1. Background
Since surgical interventions often cause damage to tissues, which in turn stimulates the central nervous system, postoperative pain is unavoidable (1). A study performed in the Netherlands on 1490 hospitalized patients reported that also there was a protocol for treatment of pain, 41% of patients had moderate to severe pain on the day of the surgery, and for about 15% of them, a moderate to severe pain was continuing to the fourth day of surgery (2). Postoperative pain may lead to adverse physiological consequences (3), that if left untreated, cause complications such as respiratory distress, sympathetic system activation, increased blood coagulability (4), increased heart rate, respiration, and sweating, and reduced arterial oxygen, increased levels of aldosterone and antidiuretic hormone, water and sodium retention and, in general, reduced urine output (5), skin irritation, restlessness, and pupillary dilatation (6), delayed recovery, impairment of the immune function, movement, and sleep pattern, and loss of appetite (7). Furthermore, postoperative pain also affects mental health, mainly increased fear, anxiety, feelings of helplessness, and hopelessness (8).
Based on the aforementioned consequences of untreated post-surgery pain, for whatever cause, caregivers have the responsibility of being aware of stressful factors involved in hospitalization as well as safe and effective interventions to eliminate or reduce stressors. Besides, they should pay special attention to non-traumatic care (3). In this line, controlling or reducing pain after appendectomy is one of the main pillars of postoperative nursing care. Although the administration of mild narcotics and tranquilizers can reduce pain, they also cause adverse effects, such as drowsiness, nausea, vomiting, constipation, respiratory system inhibition, central nervous system depression, addiction, fatigue, and confusion or restlessness (8, 9). Acknowledging the widespread importance of acute post-surgical pain has led to the development of many medical-social strategies and, in particular, new regulatory standards to evaluate and manage acute pain. A major emphasis of these new standards is routine pain assessment, or the so-called fifth vital sign (2).
In a review study, Nazemzadeh et al. reported the effectiveness of various programs intended to reduce the pain and anxiety caused by painful and anxiety-provoking procedures at different age groups. Although few studies have investigated the effects of such interventions, in general, they are safe, non-invasive, cost-effective, and practicable strategies that can be implemented independently (10).
In recent years, non-pharmacological approaches under the title of complementary and alternative medicine have attracted the attention of both patients and healthcare providers as an adjuvant treatment. One special and under-study approach of this area is aromatherapy, which uses methods such as the inhalation of vapors or absorption of essential oils by the skin to treat or alleviate emotional and physical symptoms (9).
Early clinical studies have suggested that aromatherapy has beneficial effects, such as reducing the perception of stress, pain, and depression (9). In this line, some essential oil extracts (e.g., lavender, jasmine, rosemary, rose, geranium, and chamomile) are used to treat symptoms such as pain, anxiety, etc (9). Owl pour et al. investigated the effects of aromatherapy on postoperative cesarean section pain and reported that aromatherapy could significantly reduce pain (11). Nevertheless, the therapeutic use of aromatherapy remains controversial due to the lack of scientific evidence about its effectiveness and safety (9).
Lavender is an aromatic herb used in aromatherapy with considerable analgesic effects, which has attracted much attention in recent years (12). The linalool and linalyl acetate present in this plant are capable of stimulating the parasympathetic system. Linalyl acetate also has narcotic properties, and linalool acts as a sedative (13, 14). Review studies have reported that evidence are not sufficient to decide whether aromatherapy can reduce pain and psychological suffering (15). A study by Bagheri-Nezam et al. showed that patients undergoing lavender aromatherapy experienced more pain relief compared to the control group (16).
2. Objectives
Since after surgery, most patients require narcotics and untreated pain may cause complications during the patient's recovery, on the one hand, and regarding the potential effects of aromatherapy reported by various studies conducted all around the world, on the other hand, aromatherapy can be recommended as a new and easy alternative to reduce postoperative pain, which in turn can reduce patients’ demand for narcotic drugs. In this line, the current study aimed to evaluate the effect of French lavender aromatherapy using the inhalation technique on reducing pain and decreasing patients’ need for narcotic drugs after appendectomy surgery.
3. Methods
3.1. Study Design and Samples
In this single-blind randomized clinical trial, 120 patients undergoing acute abdominal surgery in the Shohadaye Assayer Hospital in Khorramabad from 2009 to 2010 are investigated. Participants were recruited non-randomly and consecutively. For the purpose of homogeneity of the research sample concerning gender, age, type of operation, prescribed medicine, and type of surgery (elective, emergency, or urgent), participants were divided into three groups of intervention, placebo, and control using the blocked randomization method.
3.2. Inclusion Criteria
The inclusion criteria were being aged 18-65 years and having abdominal surgery with a duration of operation of less than 90 minutes.
3.3. Exclusion Criteria
The exclusion criteria were drug addiction, suffering from chronic diseases or diabetes, having more than one surgery, having cancer diagnosis, history of eczema or allergy to herbs, a history of migraine or chronic headaches, suffering from a hemorrhagic disease or active mental illness, or having disorders of the olfactory system.
3.4. Blinding
As the researcher was not aware of the type of scent used for each patient, the present study can be considered as a single-blind study.
3.5. Randomization
The blocked randomization method was used (available at https://www.sealedenvelope.com/simple-randomiser/v1/5), such that 5 blocks of 10 and 10 blocks of 7 were selected, and the patients were divided into the three groups of treatment (40 patients who received lavender), control (40 patients who received no treatment), and placebo (40 patients who received almond oil).
3.6. Intervention
The first pain assessment was performed using the Visual Analogue Scale (VAS) 6-8 hours after the surgery, at least three hours after the administration of analgesic medication (pain 1). Lavender is a flowering plant that belongs to the Labia tea family, which its leaves and green parts contain volatile essential oils. French lavender has a dark purple color. It also grows in some regions of Iran. Lavender flowers from early to late July depending on the region. After collecting the French species of the plant, the essential oil was prepared by a chemist from the flowers of the plant in pure form. Then the oil was combined with one-tenth of sweet almond oil to reduce the volatility of the essential oil and adding aroma (sweet almond oil does not have any aroma). Afterward, the resulting essential oil was kept at a temperature of -20°C. The intervention group received two drops of this mixture on a handkerchief with a dropper. The handkerchief was kept at a distance of 2.5 to 5 cm from the nose of the patient, and the patient was asked to inhale the aroma for 3 minutes. After half an hour, the pain was measured again (pain 1.1). The placebo group received two drops of almond oil on a handkerchief, then the pain was measured using the VAS. It worth noting that patients of each group were hospitalized in different rooms. In the second stage, after 6 to 8 hours, the pain was measured again (pain 2), and the intervention was repeated similar to stage one. Afterward, after half an hour, the procedure was repeated (pain 2.2). The third intervention was provided 6-8 hours after the second stage (pain 3), and the level of pain was measured half an hour later (pain 3.3).
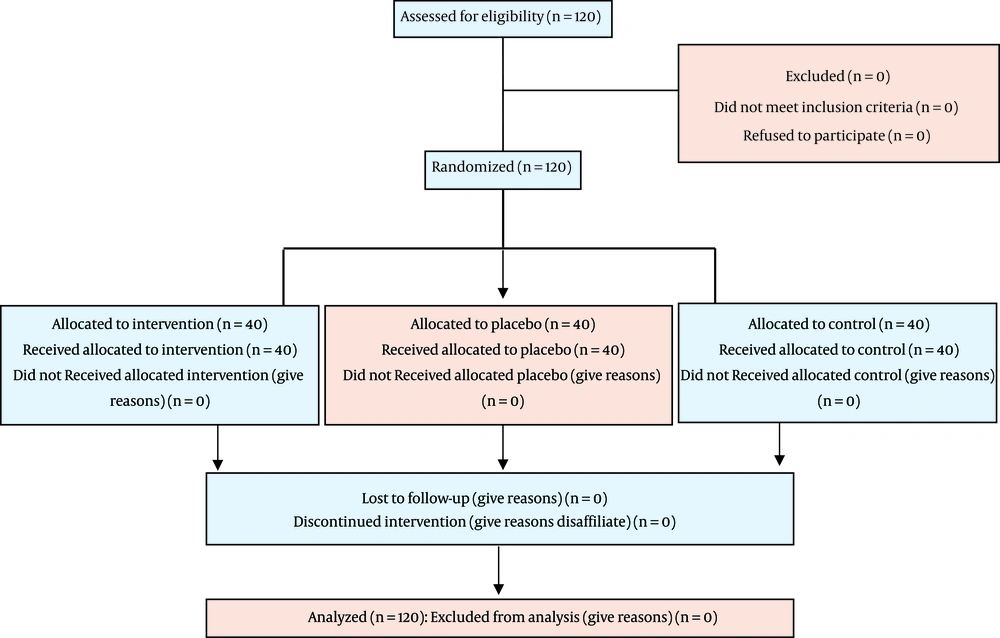
Eventually, participants were evaluated concerning the amount of received pain medication. Analgesic drugs refer to narcotic and non-opioid analgesics that had been administered after the patients had left the recovery unit and in the first 24 hours in the post-surgical ward. The dose, type, and method of administration of drugs during the first 24 hours after surgery were recorded (Figure 1).
3.7. Data Collection
General information (including age, sex, surgeon’s name, pre-operative discontinuation of medications, and pain tolerance threshold) were collected using a questionnaire. The pain was measured using the Visual Analogue Scale. Received analgesic drugs within the first 24 hours after surgery were also obtained from the patient's medical records. Hence, data were collected using a demographic questionnaire, VAS, and medical records.
3.8. The Reliability and Validity of the Data Collection Instruments
The VAS is a 10 cm line designed to measure the pain, ranging from zero (“no pain”) to 10 ("severe pain and anxiety), which the patient, based on his/her understanding, selects a point on the scale. With higher scores indicating greater pain intensity. To measure the changes in pain, values obtained from each survey can be compared to see whether the pain has intensified or decreased. The VAS was designed by Lin et al. to assess post-operation pain and anxiety (17). Several studies have used the VAS to measure pain, such as Warth et al. (18), Korhan et al. (19), Li et al. (20), Amiri Mellah et al. (21), and Ajori et al. (22). The face and content validity of the pain changes are confirmed by Ottaviani et al. (23) and Hekmat Afshar et al. (24).
The reliability of the VAS has been demonstrated by Rafieyan et al. (25) in a preliminary study using the split-half method and the Spearman-Brown test (r = 0.83). Cronbach's alpha coefficient was used to reassess the reliability. In a pilot study, a sample of 20 subjects was selected separately and was divided into two groups (each with 10 individuals). Then, the collected data were analyzed using the VAS. Cronbach's alpha coefficient was greater than 0.83.
3.9. Statistical Analyses
Data were analyzed by SPSS version 16 using the descriptive statistics as well as the ANOVA and Kruskal-Wallis tests. Statistical significance was considered when P value < 0.05.
3.10. Ethical Considerations
This study was approved by the Center for Clinical Trials (IRCT20151003024312N3). Besides, it’s confirmed by the Ethics Committee of the Lorestan University of Medical Sciences (No. 13211/200).
4. Results
4.1. Homogeneity of the Demographic Data
In this study, 120 patients undergoing appendectomy were divided into three groups. The demographic characteristics of the three groups are presented in Table 1, which shows similar distributions of participants. No significant difference was found concerning the surgeon, drug discontinuation, and pain tolerance level. Regarding confounding variables such as preoperative drug administration, dose and administration method, the process of anesthesia, as well as other demographic variables (e.g. history of disease and surgery) no significant difference was found between the three groups (P > 0.05) (Table 1).
| Variable | The intervention group (n = 40) | The placebo group (n = 40) | The control group (n = 40) | P Value |
|---|---|---|---|---|
| Age, Mean ± SD | 27.62 ± 8.97 | 26.90 ± 9.41 | 28.02 ± 8.20 | 0.84a |
| Sex, No. (%) | 0.96b | |||
| Male | 21 (52) | 20 (50) | 20 (50) | |
| Female | 19 (48) | 20 (50) | 20 (50) | |
| The Surgeon, No. (%) | 0.90c | |||
| A | 18 (45) | 14 (35) | 15 (37.5) | |
| B | 12 (30) | 15 (37.5) | 15 (37.5) | |
| C | 10 (25) | 11 (27.5) | 10 (25) | |
| Drug Discontinuation, No. (%) | 0.44c | |||
| Yes | 27 (67.5%) | 29 (72.5%) | 24 (60%) | |
| No | 13 (32.5%) | 11 (27.5%) | 16 (40%) | |
| Pain Tolerance level, No. (%) | 0.78c | |||
| Poor | 9 (22.5%) | 7 (17.5%) | 5 (12.5%) | |
| Moderate | 27 (67.5%) | 27 (67.5%) | 30 (75.5%) | |
| Good | 4 (10%) | 6 (15%) | 5 (12.5%) |
The Demographic and Background Characteristics of the Participants of the Three Groups
The Kolmogorov-Smirnov was used to test for a normal distribution. The results showed that the variables of age, the severity of pain (as measured in various stages), the time of receiving the first painkiller, administration method, and the dosage of analgesic drugs had a normal distribution. Accordingly, depending on the distribution of data the ANOVA and Tukey’s test (for parametric data) and the Kruskal-Wallis test (for non-parametric data) were used to analyze the data.
4.2. The Pain Intensity
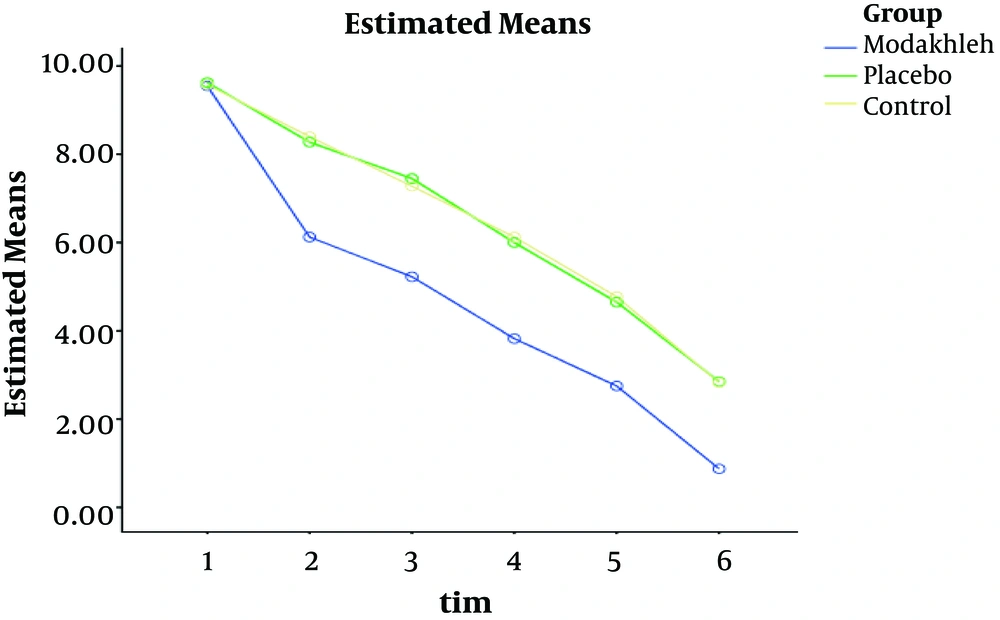
The results of the one-way ANOVA showed no statistically significant difference between the three groups concerning the severity of the pain before providing the intervention (Pain 1) (P = 0.90). However, a significant difference was found between the three groups concerning the severity of pain after providing the intervention (pain 1.1, 2, 2.2, 3, and 3.3) (P < 0.001) (Table 2 and Figure 2).
| Group | Intervention, (n = 40), (Mean ± SD) | Placebo, (n = 40), (Mean ± SD) | Control, (n = 40), (Mean ± SD) | F | P Value |
|---|---|---|---|---|---|
| Pain 1 | 9.55 ± 0.81 | 9.62 ± 0.74 | 9.57 ± 0.67 | 0.1 | 0.9 |
| Pain 1.1 | 6.12 ± 0.91 | 8.27 ± 0.98 | 8.40 ± 0.90 | 75.08 | < 0.001 |
| Pain 2 | 5.22 ± 0.99 | 7.45 ± 0.95 | 7.27 ± 1.01 | 62.37 | < 0.001 |
| Pain 2.2 | 3.82 ± 0.90 | 6.00 ± 1.30 | 6.12 ± 1.18 | 51.45 | < 0.001 |
| Pain 3 | 2.75 ± 0.58 | 4.65 ± 1.49 | 4.77 ± 1.42 | 33.56 | < 0.001 |
| Pain 3.3 | 0.87 ± 1.01 | 2.85 ± 1.59 | 2.82 ± 1.61 | 24.9 | < 0.001 |
The Distribution and Comparison of the Mean and Standard Deviation of the Perceived Pain Intensity in the Participants of the Three Groups During the Intervention
The results of the Tukey test also demonstrated a significant difference among the three groups concerning the pain intensity (1.1, 2.2, 3.3), which can be attributed to the significant differences between the groups. There was no significant difference between the placebo and control groups.
In the control group, however, the amount of pain was decreased, which can be due to the passage of time, but this decrease was not statistically significant.
The results of the repeated measures test indicated that the significant difference between the two groups of intervention and placebo is due to the significant decrease in perceived pain severity in the intervention group (Table 3).
| Pain | 1.1 | 2 | 2.2 | 3 | 3.3 |
|---|---|---|---|---|---|
| Group | Intervention Placebo | Intervention Placebo | Intervention Placebo | Intervention Placebo | Intervention Placebo |
| Pain Reduction | -2.25-0.17 | -2.02-0.12 | -2.27-0.17 | -2.00-0.17 | -1.92-0.02 |
| P Value | < 0.0001, 0.38 | <0.0001, 0.58 | <0.0001, 0.51 | < 0.0001, 0.54 | < 0.0001, 0.93 |
The Amount and the Comparison of Pain Reduction Between the Intervention and Placebo Groups During the Intervention
As shown in Figure 2, there was a significant difference concerning changes in the mean pain scores of the three groups. In the intervention group, after each intervention, a significant decrease was occurred in the mean score of pain compared to the placebo and control groups (< 0.001). However, before providing the intervention, there was no significant difference between the mean scores of pain in the three groups (P > 0.05).
4.3. Analgesics
Regarding the effect of aromatherapy intervention on the amount and type of analgesics received, the results of the present study indicated no significant difference between the three groups concerning the type of analgesics, based on the Kruskal-Wallis test (P = 0.17). Morphine, pethidine, heptidine, and pentazocine were used as sedatives for participants of all three groups. The Kruskal-Wallis test revealed a significant difference between the three groups (P < 0.001) concerning the dosage of the analgesics, administration method of the analgesics (intravenous, muscular, and oral) (P < 0.001), and the time of the first administration of the drug (P < 0.001). The total amount of administered narcotics during the first 24 hours after surgery was converted to mg morphine to facilitate better comparisons.
The mean and the standard deviation of the received dose of the analgesics in the first 24 hours after the surgery based on mg of morphine was 12.14 ± 30.5 in the intervention group, 18.87 ± 17.11 in the placebo group, and 39.12 ± 35.57 mg in the control group.
The results of the one-way ANOVA (df = 2, F = 13.26) indicated a significant difference between the three groups concerning the dose of the analgesic drug (Table 4).
| Group Statistic | Intervention | Placebo | Control | Significance level |
|---|---|---|---|---|
| Mean | 12.3 | 18.88 | 39.12 | P < 0.001 |
| Standard Deviation | 14.5 | 17.11 | 35.57 | |
| Minimum | 1 | 5 | 5 | |
| Maximum | 50 | 60 | 155 |
The Mean and Standard Deviation of the Doses of Narcotic Analgesics Administered after the Surgery in mg of Morphine Separated by Group
Additionally, the results of the Tukey test showed that the significant difference between the three groups concerning the received dose can be attributed to the difference between the intervention and control groups and the intervention and placebo groups. There was no significant difference between the control and placebo groups (Table 5).
| Group 1 | Group 2 | Mean Difference | Standard Error | Significance Level |
|---|---|---|---|---|
| Intervention | Placebo | -20.25 | 5.42 | 0.001 |
| Intervention | Control | -26.82 | 5.42 | P < 0.001 |
| Placebo | Control | -6.57 | 5.42 | 0.44 |
The Comparison of the Mean Analgesic Doses Administered to the Participants after Surgery
5. Discussion
Based on the findings, the lowest level of pain intensity was observed in the intervention group. Therefore, it can be concluded that aromatherapy was effective in significantly declining pain intensity. Consistent with the findings of the present study, Kim et al. investigated the effect of smelling lavender (Lavandula) on the levels of injection-induced stress and pain and reported similar results (26). Another study on the effects of inhaling aromatherapy with Rosa damascene mill or pelargonium grave lens on postoperative pain intensity relief in pediatrics also reported similar results (27).
When a fragrance is inhaled, the molecules of the substance are transmitted through the olfactory system to the limbic system in the brain, and the center responds to the stimulation, which causes psychological effects (9). It seems that using lavender in aromatherapy can be attributed to its calming, analgesic, and anti-contraction effects through the neurological system (28).
In the present study, a significant difference was observed concerning the intensity of pain between the intervention group and the group that received routine procedures among patients undergoing appendectomy, which is consistent with the results of Alavi et al. In their study, Alavi et al. investigated the effects of inhaling lavender extract during childbirth, by pouring one cc of lavender essential oil on a handkerchief and keeping it near the nose of the mother, and reported a significant reduction in pain intensity 30 and 60 minutes after administration (29). Moreover, a study by Niaz-Hadi et al. reported that using lavender essential oil could significantly reduce the pain after cesarean section, which confirms the results of the present study (30).
However, there are studies in which their findings are not consistent with the present study. For example, Kim et al. reported that the inhalation of a 2% Lavandula solution after surgery in patients undergoing breast biopsy did not change the pain score (31). Grunebaum et al. showed that Lavandula aromatherapy did not affect the perception of pain during Botox injection, however, when exposed to the scent of Lavandula, a significant increase was observed in parasympathetic activity (32). Martin also stated that inhalation of scents had no effect on pain relief, and even those who have pain are more likely to feel pain when they face different scents, whether pleasant or unpleasant (33). These controversial results indicate the necessity of more detailed and comprehensive studies in this area.
Besides, based on the findings, those in the intervention group consumed a significantly lower amount of analgesics. Kim et al. showed that aromatherapy with lavender reduced the administration of analgesics in patients undergoing laparoscopy and also reduced the administration of morphine in the intervention group (19), which is consistent with the findings of the present study. In general, there are several studies with similar results, and there are studies with different findings. This discrepancy can be attributed to various factors such as the research population and applied methodology (e.g. the type, dose, and duration of using scent).
In conclusion, The importance of managing and controlling pain is not limited to pain relief. Apart from pain relief, pain management is associated with reduced complications that caused by pain, frequent requests for opioid analgesics, and the length of hospitalization. On the other hand, severe pain not only has negative effects on the performance of patients but also increases the risk of further problems such as cardiovascular diseases. Nowadays, the use of conventional and traditional therapies is an integrated part of professional medical practices, with the main intention of promoting patients’ comfort. This study demonstrated that aromatherapy with lavender essential oil is an easy, inexpensive, and safe alternative to reduce the pain and the need for sedatives after appendectomy.
It worth noting that many factors contribute to the perception of pain, pain relief after an operation, and the requests for analgesics. In this line, achieving controversial results seems to be logical and justifiable. According to Howard and Hughes, participants’ attitudes towards aromatherapy can strongly influence the outcomes (34). Therefore, it seems that performing numerous high-quality studies in this field can lead researchers to more accurate results.
5.1. Limitations
The main limitation of this research was the lack of control over the personal biochemical characteristics of participants (e.g. pain threshold and the ability to tolerate the pain). To overcome this limitation, the participants were asked to report their own pain tolerance levels and this variable was assessed using a three-point Likert scale (i.e. good, moderate, and poor). The other important factor is that the time gap between the surgery and the intervention, which plays a crucial role as a confounding factor.
5.2. Application of the Findings
Currently, to reduce the postoperative pain, first narcotic drugs and then non-steroidal anti-inflammatory drugs (e.g., diclofenac) are used. Since various studies have reported that most of the Iranian patients are not satisfied with the relief, they get from postoperative pain and considering the severe side effects of narcotics and their high costs, finding an effective alternative is of crucial importance. In this line, by combining the results of such studies, healthcare providers can make better decisions regarding managing postoperative pain.
5.3. Suggestions for Further Research
It is recommended that similar studies:
Be conducted on different groups of patients who undergo surgery.
Be conducted with larger sample sizes and at longer durations.
Be conducted to assess cost-benefits.