1. Background
In recent years, especially in the twentieth century, advances in the care and treatment of military trauma have increased (1). Most Iranian veterans suffer from physical problems such as eye problems, spinal cord injuries, lower limb amputations, and zinc deficiency (2). The results of some systematic review and meta-analysis studies indicate that Iranian veterans have a low quality of physical and mental life, and most psychological injuries have been reported among chemical veterans (3). While there is extensive research literature on the physical health of war-torn populations worldwide, the psychological effects of war on survivors are not yet well understood (4). Among the most important of these consequences are mood problems and anxiety that have a negative impact on the personal and social life of war survivors (5). Some studies show that the prevalence of depression in all Iranian veterans is 0.71%. Also, the prevalence and severity of depression in chemical veterans is higher than those in non-chemical veterans (6). In this regard, review of the literature shows that among war survivors, mood and anxiety problems are common, and these psychological problems are associated with numeous problems such as suicidal thoughts and suicide attempts (7), post-traumatic stress disorder (8, 9), and personality disorders (10). Untreated psychological symptoms such as depression and anxiety in the long run, except for their own specific issues, can affect the process of treatment follow-up and medical orders in war-disabled people, exacerbate illness, cause other physical problems, and reduce the effectiveness of treatment, and in turn, lower the survival and longevity of these people (11, 12).
For many years, physicians have used a wide range of methods to relieve the pain of war veterans and survivors. Nowadays, psychological methods are used both individually and in combination with medical methods in the treatment and rehabilitation of war survivors, and research shows the high efficiency of psychological therapies (13, 14). Among these, cognitive-behavioral therapy has a strong theoretical basis, and several studies have confirmed its effectiveness in a wide range of psychological issues and different patients (13-16). The overall goal of cognitive-behavioral therapy is to replace non-adaptive cognitions, emotions, behaviors, and coping skills with adaptive states for clients (17). Recabarren et al. (15) reported that the quality of life and the rate of psychological symptoms (i.e., anxiety, depression, and interpersonal sensitivity) improved in people receiving group cognitive-behavioral therapy compared to those on the waiting list. The study of Bock et al. (16) also showed the positive impact of this treatment on the quality of life, resilience, and executive function of chronic patients.
2. Objectives
According to the high prevalence of mood problems and anxiety among war survivors in Iran, this study was conducted to determine the impact of group cognitive-behavioral therapy on the anxiety and depression of war invalids (war veterans).
3. Methods
3.1. Study Design and Samples
This quasi-experimental study was conducted with a pre-test and post-test design and a control group. The statistical population of the study included all disabled men from the Iran-Iraq war who visited Sadra Psychiatric Hospital in Tehran. Using the convenience and purposive sampling methods, 144 people were selected from 5000 male veterans and were randomly assigned to the experimental (96 people) and control (48 people) groups. The experimental group was divided into eight groups of 12 people, and the control group was divided into four groups of 12. After the sample attrition, 116 male cases with war disabilities were assigned to the experimental group (76 people) and 40 people to the control group.
3.2. Inclusion Criteria
Subjects having the handicapped percentage of less than 50%, minimum educational level of primary school, age of 40 to 60 years, and mental disorders (diagnosed by expert psychologists and psychiatrists) were included in this research, while those with a history of addiction to drugs or receiving prescriptions for psychotic disorders were excluded.
3.3. Exclusion Criteria
Exclusion criteria also included: (1) dissatisfaction and unwillingness of the individuals to continue participating in the study; (2) use of any opiates; (3) psychotropic substances, or alcohol, and absence from treatment sessions for more than two sessions.
3.4. Intervention
After completing the testing schedule, 12 sessions of therapy, each taking two hours, were conducted in the mental health center for war-handicapped, Tehran, Iran. After 12 sessions of therapy, twice per week, 76 participants from the experimental group and 40 from the control group (76 + 40 = 116) successfully completed the therapy. The experimental group underwent group-based cognitive-behavioral therapy, whereas the control group received Jacobson's progressive muscle relaxation technique.
3.5. Data Collection
3.5.1. Anxiety Scale (State-Trait Anxiety Inventory-STAI)
This scale was developed in 1970 by Spielberger. The first form of this scale was introduced in 1970 and its revised form in 1983. The Trait-Mode Anxiety Scale has 40 self-report items, with the first 20 options measuring state anxiety and the second 20 options evaluating trait anxiety. This scale has high credibility and reliability. This scale is rated based on a 4-point Likert scale (very low, score 1 to very high, score 4). On this scale, for both trait and state, anxiety scores range between 20 and 80. Therefore, the score of each subject in each form ranges from 20 to 80 (18).
3.5.2. Beck Depression Inventory (BDI) Scale
This scale was developed in 1961 by Beck. The scale contains 21 items that measure the physical, behavioral and cognitive symptoms of depression. Each item has four options that are scored from 0 to 3 and determine different degrees of depression from mild to severe. The maximum score in this test is 63, and the minimum score is 0. A score of zero to nine indicates no depression. A score between 10 and 16 indicates mild depression, a score between 17 and 29 indicates moderate depression, and a score between 30 and 63 indicates major depression. Beck Depression Inventory second edition (BDI-II) is a revised form of the Beck Inventory designed to assess the severity of depression. The revised form of depression is more in line with the diagnostic and statistical guidelines for mental disorders than the first form. In addition, the second edition of this questionnaire covers all the elements of depression based on the cognitive theory of depression (19).
3.6. The Reliability and Validity of the Data Collection Instruments
Spielberger (20) tested the stability and validity of test-retested intervals STAI over periods of 30 to 60 days using male and female high school students as subjects. For the A-Trait test, the test-retest correlations displayed a range of 0.65 to 0.75 - 0.62. A similar test was administered among undergraduate students over test-retest intervals of 20 to 104 days. The A-Trait scale resulted in a test-retest correlation range of 0.73 to 0.86. The A-State scale then resulted in a test-retest correlation range of 0.27 to 0.54, which was expected. The A-State responses are thought to be based upon momentary circumstances during the time of the test, thus lowering its stability.
Beck Depression Inventory (BDI) Scale has an alpha coefficient of 0.80, and its construct validity has been established. It is able to differentiate depressed from non-depressed patients. Its internal consistency among the undergraduate students was high with Cronbach’s alpha = 0.93 (21). Cronbach’s alpha in this study was 0.87.
3.7. Statistical Analysis
To analyze the data, descriptive statistics (i.e., mean and standard deviation) and multivariate analysis of covariance were used in SPSS, version 26. The level of significance in the tests was set at 0.05.
4. Results
Paired t-test showed a significant difference between the mean of pre-test and post-test scores of dependent variables of psychological symptoms (depression-anxiety) of war veterans in the experimental groups 1 and 2 of the cognitive-behavioral program (Table 1).
| Variables | N | Pre-test | Post-test | T Value |
|---|---|---|---|---|
| Depression | ||||
| Experimental 1 | 40 | 48.02 ± 7.66 | 47.80 ± 7.37 | 0.68 (0.005) |
| Experimental 2 | 76 | 48.16 ± 7.03 | 38.64 ± 3.62 | 18.92 (0.001) |
| Anxiety | ||||
| Experimental 1 | 40 | 73.82 ± 7.93 | 73.50 ± 8.08 | 0.80 (0.005) |
| Experimental 2 | 76 | 68.74 ± 7.78 | 60.05 ± 8.43 | 11.30 (0.001) |
Kolmogorov-Smirnov test was used to check the normality of the distribution of scores in the study groups, and the results showed that the level of significance for both groups in both stages of the test and for the studied variables was more than 0.05. (P < 0.05); thus, the null hypothesis of the test is not rejected. Levene’s test was used to test the assumption of equality of variance. Considering that the F-statistic for the dependent variables of the study, that is, depression and anxiety, was greater than 0.05, the assumption of equality of variances between the two groups was accepted (Table 2).
| Variables | Source of Changes | df | Average Squares | F | P | Effect Size |
|---|---|---|---|---|---|---|
| State Anxiety | Group membership | 1 | 1969.83 | 66.42 | 0.000 | 0.376 |
| Depression | Group membership | 1 | 1826.27 | 143.17 | 0.000 | 0.566 |
Results of Multivariate Analysis of Covariance on the Effect of Group Cognitive-Behavioral Therapy on Dependent Variables in Research Groups
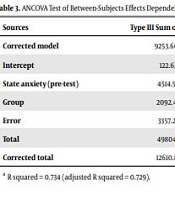
In examining the assumption of homogeneity of variance-covariance matrix, considering that the F-statistic was smaller than the corresponding value in Fisher's table and considering that the corresponding significance level was more than 0.05 (P > 0.05), the null hypothesis of the Box's M test (based on variance homogeneity) was accepted. Also, considering that in the relationship between auxiliary variables (co-scattering) and dependent variables (post-test) a significance level of less than 0.05 was obtained (P < 0.05), it can be stated that the assumption of linearity of the relationship between auxiliary variables (dependent) and dependent variables has been observed. The assumptions of alignment of variables and independence of errors also showed that the tolerance index for the predictor variable was less than 0.90. The variance inflation factor was also less than 10, and the value of the Watson camera-test, which was performed to test the hypothesis of error independence, ranged from 1.5 to 2.5. According to the above assumptions, multivariate analysis of covariance (MANCOVA) test was used. Also, the results of four multivariate analysis of covariance tests (Pilay effect, Wilkes lambda, holding effect, and largest Ray root) related to the difference of research variables were statistically significant. Therefore, the two groups were significantly different in at least one of the studied variables in the post-test stage (Tables 3 and 4).
| Sources | Type III Sum of Squares | df | Mean Square | F | Significancy | Partial Eta Squared |
|---|---|---|---|---|---|---|
| Corrected model | 9253.60 a | 2 | 4626.80 | 155.73 | 0.000 | 0.734 |
| Intercept | 122.63 | 1 | 122.63 | 4.13 | 0.045 | 0.035 |
| State anxiety (pre-test) | 4514.56 | 1 | 4514.56 | 151.95 | 0.000 | 0.574 |
| Group | 2092.45 | 1 | 2092.45 | 70.43 | 0.000 | 0.384 |
| Error | 3357.23 | 45 | 29.71 | |||
| Total | 498042 | 48 | ||||
| Corrected total | 12610.83 | 47 |
ANCOVA Test of Between-Subjects Effects Dependent Variable: State Anxiety (Post-test)
| Sources | Type III Sum of Squares | df | Mean Square | F | Significancy | Partial Eta Squared |
|---|---|---|---|---|---|---|
| Corrected model | 6196.84 a | 2 | 3098.42 | 248.38 | 0.000 | 0.815 |
| Intercept | 38.96 | 1 | 38.96 | 3.12 | 0.080 | 0.027 |
| Depression (pre-test) | 4000.21 | 1 | 4000.21 | 320.67 | 0.000 | 0.739 |
| Group | 2048.87 | 1 | 2248.88 | 180.28 | 0.000 | 0.615 |
| Error | 1409.60 | 113 | 12.47 | |||
| Total | 210303 | 116 | ||||
| Corrected total | 7606.44 | 115 |
ANCOVA Test of Between-Subjects Effects Dependent Variable: Depression (Post-test)
5. Discussion
The aim of this study was to determine the effectiveness of group cognitive-behavioral therapy on the anxiety and depression of war veterans. The results showed that group cognitive-behavioral therapy was effective in improving the psychological symptoms (reducing depression and anxiety) of war veterans. Consistent with this finding, the results of research by Recabarren et al. (15), Sakakibara et al. (22), and Lee et al. (23) showed that cognitive-behavioral therapy leads to improved general health and psychological symptoms (i.e., anxiety, stress, depression, and anger) of clients. Consistent with the findings of the present study, Lamb et al. (24) showed that the use of cognitive-behavioral therapy in a group manner reduced the symptoms of anxiety and anger in a group of chronic medical patients.
In line with the present finding, Lee et al. (23) showed that the use of cognitive-behavioral program in addition to improving lifestyle in patients with chronic pain reduced mood symptoms and stress. Explaining the findings of this study, it can be stated that psychological symptoms are important factors in the development of psychiatric illnesses and follow-up treatment. Psychological symptoms and the stresses caused by these symptoms peak during the illness period and make the problems caused by physical illnesses more pronounced among veterans. Theories in this field and the interventions based on them have always sought to develop and promote theoretical and practical models regarding how irrational thoughts are formed and methods to control them (15, 22, 23).
Documents of war veterans with depression are quite depressing; thus, the positive effect of cognitive-behavioral therapy on depression in war survivors with disabilities due to the use of cognitive methods, including the identification of negative thoughts, knowing the difference between logical and irrational self-talk, and doing exercises such as relaxation, objectivity, and behavioral muscle relaxation, can justify lowering depression scores in this group of clients. Consistent with the present finding on the effectiveness of cognitive-behavioral therapy in reducing depression and anxiety in war veterans, previous studies such as Lau et al. (25) and McGinn et al. (26) have shown that cognitive-behavioral therapy reduces mood problems and increases client resilience. In the same vein, it can be stated that this approach can help free people from unwanted thoughts and habits and unhealthy patterns of behavior. Hence, patients realize their abilities and increase their resilience by changing roles in life. By increasing cognitive-behavioral skills, individuals develop a stronger sense of control.