1. Background
The hepatitis A virus is among the most common causes of fecal-oral infection in the developing world. Hepatitis A is a single-stranded ribonucleic acid virus assigned to the genus picornavirus, and only one serotype is known with no cross-reactivity with other hepatitis viruses. Hepatitis A infection has a wide clinical spectrum, ranging from asymptomatic cases to severe acute liver failure that leads to mortality. It has an incubation period usually ranging from 14 to 28 days.
The onset of clinical features is abrupt and commonly comprises fever, diarrhea, nausea, abdominal discomfort, and elevated aminotransferases. The hepatitis A virus by far is the most common cause of acute hepatitis in the world, followed by the hepatitis E virus. Non-icteric hepatitis is common in children, with chronicity and associated complications occurring very rarely. Symptomatic hepatitis and death are more likely to occur with increasing the average age of infection (1, 2).
Prolonged epidemics are noted with hepatitis A due to person-to-person transmission, leading to significant economic consequences. Public health interventions are particularly gaining momentum in the western world, with the ongoing outbreak of hepatitis A reported in the United States as one of its largest-ever outbreaks of the disease. A public health emergency for hepatitis A was declared in Florida, the United States, in August, with over 2000 cases across several counties in the year 2019 (3). Among the worst affected states are Kentucky, Ohio, Minnesota, Colorado, the United States, and several more, and vaccination efforts have been initiated.
A rising number of hepatitis A naïve adults in the population leads to a paradoxical increase in hepatitis A morbidity and mortality. In addition, several hepatitis A epidemics in these age groups have been reported from numerous countries in Europe and Kerala coastal state and a few outbreaks from other areas of India (4-11). With this background in mind, the present study aimed to investigate and characterize an outbreak of acute viral hepatitis in an Indian Himalayan mountain camp in a tertiary-care teaching hospital in the Jammu region of Jammu and Kashmir State, India.
2. Methods
This investigation was carried out in a tertiary-care teaching hospital located in the middle of the mountains/hills in the Jammu region of Jammu and Kashmir, India, during June 1 to July 31, 2019. All the patients who visited the hospital with clinical features suggestive of viral hepatitis infection were included in this study. The study was conducted after obtaining Institutional Ethics Committee approval (CHNC-IEC 2/2019) affiliated to Command Hospital (Northern Command), Udhampur for identity anonymization for all the patients. The patient population consisted of travelers exploring the region.
The patients were admitted to the acute medical ward of the hospital, and patients’ particulars, including demographic information (e.g., age and gender), were recorded. Detailed clinical history and clinical examination findings were noted by a physician. Whole blood samples were collected on admission, and separated serum samples were immediately sent for blood biochemistry and serological tests for hepatitis A. The patients were symptomatically managed and followed up until discharge. The duration of hospitalization for each patient was recorded.
All the samples were analyzed for liver function tests, including serum bilirubin, alanine transaminase (ALT), and aspartate transaminase (AST), in addition to other routine biochemistry investigations. Anti-hepatitis A antibodies [e.g., immunoglobulin M (IgM)] were detected using a rapid solid-phase immunochromatographic assay and an IgM-capture enzyme-linked immunosorbent assay (ELISA). The case definition of hepatitis A infection in this investigation was a patient with clinical signs and symptoms compatible with hepatitis A, such as fever, malaise, upper abdominal pain, nausea, anorexia, icterus, hepatomegaly, and positivity for anti-hepatitis A IgM.
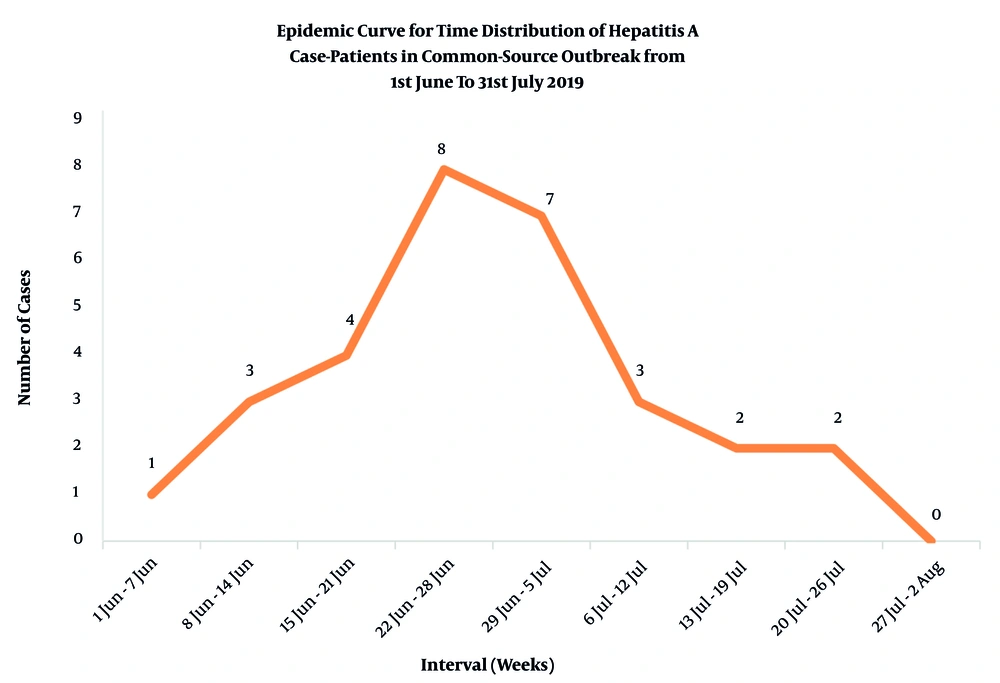
A line list of case-patients was prepared, and an epidemic curve was plotted. Water was not available for environmental surveillance as it was running water from various small mountain streams/rivers. Clinicodemographic, clinical, laboratory, and outbreak variables were descriptively analyzed using Microsoft Excel software (version 2016). Categorical variables are presented as percentages, and continuous variables are presented as mean ± 95% confidence interval (CI).
3. Results
A total of 30 patients were referred to the hospital with symptoms of acute viral hepatitis, and all 30/30 patients (100%) were confirmed the case-patients of hepatitis A infection by anti-hepatitis A IgM detection. The mean age of the subjects was 27.3 ± 2.7 years. A total of 24 case-patients (80%) among 30 patients (95% CI: 0.657 - 0.943) were within the age range of 20 - 30 years. Only two case-patients under the age of 20 years and four case-patients over the age of 30 years were present. A male preponderance was observed with 22 male patients (73.3%; 95% CI: 0.575 - 0.891) and 8 female patients (26.7%; 95% CI: 0.109 - 0.425).
A peak was observed from June 22 to July 5, 2019, with the maximum number (n = 15) of case-patients noticed in this duration as plotted in the epidemic curve (Figure 1). The clinical spectrum was heterogeneous, with no single sign or symptom common to all the patients. The most common clinical features among the case-patients were anorexia and vomiting (Table 1). No history of high-risk behavior was elicited from the case-patients.
| Clinical Features (n = 30) | Frequency (n) | Proportion (%) (95% CI) |
|---|---|---|
| Fever | 23 | 76.67 (0.615 - 0.918) |
| Malaise/fatigue | 19 | 63.33 (0.461 - 0.806) |
| Anorexia | 26 | 86.67 (0.745 - 0.988) |
| Nausea/vomiting | 24 | 80.00 (0.657 - 0.943) |
| Diarrhea | 6 | 20.00 (0.057 - 0.343) |
| Upper abdominal pain | 23 | 76.67 (0.615 - 0.918) |
| Hepatomegaly | 17 | 56.67 (0.389 - 0.744) |
Liver function tests showed mild derangement in all the case-patients. The mean values of AST, ALT, total bilirubin, and alkaline phosphatase were 82 ± 5.3 U/L, 110 ± 7.6 U/L, 4.3 ± 1.07 mg/dL, and 102 ± 3.3 IU/L, respectively. Mild jaundice accompanied by dark-colored urine was observed in all the patients. Anti-hepatitis A IgM was positive in all 30 case-patients. Atypical manifestations, such as arthralgia, myalgia, cough, constipation, lymphadenopathy, or pruritus, were not observed in any patient. All the patients required hospitalization, ranging from a minimum stay of 3 up to 26 days. The mean duration of hospital stay was 11.86 ± 2.53 days. All the patients fully recovered, and the case fatality rate in this investigation was 0%.
4. Discussion
India is an endemic region for hepatitis A infection, with well-documented epidemics and sporadic cases. The most common form of viral hepatitis is hepatitis A in the world. The geographical distribution of hepatitis A infection is heterogeneous and is closely linked with sanitary conditions and hygiene, and thereby with socioeconomic development (12-15). In highly endemic regions where infections are widespread, most individuals are infected in early childhood primarily resulting in asymptomatic infections and very few outbreaks. Although India was a high endemicity area for hepatitis A, declining early childhood exposure and seroprevalence, along with a rising number of reported outbreaks, is increasingly suggestive of a shift in epidemiology (6, 7, 9).
The current hospital-based investigation reported 30 case-patients of hepatitis A infection in 2 months, clearly suggestive of a common-source outbreak. The sample size was limited to a small population in a makeshift mountain camp. A greater number of infected but oligosymptomatic cases in the region may be anticipated, as only symptomatic patients seeking healthcare were included in this investigation. The age distribution of hepatitis A infection in the present study population was predominantly in the young adult/adult (range: 20 - 30 years) age group. This finding is in line with the findings of other outbreak investigations in the country, which further signifies that an increasing number of hepatitis A naïve individuals exist in this age group. Likewise, antibody levels of anti-hepatitis A among neonates in India are reported to be low at 50 - 60%, compared to nearly 100% since 15 years ago.
Increasing the age of first exposure increases the likelihood of icteric or symptomatic hepatitis, complications, and outbreaks. A male preponderance was also observed among the case-patients in the current setting, similar to findings reported by other studies. The causes may range from increased exposure to the male population to better health-seeking behavior (10, 16).
The number of case-patients peaked for 2 weeks during June 22 to July 5. The epidemic curve is suggestive of a common source outbreak, with a rapid rise in the first 3 weeks of June, followed by a peak for 2 weeks and a sharp fall from the second to fourth week of July. Case-patients continued to occur for several weeks starting since early June, indicating a constant source of infection. There were no peaks in the epidemic curve after the initial fall, suggesting that person-to-person transmission and repeated exposures were unlikely.
The fecal-oral transmission of hepatitis A is the most common route, and poor quality of drinking water is among the main culprits implicated in outbreaks. Poor sanitation and hand hygiene, improper food handling, contamination of food, and sewage contamination of water pipelines are also very common modalities of transmission frequently reported. Due to the hospital-based nature of the study, the exact source of infection could not be identified by means, such as water sample testing (17).
The present investigation was conducted in a hospital setting in an Indian Himalayan mountain camp, and unique public health challenges exist in these regions (18). The current de novo common-source outbreak of hepatitis A was likely due to contaminated water in the mountain country. Residents in this region often do not have access to an intermittent residential treated water supply. It is a common practice among mountain residents or travelers in this region to use untreated running water from streams and rivers for cooking, drinking, and washing purposes. Local knowledge of the potability of these water sources and practices, such as adequate water boiling before use, are well-established determinants for outbreak prevention and control.
The contamination of these water sources by excrements from human settlements, livestock, and mountain fauna is a cause for concern. Effluents from settlements located in the higher reaches of the mountains mainly contribute to downstream contamination. Climatological considerations are significant in hepatitis A outbreaks, with heavy rainfall typically associated with a peak in the number of reported cases. Likewise, the current study reported an outbreak in the peak monsoon months of June to July in this region. Open defecation by travelers, hikers, and mountaineers is a significant phenomenon in this region, directly leading to the contamination of the indigenous water sources soon after rainfall. Other human activities in mountain campsites, such as washing and cooking, also lead to water pollution. Mountain wilderness environments and campsites universally pose risks, regardless of developed or developing socioeconomic conditions, due to largely compromised hygiene in these areas.
The clinical features of the case-patients in the present outbreak were largely non-severe, with mild jaundice observed in all cases. Mild to moderate elevations in liver function parameters, along with commonly reported clinical features, such as fever, malaise, abdominal pain, nausea, diarrhea, and hepatomegaly, were observed. The symptomatology of hepatitis A infections varies significantly with the age of the infected individual. Asymptomatic presentation is noticed in almost half of all children under the age of 6 years, and the remaining have a subclinical disease not easily recognizable as hepatitis. Since 6 years of age to adulthood, more than 75% of individuals are observed to develop hepatitis characteristics, including jaundice and dark urine (19). The risk of fulminant hepatitis and mortality, although very low, increases with the age of the patient (20). No death occurred in the present investigation, although the patients required hospitalization for an average duration of 12 days.
Although most individuals in resource-poor countries are infected in early childhood, anti-hepatitis A seroprevalence rates in adults are falling in many parts of the world, with the increasing age of the first exposure (21, 22). Likewise, India is experiencing a considerable decrease in early childhood exposure (23). A mixture of high and low endemicities are noted across the country, owing to improving socioeconomic conditions. A transition in the epidemiology of this disease is noticeable in India, with children under 2 years of age no longer representative of the bulk of cases (24, 25).
Hepatitis A infection accounts for 0.5% of the mortality due to viral hepatitis, causing approximately 7,134 deaths in 2016 according to World Health Organization estimates. Lifelong protection from hepatitis A is conferred by seroconversion, either by childhood infection or vaccination. Anti-hepatitis A IgM and immunoglobulin G antibody titers are detectable in the blood of infected individuals by an ELISA. They are the mainstay for confirmatory diagnosis and assessment of immunization status, respectively. The IgM levels are generally rendered undetectable within 3 - 6 months. Viral particles can be detected by immune electron microscopy in the stool early in the disease, before the onset of jaundice, but disappear in up to 2 weeks after the onset of jaundice. Hepatitis A particles may also be detected in bile, blood, and the liver by nucleic acid hybridization assay or polymerase chain reaction. The investigations of seroprevalence, along with the exploration of national-level interventions for better sanitation and vaccination for high-risk groups, are assuming public health importance (26).
Large outbreaks of viral hepatitis are burdens on local public health systems. Water safety is a concern in developing economies worldwide assuming greater importance in mountainous settings where treated potable water is not readily available. It is difficult to control outbreaks in scenarios where the water supply remains unsafe persistently and infection rates are high. Water sustainability and the development of infrastructure and distribution networks are warranted for improved access to safe water for human consumption. Strengthening outbreak surveillance systems is crucial, as incidents often go unreported. Communities living further downhill are at risk of infection due to using the same contaminated sources of water, which augments the vicious cycle and leads to large epidemics which are detected very late. Medical personnel to diagnose, treat, and ascertain the risks in these settings are scarce. Therefore, small clusters of cases should be identified and notified, as these diseases can easily reach epidemic proportions.
The virus is also resistant to routine disinfection procedures and food safety measures used for controlling bacterial pathogens. In countries with decreased risk of infection from contaminated food or water, outbreaks are observed in people who inject drugs (PWIDs) or men who have sex with men. Other high-risk groups include transfusion recipients, travelers, healthcare professionals, immunocompromised individuals, sewage workers, prisoners, military personnel, and liver transplant recipients (3).
Hepatitis A is an entirely vaccine-preventable illness, and the vaccination of high-risk adults is the mainstay for outbreak control (27). At-risk groups in the American population also predominantly include PWIDs and homeless individuals, especially in the wake of the nationwide opioid crisis. Among other strategies, the United States Food and Drug Administration has recently begun testing frozen fruits and berries for contamination by hepatitis A and norovirus (28). The prevention of hepatitis A morbidity and mortality in the young adult population, due to the severity of illness in this age group as evidenced by the fatalities reported in these outbreaks, is the central theme for policymakers (29).
The hepatitis A vaccine is an inactivated killed vaccine and was first introduced in the United States in 1996. The number of annual cases subsequently reported in the US have dropped from 31,000 to less than 1,500 presently according to Centre for Disease Control and Prevenstion estimates. An ongoing outbreak of hepatitis A in the United States since 2016 has affected at least 29 states, and vaccination has been the leading public health intervention adopted across the country. With over 23,600 infected individuals, most of them requiring hospitalization, and over 230 deaths, the USA outbreak serves as a classic example of the deadly nature of hepatitis A infection in a largely seronegative population of adults in developed countries with good hygiene. Hepatitis A vaccination is presently not prescribed in the Indian National Immunization Schedule. The continued surveillance and assessment of seroprevalence will be crucial in devising vaccination strategies, and coordination with public sectors for safe water supply will also be valuable for public health (30).
4.1. Conclusions
A common-source outbreak of viral hepatitis A during June 1 and July 31, 2019, was investigated in a hospital setting in a mountain camp, with 30 confirmed case-patients and no mortality. Hepatitis A outbreaks can occur through the consumption of untreated mountain stream/river water due to upstream contamination with human/animal excrements. Strengthening surveillance systems, traveler education, vaccination, and intersectoral coordination for safe water supply remains a necessary public health measure.
4.2. Research Highlights
4.2.1. What Is Already Known?
Hepatitis A is an emerging public health problem worldwide, with alerts issued in developed countries, although it remains under-reported, under-diagnosed, and under-investigated in the developing world. A public health emergency for hepatitis A was declared in Florida in August, with over 2,000 cases across several regions of the United States in 2019.
4.2.2. What Does This Study Add?
Hepatitis A outbreaks can occur through the consumption of untreated mountain stream/river water due to upstream contamination with human/animal excrements. Strengthening surveillance systems, traveler education, vaccination, and intersectoral coordination for safe water supply remains a necessary public health measure.