatric disease prevalence in Lorestan are rare, equally considering the prevalence of psychiatric disorders in numerous regions of Iran.
2. Objectives
This study aimed to investigate the prevalence of psychiatric disorders in patients referring to a psychiatric clinic in Lorestan province.
3. Methods
A cross-sectional study was conducted on all people aged 18 years or older. The survey was conducted from January to June 2018. The study population included people referring to the Psychiatric Disorders Clinic of Lorestan University of Medical Sciences, Khorramabad, Iran. Participants were selected by a convenience sampling method. A total of 750 individuals participated in the examinations. Subjects were referred for clinical interviews by two psychiatrists based on the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) checklist. The clinical interview checklist was provided by two psychiatrists based on the DSM-5 criteria and assessed simultaneously by two psychiatrists to agree upon the same diagnosis. The Kappa coefficient was 0.87. This tool included 149 symptoms of psychiatric disorders, including anxiety, mood disorder, psychosomatic disorders, psychotic disorders, mental retardation, epilepsy, and psychiatric disorders caused by organs (15).
In addition, a questionnaire was designed and used to collect basic and demographic information. The items of this questionnaire included gender, age, education, occupation, marital status, history of drug addiction, and history of physical or mental disorders in the family. The answers to this semi-structured questionnaire were collected as self-report. The average time for answering the questions was about 45 minutes. SPSS version 22 was used for data analysis. Absolute frequency, relative frequency, mean, and chi-square test were utilized to report the data. Before completing questionnaires, participants provided their informed consent, and all information remained confidential. The study was approved by the Ethics Committee of Lorestan University of Medical Sciences.
4. Results
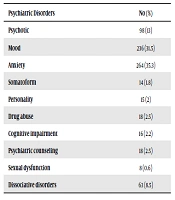
A total of 750 individuals were invited to participate in this study. The participants had a mean age of 45.0 ± 14.4 years. Women included 53% of the study sample. Table 1 illustrates the participants' demographic information. Psychiatric disorders were most frequent at the ages of 21-30 years and among people with illiterate or primary education (52.4%). Housekeepers showed a high prevalence of psychiatric disorders (29.5%) (Table 2). The most prevalent psychiatric disorders were anxiety (35.3%) and mood disorders (31.5%) (Table 3). The most prevalent anxiety disorder was generalized anxiety disorder (60%) (Table 4).
| Variable | No (%) |
|---|---|
| Age | |
| 20 ≥ | 125 (16.7) |
| 21-30 | 214 (28.5) |
| 31-40 | 212 (28.3) |
| 41-50 | 120 (16) |
| 50 ≤ | 79 (10.5) |
| Gender | |
| Male | 353 (47) |
| Female | 397 (53) |
| Education | |
| Illiterate or Primary | 393 (52.4) |
| Diploma | 202 (27) |
| Higher than diploma | 155 (20.6) |
| Occupation | |
| Student | 138 (18.4) |
| Worker | 88 (11.7) |
| Self-employed | 147 (19.6) |
| Unemployed | 150 (20) |
| Housekeeper | 221 (29.5) |
| Retired | 6 (0.8) |
| Marital status | |
| Single | 305 (40.7) |
| Married | 389 (51.8) |
| Widow | 41 (5.5) |
| Divorced | 15 (2) |
| Drug addiction | |
| Yes | 125 (16.6) |
| No | 625 (83.4) |
| Family history of psychiatric disorders | |
| Yes | 209 (27.8) |
| No | 541 (72.2) |
| Disorders | Psychotic | Mood | Anxiety | Somatoform | Personality | Drug Abuse | Cognitive impairment | Psychiatric counseling | Sexual dysfunction | Dissociative | Total |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age | |||||||||||
| 20 ≥ | 10 (8) | 14 (11.2) | 37 (29.6) | 3 (2.4) | 7 (5.6) | 2 (1.6) | 2 (1.6) | 12 (9.6) | 2 (1.6) | 36 (28.8) | 125 (16.6) |
| 21-30 | 28 (13.1) | 82 (38.3) | 71 (33.2) | 3 (1.4) | 2 (0.9) | 10 (4.7) | 4 (1.9) | 3 (1.4) | 1 (0.5) | 10 (4.7) | 214 (28.5) |
| 31-40 | 39 (18.4) | 70 (33) | 73 (34.4) | 3 (1.4) | 4 (1.9) | 5 (2.4) | 2 (0.9) | 2 (0.9) | 2 (0.9) | 12 (5.7) | 212 (28.2) |
| 41-50 | 14 (11.7) | 35 (29.2) | 55 (45.8) | 3 (2.5) | 2 (1.7) | 1 (0.8) | 4 (3.3) | 0 (0) | 1 (0.8) | 5 (4.2) | 120 (16) |
| 50 ≤ | 6 (7.6) | 36 (45.6) | 28 (35.4) | 2 (2.5) | 0 (0) | 0 (0) | 4 (5.1) | 1 (1.3) | 2.25 (10.5) | 0 (0) | 79 (10.5) |
| Gender | |||||||||||
| Male | 61 (17.3) | 91 (25.6) | 109 (31) | 5 (1.4) | 9 (2.6) | 16 (4.5) | 6 (1.7) | 5 (1.3) | 4 (1.1) | 47 (13.4) | 353 (47) |
| Female | 13 (9.1) | 146 (36.7) | 155 (39) | 397 (53) | 9 (2.3) | 6 (1.5) | 2 (0.5) | 10 (2.5) | 13 (3.3) | 4 (1) | 397 (53) |
| Education | |||||||||||
| Illiterate | 13 (14.7) | 24 (27) | 34 (38.2) | 2 (2.2) | 2 (2.2) | 5 (5.6) | 0 (0) | 5 (5.6) | 2 (2.2) | 3 (3.4) | 304 (40.5) |
| Primary | 33 (10.9) | 94 (30.9) | 87 (28.6) | 7 (2.3) | 7 (2.3) | 3 (1) | 9 (3) | 10 (3.3) | 5 (1.6) | 49 (16.1) | 89 (11.8) |
| Diploma | 35 (17.4) | 64 (31.3) | 73 (36.3) | 3 (1.5) | 5 (2.5) | 6 (3) | 5 (2.5) | 3 (1.5) | 1 (1) | 6 (3) | 202 (26.9) |
| University | 16 (103) | 55 (35.5) | 70 (45.2) | 2 (1.3) | 1 (0.6) | 4 (2.6) | 2 (1.3) | 0 (0) | 0 (0) | 5 (3.2) | 155 (20.6) |
| Occupation | |||||||||||
| Student | 10 (7.2) | 36 (21.1) | 50 (36.2) | 3 (2.2) | 3 (2.2) | 3 (2.2) | 1 (0.7) | 4 (2.9) | 0 (0) | 28 (20.3) | 138 (18.4) |
| Worker | 10 (11.4) | 29 (33) | 41 (46.6) | 0 (0) | 0 (0) | 2 (2.3) | 0 (0) | 0 (0) | 2 (2.3) | 4 (4.5) | 88 (11.7) |
| Self-employed | 30 (20.4) | 49 (33.1) | 44 (29.9) | 1 (0.7) | 2 (1.4) | 5 (3.4) | 3 (2) | 2 (1.4) | 1 (0.7) | 10 (6.8) | 147 (19.6) |
| Unemployed | 32 (21.3) | 39 (26) | 32 (21.3) | 4 (2.7) | 7 (4.7) | 7 (4.7) | 3 (2) | 7 (4.7) | 3 (2) | 16 (107) | 150 (20) |
| Housekeeper | 15 (6.8) | 82 (37.1) | 94 (42.5) | 6 (2.7) | 3 (1.4) | 1 (0.5) | 8 (3.6) | 5 (2.3) | 2 (0.9) | 5 (2.3) | 221 (29.4) |
| Retired | 0 (0) | 2 (33.3) | 3 (50) | 0 (0) | 0 (0) | 0 (0) | 1 (16.7) | 0 (0) | 0 (0) | 0 (0) | 6 (0.8) |
| Marital status | |||||||||||
| Single | 45 (14.8) | 84 (27.5) | 86 (28.2) | 6 (2) | 9 (3) | 11 (3.6) | 5 (1.6) | 7 (2.3) | 3 (1) | 49 (16.1) | 305 (40.6) |
| Married | 45 (11.6) | 128 (33) | 159 (40.7) | 7 (1.8) | 6 (1.5) | 7 (1.8) | 10 (2.6) | 11 (2.8) | 3 (0.8) | 13 (3.4) | 389 (51.8) |
| Widow | 0 (0) | 22 (53.7) | 15 (36.7) | 1 (2.4) | 0 (0) | 0 (0) | 1 (2.4) | 0 (0) | 1 (2.4) | 1 (2.4) | 41 (5.4) |
| Divorced | 15 (2) | 15 (2) | 15 (2) | 15 (2) | 15 (2) | 15 (2) | 15 (2) | 15 (2) | 15 (2) | 15 (2) | 15 (2) |
| Drug addiction | |||||||||||
| Yes | 22 (17.7) | 40 (32.3) | 35 (28.2) | 1 (0.4) | 5 (4) | 14 (11.3) | 1 (0.4) | 1 (0.8) | 2 (1.7) | 4 (3.2) | 125 (16.6) |
| No | 75 (12) | 197 (31.5) | 229 (36.6) | 13 (2.1) | 9 (1.4) | 4 (0.6) | 16 (2.6) | 17 (2.7) | 6 (1) | 59 (9.4) | 625 (83.3) |
| FH of psychiatric disorders | |||||||||||
| Yes | 28 (13.5) | 74 (35.3) | 69 (33.2) | 3 (1.4) | 3. (1.4) | 3 (1.4) | 1 (0.2) | 0 (0) | 0 (0) | 28 (13.5) | 209 (27.8) |
| No | 69 (12.8) | 163 (30.1) | 194 (35.9) | 11 (2) | 12 (2.2) | 15 (2.8) | 16 (3) | 18 (3.2) | 8 (1.5) | 35 (6.5) | 541 (72.1) |
| Psychiatric Disorders | No (%) |
|---|---|
| Psychotic | 98 (13) |
| Mood | 236 (31.5) |
| Anxiety | 264 (35.3) |
| Somatoform | 14 (1.8) |
| Personality | 15 (2) |
| Drug abuse | 18 (2.5) |
| Cognitive impairment | 16 (2.2) |
| Psychiatric counseling | 18 (2.5) |
| Sexual dysfunction | 8 (0.6) |
| Dissociative disorders | 63 (8.5) |
| Variable | No (%) |
|---|---|
| Psychotic disorders | |
| Schizophrenia | 20 (20.4) |
| Psychotic disorder | 78 (79.6) |
| Mood Disorders | |
| Depression | 150 (63.6) |
| Bipolar | 86 (36.4) |
| Anxiety disorders | |
| Obsessive-compulsive disorder | 53 (20.1) |
| Generalized anxiety disorder | 160 (60) |
| Post-traumatic stress disorder | 26 (9.8) |
| Panic disorder | 25 (9.5) |
| Dissociative disorders | |
| Autism | 5 (8) |
| Tic | 13 (20.6) |
| Narcolepsy | 6 (9.5) |
| Mentally retarded | 12 (19) |
| ADHD | 27 (43) |
5. Discussion
This is the first study conducted by full, structured psychiatric interviews with a representative sample of patients referring to a psychiatric clinic in Lorestan. The results showed anxiety (35.3%) and mood disorders (31.5%) were the most common psychiatric disorders. The results of this study confirm the findings of prior epidemiological studies in various respects (12). This study was closely in agreement with the studies by Noorbala in Tehran (16), Ahmadvand in Kashan (15), Preville (17) in Canada, and Simsek in Turkey (18). The results of another study confirmed the high prevalence of anxiety disorders and mood disorders in Iran. Also, the results showed an increasing rate of psychological distress, including depression, in recent years (19). We showed that major depression and generalized anxiety disorder were the most common anxiety and mood disorders, and autism and narcolepsy were the least frequent disorders in Lorestan.
The results showed that most studied subjects were women and the prevalence of psychiatric disorders was higher in females. A review of studies conducted in the world and Iran confirms the results of this study that women are more prone to psychiatric disorders than men. The high prevalence of psychiatric disorders in women compared to men can be due to gender roles, biological factors, environmental factors, job stress, limitation of satisfaction, and lack of social participation in Iran's current population (12, 20, 21). Furthermore, most females are bound to their social roles as housewives; even when a woman works outside the home, she remains a housewife.
Consistent with other studies, the results of this study showed that psychiatric disorders were more common in housewives and unemployed men than in employed men and women (1, 9, 15). The probable causes of this problem are low income, unemployment stress, restrictions on social interactions, lower chance of marriage, and reducing diversity in the lives of housewives and unemployed ones. The results of this study showed that the prevalence of psychiatric disorders was higher in married people than in single individuals.
Data in this investigation showed that the prevalence of psychiatric disorders was higher in married ones than in single ones. These results are similar to the results of other studies conducted in Iran (2, 15). Most studies in the world show that the prevalence of psychiatric disorders is higher in single people than in married individuals (9). The higher prevalence of psychiatric disorders in married people in Iran can be due to marital problems and sexual dysfunction (22). Also, financial problems are much more for married couples than for single people.
In this study, illiterate and primary-educated people (52.4%) showed a higher prevalence of psychiatric disorders, while people with an academic education (20.6%) had a lower prevalence; these results are similar to the results of other studies (2, 15). Social and cultural limitations and the inability to use the correct mechanism in the face of stress are the reasons for the higher prevalence of psychiatric disorders in people with low education. The lowest incidence of psychiatric disorders was among people with postgraduate degrees, which confirms the findings of most studies conducted in Iran (20).
Despite some improvements in recent years, mental health services have not yet been optimally developed in Lorestan, and there are not many qualified mental health professionals in this province. We need rapid responses to the problem by taking new actions in mental health approaches, programs, organizations, new consultation centers, mental therapeutic services, and support in this region. Considering the high prevalence of anxiety and mood disorders relative to other diseases, the public health authorities of the province need to warrant necessary measures including mental health promotion policies to improve mental health status and propose ways to develop stressful factors and improve the quality of life. Women, unemployed people, housekeepers, and people with lower education are at a higher risk of psychiatric disorders. The establishment of centers for assessment and diagnosis of high-risk groups and a referral system to counseling and psychiatric clinics is essential.
In conclusion, the majority of the patients referring to the psychiatric clinic suffered from mood and anxiety disorders. Therefore, the public health authorities of the province need to take steps to warrant necessary measures, including mental health promotion policies, to improve the mental health status and prevent anxiety and mood disorders.