1. Background
Laryngopharyngeal Reflux (LPR) is a condition in which gastric content reflux into the larynx and pharynx. It is one of the extraesophageal manifestations of gastroesophageal reflux disease (GERD), involving the laryngeal region (1). The laryngopharyngeal epithelium is more susceptible to reflux-related tissue injury than the esophageal epithelium (2). These injuries result in a wide constellation of symptoms commonly seen as voice changes, odynophagia, and lump sensation in the throat (3, 4). The prevalence of LPR in Indian women in north India is reported to be approximately 10% (5).
Recently, the role of vitamin D is being evaluated as one of the factors responsible for GERD and LPR. Approximately more than two-thirds of Indian females are found deficient in vitamin D, with a prevalence of 64.06% (6). Hypovitaminosis D is a known causative factor for muscular sphincter relaxation and contraction, resulting in delayed muscle relaxation and longer times to reach peak muscle contraction (7, 8). This mechanism affects the tone of the lower esophageal sphincter, thereby resulting in reflux.
On the basis of the above pathophysiology, we hypothesized whether severe vitamin D deficiency might result in increased LPR symptoms in Indian females. This study aimed to prove or reject this hypothesis.
2. Objectives
The objective was to find out the prevalence of LPR in the severe vitamin D deficient Indian female population.
3. Methods
This descriptive observational study was carried out at a multispecialty polyclinic in North India over a period of one year between May 2019 to May 2020 after approval from Institutional Ethics and Scientific Committee. A pilot study was conducted during the month of March to April 2019, in which 34 consecutive females with Vitamin D levels below 20 ng/ml were recruited. Four out of these 34 females showed a score of more than 13 on the reflux symptom index (RSI) and taken as symptomatic for LPR. The disease proportion in reported patients was found to be 11.7% based on this pilot study. These data were used in sample size calculation. The sample size was calculated using the following formula:
Where n was the sample size, Z was the statistic value corresponding to the level of confidence, P was considered the prevalence (obtained from the pilot study conducted), and d is the precision. Considering a 95% level of confidence and 5% (d) precision, the statistical corresponding value of Z was estimated to be 1.96. The value of n was calculated as equal to 158. Considering dropouts, an adequate sample size of 185 was taken.
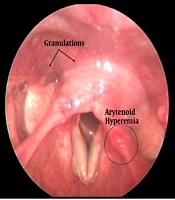
All females referring to the general outpatient department (OPD) with vitamin D levels below 20 ng/ml and willing to participate in the study were included after obtaining consent. Females reporting to OPD for antenatal care, who were on long-term steroids and/or proton-pump inhibitors (PPI) and with any history of laryngeal manipulation, were excluded from the study. All participants were divided into two groups based on age; less than 25 years and more than 25 years and based on vitamin D levels, less than 10 ng/ml as severe deficiency, and 11-20 ng/ml as mild to moderate deficiency. The study participant’s frequency of LPR symptoms and its severity were subjectively assessed using RSI described by Belafasky et al. (9), as shown in Figure 1. The severity of nine commonly encountered LPR symptoms was assessed, and scores were given using a five-point Likert scale checklist. The total score ranged between 0 and 45 for each participant. A score of less than 13 was defined as no LPR symptoms, a score between 13 to 29 as mild to moderate symptoms, and 30 or more as severe LPR symptoms.
The reflux symptom index adopted from Belafsky et al.; the validity and reliability of the reflux finding score are shown (9).
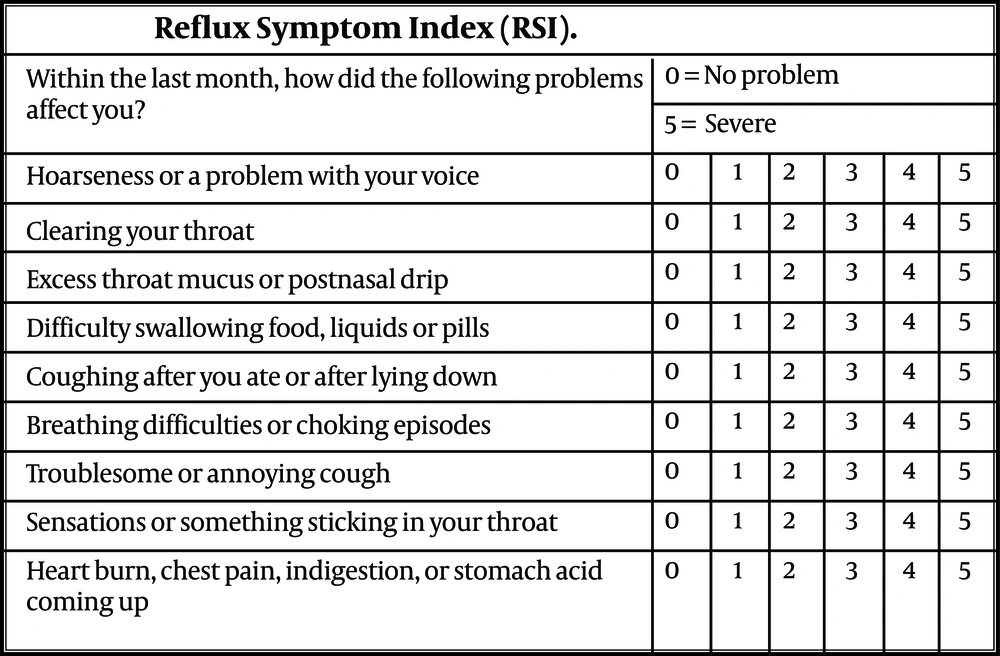
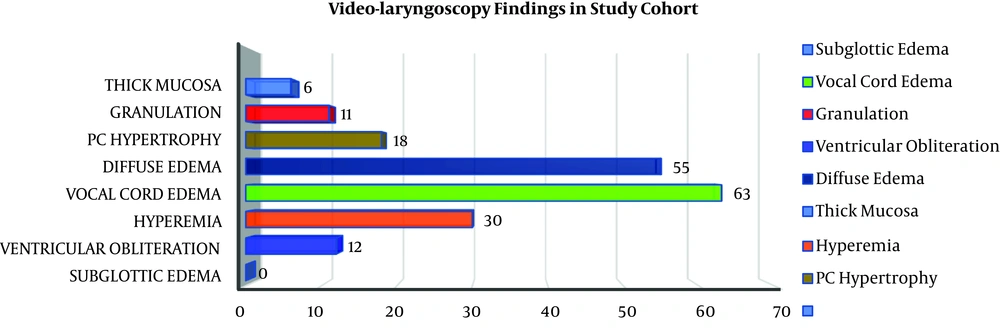
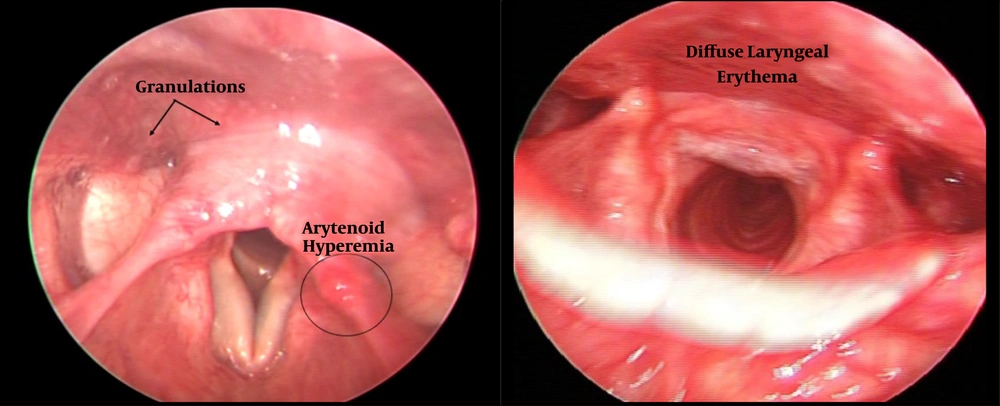
All participants with RSI score more than 13 were subject to a 70-degree rigid video-laryngoscopy, and the findings were recorded. The reflux finding score (RFS) was given to each positive finding, as described by Belafasky et al. (9), as shown in Figure 2. In fact, RFS is an eight-item clinical severity rating score based on laryngoscopy findings. The participants who did not undergo laryngoscopy owing to RSI less than 13 were given an RFS of 0. the patients were then divided into three groups based on total RFS. A score of 0 was defined as no disease, RFS 1 to 10 as a mild disease, and RFS more than 10 as moderate to severe disease. All observations were recorded by the same investigator to rule out observer bias.
Reflux finding score adopted from Belafsky et al.; the validity and reliability of the reflux finding score are shown (9).
The data were analyzed descriptively with Microsoft Excel and SPSS version 21 using appropriate tests.
4. Results
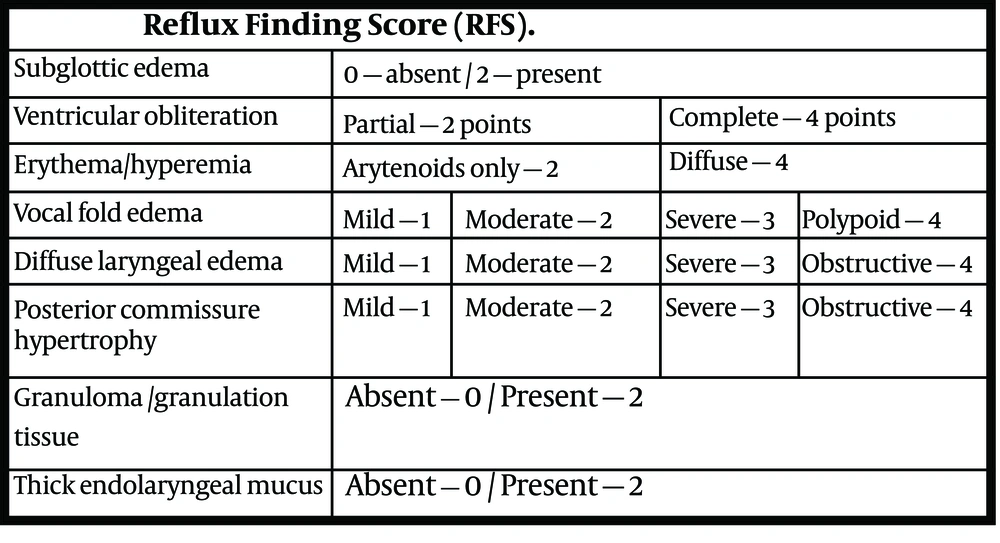
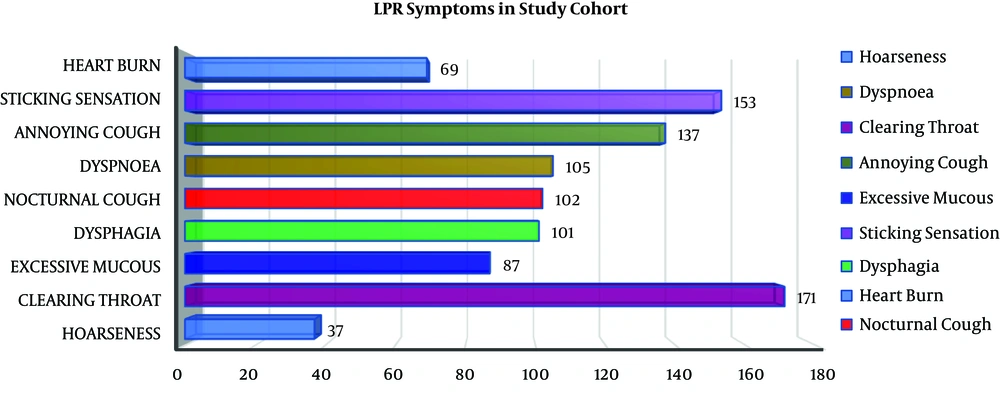
Data pertaining to 185 females who had deficient levels of vitamin D (less than 20 ng/ml) were collected. The mean age of the study population was 38.71 (± 11.834) years and ranged between 6-82 years. Moreover, 92% (n=170) of our study patients aged more than 25 years and 8% (n=15) aged less than 25 years. The mean vitamin D level was 9.87 (± 3.425) ng/ml. Also, 74% (n=137) of patients had severe deficiency (vitamin D level ≤ 10ng/ml) and 26% (n=48) had mild to moderate deficiency (vitamin D level between 11-20ng/ml). LPR symptoms were present in 43% (n=79), while it was absent in 57% (n=106) of the patients. The mean RSI was 14.54 (± 10.353). The commonest symptom was clearing throat (92.4%) followed by sticking sensation in throat (82.7%), as shown in Figure 3. The mean RFS was 1.77 (± 3.069). The commonest video-laryngoscopy finding was hyperemia (63%) followed by diffuse oedema (55%) as shown in Figures 4 and 5. Based on RSI and RFS scores, mild to moderate LPR (scores between 13-29) was present in 34% of the patients (n=63), while severe LPR (scores between 30-42) was seen in 9% of the patients (n=16). In our study, no significant correlation was established (P value > 0.05) between the severity of vitamin D deficiency and RSI as well as RFS. The prevalence of LPR in our study population was 43%.
5. Discussion
The laryngopharyngeal complex is made of bone, cartilage, and mucosa. Given its similarity to the remaining musculoskeletal structures and the known vitamin D deficiency-induced muscular dysfunction, a hypothesis was made that vitamin D deficiency might lead to LPR. A higher reflux index score was hypothesized in the severe vitamin D deficient group. We could not demonstrate a statistically significant correlation (P value > 0.05) between the severity of vitamin D deficiency and RSI as well as RFS. A similar effort was made in 2016 by Hamdan et al. (10), who investigated the effect of vitamin D on vocal tract symptoms in a limited sample size. They used vocal tract discomfort scores in their methodology to quantify the frequency and severity of vocal tract symptoms in the vitamin D deficient group and found no significant difference. Despite the limited background knowledge on the subject due to the paucity of research, we could draw significant conclusions with an appropriate sample size and validated scoring system.
Various literature shows that the prevalence of LPR in the general population varies from 10%-50% (11). A study done by Nizamma et al. (12) showed a prevalence of 18% in Bosnia; however, Mishra P et al. (5) found a prevalence of 11.2% in Indian population. In our study population, we found a prevalence of LPR of 43% in females suffering from hypovitaminosis D. However, this study failed to demonstrate any statistically significant correlation between vitamin D deficiency and LPR.
In conclusion, vitamin D deficiency is a well-known cause of musculoskeletal dysfunction, and hypothetically it can cause LPR by altering the function of the lower esophageal sphincter. Only limited studies with a limited sample size investigated the effect of vitamin D deficiency and LPR. This study was done to evaluate the effect of vitamin D deficiency in females on RSI and RFS in LPR. The results of this study indicate that vitamin D deficient females did not have any significant rise in LPR symptoms and RFS.