1. Introduction
Penetrating abdominal injuries form an important component of surgical emergencies in peripheral hospitals. The victims are essentially healthy individuals and mostly belong to the young and middle age group. These injuries have a significant morbidity and mortality in view of the vascular and visceral injury associated with these injuries. The management of these injuries gives rise to specific challenge with respect to pre-hospital care, transport, resuscitation, and management strategies in a resource poor setting.
This study aimed to report the successful surgical management of abdominal injury with a construction iron rod, traversing from the left lower abdominal wall to the left posterior chest wall in a young male.
2. Case Presentation
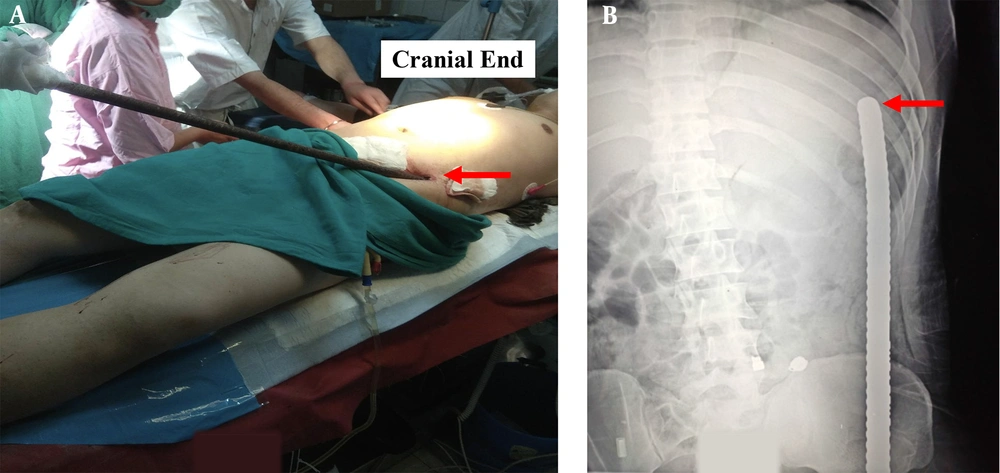
A 26-year-old male presented to a remote district hospital in northeast India during the early hours of the day with an alleged history of penetrating injury to the abdomen and chest wall following the fall over an under construction iron rod from a height of about 3 metres. On arrival at the hospital, the individual was alert, coherent, and hemodynamically stable, with the chief complaints of abdominal pain. There was no episode of hematemesis or proctorrhagia, or haematuria with his general survey within normal limits. Abdominal examination revealed trans-abdominal penetrating injury with a ribbed iron rod measuring ~ 1 meter in length and 16 mm in calibre impaled in situ. The entry wound in the left groin, 7 cm from ASIS, with the other end palpable along posterior-lateral chest wall ~ 10 cm from the left posterior axillary line at the level of 9th rib (Figure 1A). Sero-sanguinous discharge was present at the entry wound. Generalized abdominal tenderness with rebound tenderness was present. Bowel sounds were present. Danforth sign was negative. Digital rectal examination finding was normal. Examination of the chest wall showed tenderness at the site of injury. Bilateral breath sounds were equal, and no adventitious sounds were present.
Initial laboratory examination investigations demonstrated Hb- 12.3 gm% and leucocytosis [TLC-15,300 /mm3, DLC- P87 L10]. Coagulation studies, liver function tests, and renal function tests were normal. There was no radiological evidence of pneumothorax or haemothorax. X ray of the abdomen showed no evidence of pneumoperitoneum. The iron rod was appreciated entering from the left lower abdomen and the tip of the rod was at the level of the 9th rib posteriorly (Figure 1B).
Following general survey, pre-operative broad spectrum antibiotics and tetanus toxoid prophylaxis were administered. Foleys catheter was placed, which drained clear urine.
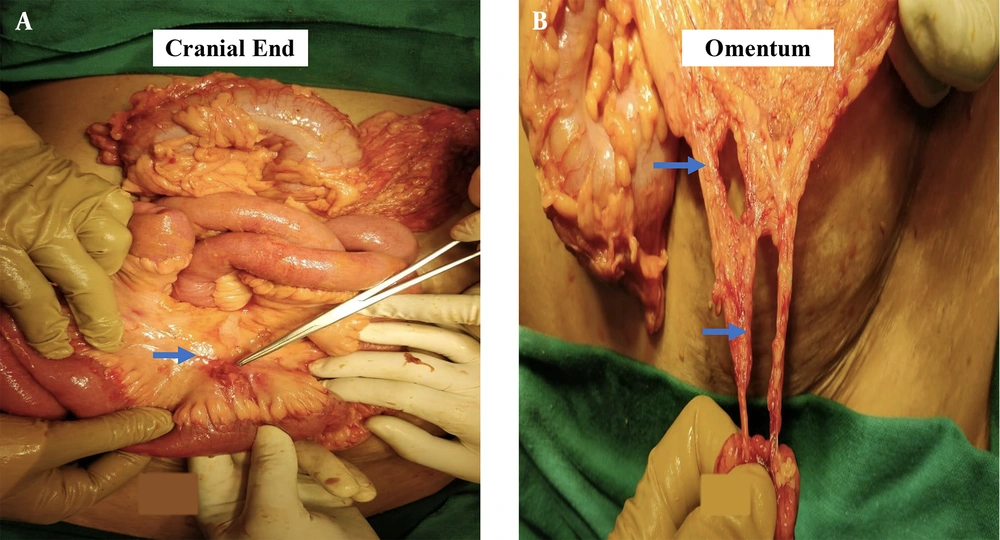
Formal exploration of abdomen for operative management of intra-abdominal and possible diaphragmatic injuries was planned due to non-availability of any other imaging modality other than X ray to assess trajectory of the foreign body and the extent and the character of the intra-abdominal injury. The patient was induced with 120 mg Propofol, intubated, and maintained with Atracurium (bolus 30 μgm bolus and 10 μgm every half hour) and paracetamol infusion. The patient was on low flow anaesthesia (1 Litre/min) with low tidal volume (4 mL/kg) to reduce the diaphragmatic movement. On exploration via standard midline laparotomy, the iron rod was intra-peritoneal, entering the peritoneal cavity from the left iliac region, traversing the abdominal cavity for around 15 cm before penetrating the parietal peritoneum entering the posterolateral intramuscular plane. Around 10 cm of ileal loop was entangled on the iron rod, and there was soiling of the general peritoneal cavity with multiple tears in the mesentery and the omentum (Figure 2A and B). There was no other visceral or vascular injury. The rod was removed after assessing the extent of the injury and margins of the breached peritoneum freshened up, thorough peritoneal lavage was given. The omental tears and mesenteric tears were repaired, and the abdomen was closed. The entry and possible exit tracts were explored via two separate incisions along anterior abdominal wall, and posterolateral aspect of the chest and unviable margins of the tract along the rod was excised. The post-operative recovery of the patient was uneventful, and he was discharged on 10th post-operative day.
3. Discussion
Impalement abdominal injuries are acute emergencies. The management of these injuries are based on the basic principles of trauma care. The patient should be managed as per the initial assessment of the hemodynamic status and the amount of blood loss, and in the meantime, preparation for the surgery should be made (1). The highly infective potential of the impaling objects merits the administration of the broad spectrum antibiotics and the tetanus prophylaxis. The tract of the impaling object determines the operative approach (1-3).
Diagnostic laparoscopy plays an important role in the impalement abdominal injuries. It plays a diagnostic role in assessing any solid organ injury, diaphragmatic injury as well as any vascular injury. Laparoscopy has an advantage that it can have a therapeutic role too. The various indications for laparoscopy include thoracoabdominal stab wounds, anterior or flank stab wounds without obvious indication for laparotomy, and abdominal stab wounds with omental herniation in a hemodynamically stable patient because most of these conditions carry a high risk for diaphragm injury, and laparoscopy is ideal for their repair (4-7).
The impalement injuries of the abdomen have the component of both the penetrating injury as well as blunt injury and commonly have multiple organ injuries. These injuries carry high morbidity and mortality due to multi system involvement. Impalement injuries are classified into three types based on the mechanism of injury (8-10). Type I impalement injury results from the impact of the body against an immobile object (8, 11, 12). Type II impalement injuries are due to the impact of a mobile object into the stationary patient (8, 13, 14). Type III impalement injury combines the mechanism of injury in type I and II, and results are due to an impact between a mobile patient and a mobile object (8, 9).
The management of impalement injuries can be handled by following few broad recommendations. The treatment generally demands multidisciplinary team approach due to multiple organ system involvement. The immediate management of the penetrating abdominal injuries includes the initiation of resuscitation and the rapid assessment for the source of bleeding. The patients in shock should be administered crystalloid solutions and blood products. The impaled foreign object should not be removed or manipulated outside the operation theatre; however, the object can be shortened for safe transport of the patient to the medical facility. The removal of the object can cause the release of the tamponade effect exerted by it, leading to extensive bleeding (8, 15). The trajectory of the object should be considered while planning the treatment as it helps in making an assessment of the damage to vital structures in its path. Hemodynamic stability at the time of presentation in the hospital can be misleading as it doesn’t preclude vascular injury (8, 16, 17). Similarly, hematochezia and haematuria may be absent in the penetrating abdominal injuries with gastrointestinal and genitourinary injuries (8, 18). The spine should be immobilized in patients whose spinal injury is anticipated depending on the mechanism of injury. Abdominal contrast enhanced computerised tomography (CT) is the primary method for imaging of a stable patient. CT plays a phenomenon role in the evaluation of the injuries of the peritoneum, solid organs, as well as retroperitoneum; however, it rarely detects diaphragmatic and hollow viscus injuries (19, 20). The investigations carried out are based on the clinical evaluation as well as the hemodynamic stability of the patient at presentation to the hospital. A hemodynamically unstable patient should be directly taken to the operating room without the imaging studies (8, 21).
During the surgical exploration, incision should be placed in such a manner that it provides adequate exposure for vascular control as well as the it provides the visualisation of the tract of the penetrating object. Sometimes an unconventional or non-standard incision may be preferred since these incisions may facilitate the removal of the object under direct vision (8, 15, 21). The extreme force causing these impalement injuries may demand evaluation for damage to the structures in the vicinity of the tract taken by the foreign objects (8, 10). Complete exploration of the tract should be done, and adequate vascular control should be achieved prior to the removal of the impaled object (8, 15). Thorough debridement with lavage of the wounds as well as the structures along the trajectory of the impaling object should be carried out. Injuries to specific organs is managed as per the recommended guidelines of trauma. Wound closure is done as per the contamination status of the wound (8, 15).
Post operatively, the patients surviving these injuries may suffer from post-traumatic stress related disorders requiring psychological counseling (8, 22).
3.1. Conclusions
Penetrating abdominal injuries are acute surgical emergencies, and timely intervention can reduce the mortality hence improving the patient outcome. Prehospital care plays a critical role in the survival of these patients. The management of these injuries is in accordance with the basic trauma care principles. The investigations carried out in the management of these injuries is dictated by the clinical findings and the hemodynamic stability of the patient, and are limited to those that are mandatory for planning the surgical management. These injuries call for immediate resuscitation, quick transfer of patient to a tertiary care center where a speedy diagnosis is made and multimodality surgical intervention is available to improve the patient outcome.