1. Background
Intensive Care Unit (ICU) and Emergency Department (ED) nurses experienced unprecedented moral distress (MD) during the COVID-19 pandemic (1, 2). In these situations, nurses faced challenges such as a lack of safety protocols, inadequate personal protective equipment, shortages of ventilators, a sense of responsibility amidst uncontrolled spread and infection, limited or absent patient family visits, physical and psychological exhaustion, and fear of infecting themselves and their families while caring for critically ill and emergency patients (3-5). Under these circumstances, MD can affect nurses’ personal and professional lives (6). The experience of MD is associated with consequences such as lack of sleep, loss of appetite, feelings of worthlessness, nightmares, palpitations, changes in physical function, and headaches (7-9). Following the experience of MD, nurses may reduce the quality of their care or even avoid caring for patients in severe cases (10, 11). As a result, MD may lower job performance, job satisfaction, and resilience, potentially leading to burnout and leaving the profession (9, 12).
Research has shown that, during the COVID-19 pandemic, spiritual and moral factors are associated with job adjustment and mental health (13, 14). In stressful situations, spirituality can be a source of comfort, support, and meaning, helping to reduce anxiety and promote mental health (15, 16). Employees with higher moral intelligence (MQ) can distinguish right from wrong (17). Consequently, MQ and spirituality can be related to professional performance, resilience, and anger management (15, 18, 19). The results of a study indicated that participants’ MD had a significant positive relationship with spiritual intelligence (20). However, another study showed that spiritual well-being was not associated with MD (21).
Most Iranian nurses are Muslim, have strong spiritual beliefs, and consider serving during the COVID-19 pandemic as an act of worship. Besides issues such as the lack of resources (e.g., medicine and hospital equipment) and the shortage of nursing staff in ICUs and EDs, specific personal characteristics are also among the main issues in service provision. The discrepancy in some evidence regarding the relationship between MD and spirituality highlights a knowledge gap in this area.
2. Objectives
The present study was conducted to determine the relationship between MD, SWB, and MQ among ICU and ED nurses during the COVID-19 pandemic.
3. Methods
3.1. Study Design, Setting, and Sampling
This descriptive cross-sectional study was conducted on all nurses working in the ICUs, Coronary Care Units (CCUs), Neonatal Intensive Care Units (NICUs), and EDs of Ayatollah Mousavi, Vali Asr, Shahid Beheshti, and Al-Ghadir hospitals, which are affiliated with Zanjan University of Medical Sciences in Iran. Sampling was performed from May 31, 2020, to September 17, 2020, which coincided with the second peak of COVID-19 in Iran. During this period, the entire country experienced intermittent quarantines, and there were significant concerns and fears about the disease within both the community and the health system (22).
During the sampling period, Vali Asr Hospital was designated specifically as a care center for COVID-19 patients. However, due to the increasing number of COVID-19 cases, all hospitals, particularly the EDs and ICUs, were required to admit COVID-19 patients. Consequently, sampling in this study was conducted using the census method, which included all 543 nurses working in the ICUs and EDs of the hospitals under study. The inclusion criteria were having at least one year of work experience and a willingness to participate in the study. Of the 543 nurses, 487 were found eligible for the study.
3.2. Measures
Data were collected using four questionnaires: The personal and professional profile questionnaire, the Moral Distress Scale, the Ellison and Paloutzian Spiritual Health Questionnaire, and the Lennick & Kiel Moral Intelligence Questionnaire.
Demographic Information Questionnaire: This questionnaire included items related to personal and professional details, such as gender, age, marital status, education, hospital, unit, employment status, and work experience.
3.3. Moral Distress Scale
In this study, the Persian version of the Corley MD scale was used to assess the severity of MD (23, 24). Vaziri et al. developed the MD scale using a qualitative-quantitative method. These researchers examined the psychometric characteristics of the questionnaire on 300 Iranian nurses and confirmed its validity and reliability. The MD scale is a 30-item instrument that evaluates MD using a Likert scoring system, with responses ranging from 1 (almost never) to 7 (very much). A score of 1 to 3.5 indicates low MD, while a score above 3.6 indicates high MD. In the present study, the reliability of this scale was calculated to be 97% using Cronbach’s alpha (23).
3.4. Spiritual Well-being Scale
The collected data were analyzed using a 20-item scale developed by Ellison and Paloutzian. This questionnaire contains 10 questions that measure "religious well-being" and another 10 questions that measure "existential well-being." Additionally, a 10-item scale developed by Elliott was used to evaluate spiritual well-being (SWB) using a Likert scale. The responses on this scale range from 1 (I completely disagree) to 6 (I completely agree), with 9 items scored in reverse. The final score of this tool is obtained by adding the scores for each item. The total score for SWB is divided into three levels: Low (20 - 40), medium (41 - 99), and high (100 - 120). Notably, the psychometric properties of this scale were confirmed in a study involving 300 patients with myocardial infarction in the Iranian community (25). In the present study, the reliability of the questionnaire, as measured by Cronbach’s alpha, was 0.84.
3.5. Lennick and Kiel Moral Intelligence Scale
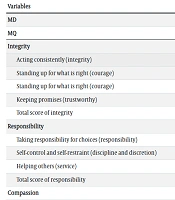
This scale, developed by Lennick and Kiel, includes 40 items across 4 dimensions (26). The psychometric properties of this scale were confirmed in Iran by evaluating 400 nurses (27). The four subscales of the integrity dimension are acting consistently (integrity), telling the truth (honesty), standing up for what is right (courage), and keeping promises (trustworthy). The responsibility dimension includes three subscales: Taking responsibility for choices (responsibility), self-control and self-restraint (discipline and discretion), and helping others (service). Kindness and friendliness are two subscales of actively caring about others. The forgiveness dimension also includes two subscales: Recognizing others’ feelings (courtesy, humility, civility) and recognizing spiritual needs (faith and reverence). This scale evaluates MQ using Likert-scale responses ranging from 1 (I completely disagree) to 5 (I completely agree). The scores for each item are summed to calculate the total score of the scale. The total MQ score is then divided into 4 levels: Low (40 - 50), moderate (51 - 100), high (101 - 150), and very high (151 - 200) (27). In the present study, the reliability of the questionnaire was calculated to be 0.91 using Cronbach’s alpha.
3.6. Procedures
After obtaining the ethics committee's approval, data collection was carried out with the official permission of hospital managers and head nurses. The researcher (i.e., the third author) visited the ICUs and EDs of the mentioned hospitals during different work shifts to meet with eligible nurses. After introducing herself, the researcher explained the study's objectives to the nurses and provided instructions on how to complete the questionnaire. Participants were asked to answer the questions carefully and honestly. To control for confounding factors such as environmental noise and the nurses’ workload while completing the questionnaires, the researcher collected the completed questionnaires one week after distribution.
3.7. Ethical Considerations
This study was approved by Iran’s National Committee for Ethics in Biomedical Research (IR.ZUMS.REC.1395.02). Written informed consent was obtained from all participants, and participation in the study was voluntary. Additionally, participants were assured of the anonymity of the questionnaires and the confidentiality of the data.
3.8. Statistical Analysis
Data obtained from the questionnaires were analyzed using SPSS software version 16 (SPSS Inc., Chicago, IL, USA). The normal distribution of the data was assessed using the Kolmogorov-Smirnov test. Both descriptive and inferential statistics were employed for data analysis. The mean was used to handle missing data, and outliers were detected by assessing the variance of the data. Independent t-tests and analysis of variance (ANOVA) were used to examine differences in the mean MD of nurses based on personal and professional variables. Additionally, the Pearson correlation coefficient was used to investigate the relationship between nurses’ MD and their SWB and MQ. The partial correlation coefficient was used to analyze the relationship between the total MD, SWB, and MQ scores of nurses. Multiple linear regression was employed to evaluate the predictability of the nurses’ MD variable using SWB, MQ, and personal and professional variables. The statistical significance level was set at P < 0.05.
4. Results
Of the 478 ICU and ED nurses, 374 completed the questionnaires and were included in the analysis, resulting in a response rate of 78.24%. The data from 4 questionnaires were excluded from the analysis due to the selection of only one option for all questions or the omission of answers to more than 50% of the questions. Ultimately, the data from 370 questionnaires were analyzed. The mean age of the nurses was 31.39 ± 6.04 years, and their mean work experience was 8.08 ± 6.19 years. Most participants were female (82.1%), married (60.3%), and worked in the EDs (51.8%) (Table 1).
| Variables | No. (%) |
|---|---|
| Gender | |
| Female | 312 (82.1) |
| Male | 68 (17.9) |
| Age (y) | |
| 22 - 30 | 197 (51.8) |
| 31 - 40 | 139 (36.6) |
| 41 - 50 | 34 (8.9) |
| Marital status | |
| Single | 138 (36.3) |
| Married | 229 (60.3) |
| Educational level | |
| Associate’s degree | 7 (1.8) |
| Bachelor’s degree | 364 (95.8) |
| Master’s degree | 9 (2.4) |
| Wards | |
| Intensive care unit | 127 (33.4) |
| Coronary care unit | 36 (9.5) |
| Neonatal intensive care unit | 197 (51.8) |
| Emergency department | 20 (5.3) |
| Employment status | |
| Casual employees | 191 (51.3) |
| Fixed employment contracts | 81 (21.3) |
| Permanent full-time employment | 108 (28.4) |
| Work experiences (y) | |
| 1 - 5 | 168 (44.2) |
| 6 - 10 | 93 (24.5) |
| 11 - 15 | 56 (14.7) |
| 16 - 20 | 51 (13.4) |
| 21 - 26 | 11 (2.9) |
The results indicated that participants experienced high levels of MD (Table 2), with 90.8% (n = 345) experiencing high distress and 9.2% (n = 35) experiencing low distress. The participants’ SWB was moderate, with the religious well-being score being higher than the existential well-being score (Table 2). The results showed that 0.3% (n = 1) of participants had low SWB, 71.3% (n = 271) had moderate SWB, and 28.4% (n = 108) had high SWB. Nurses’ MQ scores were moderate (Table 2), with 0.8% (n = 3) having moderate MQ, 31.3% (n = 119) having high MQ, and 67.9% (n = 258) having very high MQ.
| Variables | Mean ± SD |
|---|---|
| MD | 5.39 ± 1.05 |
| MQ | |
| Integrity | |
| Acting consistently (integrity) | 15.26 ± 2.28 |
| Standing up for what is right (courage) | 15.95 ± 2.09 |
| Standing up for what is right (courage) | 15.81 ± 2.06 |
| Keeping promises (trustworthy) | 15.48 ± 2.12 |
| Total score of integrity | 62.50 ± 7.20 |
| Responsibility | |
| Taking responsibility for choices (responsibility) | 15.77 ± 2.04 |
| Self-control and self-restraint (discipline and discretion) | 15.80 ± 2.08 |
| Helping others (service) | 15.79 ± 2.08 |
| Total score of responsibility | 47.36 ± 5.25 |
| Compassion | |
| Actively caring about others (kindness and friendliness) | 16.25 ± 2.15 |
| Forgiveness | |
| Forgive your mistakes | 15.55 ± 2.15 |
| Forgive the mistakes of others | 15.83 ± 2.08 |
| Total score of forgiveness | 31.37 ± 3.74 |
| Total score of MQ | 78.74 ± 8.77 |
| SWB | |
| Religious well-being | 48.86 ± 7.80 |
| Existential well-being | 42.78 ± 6.10 |
| Total score of SWB | 91.64 ± 12.88 |
Abbreviations: MD, moral distress; MQ, moral intelligence; SWB, spiritual well-being; SD, standard deviation.
Independent t-tests and ANOVA tests were performed to compare the mean MD of nurses based on gender (P = 0.581, t = -0.24), marital status (P = 0.201, t = -0.72), age (P = 0.301, F = 1.205, df = 2), and work experience (P = 0.123, F = 1.83, df = 4). However, these results did not show any statistically significant differences.
The ANOVA results indicated that the mean MD of nurses differed significantly based on the level of education (P = 0.019, F = 4.019, df = 2). Furthermore, the LSD post-hoc test results revealed that nurses with an associate’s degree experienced more MD than those with a bachelor’s degree (P = 0.036) and a master’s degree (P = 0.005). The mean MD of nurses also showed a statistically significant difference based on hospital wards (P = 0.01, F = 3.8, df = 3). The LSD post-hoc test results showed that nurses in the EDs experienced more MD than those in the ICUs (P = 0.004) and NICUs (P = 0.025). Nurses’ MD also showed statistically significant differences based on the hospital (P = 0.001, F = 9.95, df = 3). The LSD post-hoc test results indicated that nurses in Vali Asr Hospital, the designated care center for COVID-19 patients, experienced more MD than those in Ayatollah Mousavi Hospital (P = 0.001), Al-Ghadir Hospital (P = 0.001), and Beheshti Hospital (P = 0.003).
Nurses’ religious well-being showed a statistically significant negative relationship with their MD, whereas existential well-being did not. None of the dimensions of nurses’ MQ showed a statistically significant relationship with their MD. However, all dimensions of nurses’ MQ had a positive statistically significant relationship with both dimensions of existential well-being and religious well-being. The highest correlation was observed between the dimension of religious well-being and the dimensions of integrity and compassion (r = 0.34) (Table 3). The results of the partial correlation showed no statistically significant relationship between nurses’ MD and the total MQ or SWB scores. However, the total SWB and MQ scores had a positive statistically significant relationship (r = 0.33) (Table 4).
| Variables | Pearson Correlation Coefficient | ||||||
|---|---|---|---|---|---|---|---|
| MD | SWB | MQ | |||||
| Existential Well-being | Religious Well-being | Integrity | Responsibility | Compassion | Forgiveness | ||
| r | r | r | r | r | r | r | |
| MD | 1 | ||||||
| SWB | |||||||
| Existential well-being | -0.03 | 1 | |||||
| Religious well-being | -0.12 a | 0.71 b | 1 | ||||
| MQ | |||||||
| Integrity | -0.03 | 0.29 b | 0.34 b | 1 | |||
| Responsibility | -0.02 | 0.26 b | 0.29 b | 0.95 b | 1 | ||
| Compassion | 0.05 | 0.24 b | 0.34 b | 0.81 b | 0.77 b | 1 | |
| Forgiveness | 0.01 | 0.25 b | 0.26 b | 0.90 b | 0.92 b | 0.70 | 1 |
Abbreviations: MD, moral distress; MQ, moral intelligence; SWB, spiritual well-being.
a P < 0.05.
b P < 0.001.
| Controlled Variables | Partial Correlation | ||
|---|---|---|---|
| r | P-Value | df | |
| MQ | -0.10 | 0.061 | 377 |
| MD | |||
| SWB | |||
| SWB | 0.04 | 0.393 | 377 |
| MD | |||
| MQ | |||
| MD | 0.30 | 0.001 | 377 |
| SWB | |||
| MQ | |||
Abbreviations: MD, moral distress; MQ, moral intelligence; SWB, spiritual well-being.
A stepwise multiple regression model was used to determine the predictors of nurses’ MD. In this model, nurses’ MD was used as the dependent variable, while personal and professional variables (age, gender, marital status, education, employment status, hospital, and wards), dimensions of MQ, total MQ score, religious well-being, existential well-being, and total SWB score were considered as independent variables. After implementing the model, three variables—hospital, education, and compassion—remained in the model, while the rest were excluded. The model’s coefficient of determination (R²) in the third step was 0.09, and the adjusted coefficient (Adjusted R²) was 0.08. The results indicated that these three variables could only predict 8% of the changes in nurses’ MD (P = 0.003) (Table 5).
| Model | Unstandardized Coefficients | Standardized Coefficients | t | P-Value | 95.0% Confidence Interval for B | ||
|---|---|---|---|---|---|---|---|
| B | Std. Error | Beta | Upper Bound | Lower Bound | |||
| Constant | 162.15 | 15.57 | 10.41 | 0.001 | 131.54 | 192.77 | |
| Hospital | 8.56 | 1.74 | 0.25 | 4.92 | 0.001 | 5.14 | 11.98 |
| Education | -15.69 | 4.96 | -0.16 | -3.17 | 0.002 | -25.44 | -5.94 |
| Compassion | 1.49 | 0.74 | 0.10 | 2.02 | 0.044 | 0.04 | 2.95 |
5. Discussion
The stressful environment of ICUs and EDs, especially during the COVID-19 pandemic, caused nurses to experience high levels of MD (28, 29). The present study showed that 90.2% of nurses working in ICUs and EDs experienced high MD. Similarly, Babamohamadi et al. reported an MD severity of 86% among ED nurses in Semnan city, Iran (29). In Canada, the severity of MD among nurses was 58% (30), while it was 72% in Australia (31). These differences in results can be attributed to variations in the study environment, research timing, measurement scales, and the ethical climate of the research settings.
In the present study, personal characteristics such as gender, age, marital status, and work experience, with the exception of education, were not associated with nurses' MD. Previous studies have reported contradictory results regarding the relationship between certain personal and professional factors and nurses' MD (29, 32-34), which can be attributed to the different cultural contexts of these studies. However, the mean score of nurses' MD varied according to the hospital and wards, with ED nurses experiencing higher MD than ICU and NICU nurses. During the COVID-19 peak, the number of patients and the workload in EDs were higher than in other wards, contributing to higher MD levels among ED nurses. Among the studied hospitals, nurses working at Vali Asr Hospital, the designated care center for COVID-19 patients, experienced more MD than those in other hospitals. Factors related to MD in such situations should be sought in the nurses' work environment (35, 36).
Iranian nurses faced a shortage of resources to protect themselves and provide better care for patients during the COVID-19 pandemic, a problem that was common in many countries, where nurses faced shortages of resources and staff (37, 38). Sanctions imposed on Iran caused shortages of medicine and ventilators, placing additional pressure on the nurses. Due to the religious orientations of Iranian nurses, it is believed that MQ and SWB could enhance their resilience to MD.
The results of the present study showed that nurses' MD had no statistically significant relationship with their MQ and SWB, except for a negative statistically significant relationship between the dimensions of SWB and MD (r = -0.12). In line with our findings, Soleimani et al. found that participants' SWB was not associated with their MD (21). However, Hannani et al. reported a significant positive relationship between participants' MD and their spiritual intelligence (20).
Although nurses' religious well-being was associated with their MD in the present study, the correlation was not strong. A positive and statistically significant relationship was observed between participants' SWB and MQ (r = 0.30). Previous studies have also shown a positive relationship between participants' SWB and MQ (39, 40).
In critical situations such as the COVID-19 pandemic, where ICU and ED nurses were experiencing MD and moral injury (41), workplace support can play a crucial role in moderating the severity of nurses' MD. Iranian nurses served their communities with all the available resources and by relying on their faith, without any special material benefits. However, the lack of support for nurses, especially in high-stress areas like ICUs and EDs where long-term MD is experienced, can lead to job burnout and dissatisfaction (42, 43).
5.1. Conclusions
Due to the high MD experienced by nurses in ICUs and EDs, appropriate support for these nurses is essential. The high workload and lack of resources, particularly during the COVID-19 pandemic, increased the MD experienced by ICU and ED nurses. Although MD was not significantly related to the underlying characteristics, MQ, and SWB of the nurses, the characteristics of the work environment, such as the ward and the hospital, influenced the severity of MD. Based on these results, it is recommended that health system managers provide adequate facilities, equipment, and mental health support to nurses to reduce the severity of their MD.
In this respect, the long-term effects of MD on nurses can impact their physical and mental health and the quality of nursing services they provide. Therefore, further studies to explore the factors related to nurses’ MD in Iranian society are also recommended.
A strength of this study was its focus on MD, MQ, and SWB in both ICUs and EDs, allowing for a comparison of the two environments with the highest exposure to COVID-19 during the pandemic. However, the study has some limitations, including the high workload of chief nurses at the time of data collection, which may have affected their accuracy in completing the questionnaires. To address this, nurses were given one week to complete the questionnaires. The results of this study are influenced by the cultural context of Iran and the moral climate prevailing in the hospitals of Zanjan Province, which limits the generalizability of the findings.