1. Background
Today, information technology has permeated all fields, transforming numerous aspects of society. In medicine, the integration of this technology has become essential. This system leverages databases, connects medical centers and teams, and facilitates the transmission of diagnostic information. Telemedicine, in particular, involves using electronic communications and telecommunication technology to provide and support services such as remote clinical care, health education for professionals and patients, public health initiatives, and health management. It bridges the geographical and temporal gaps between service providers and recipients, enabling more efficient and accessible healthcare delivery (1).
Information and communication are critical tools for any entrepreneurial activity. Effective communication adds value, depending on the type and extent of the connection. A person with diverse and stronger connections can achieve results more quickly. Entrepreneurship involves identifying a social need and understanding the solutions provided elsewhere. Without information, identifying needs and providing solutions is impossible, making information and knowledge crucial for any entrepreneurial activity (1).
With the advent of the digital age and advances in telecommunication technology, interest in researching remote care services has increased (2). One of the most significant applications of information and telecommunication technology today is in healthcare (3). The development of information technology has created a vast global internet network. In developed countries, the internet is a vital tool for entrepreneurs, enhancing their capabilities and benefits. Information and communication have opened new horizons in entrepreneurship, business, and productive employment, playing an essential role in sustainable development within the global village. The digitalization of trade, marketing, education, information dissemination, communication, and transportation marks the transition from traditional practices to digital modernity. Information technology stands out as a potent industry for job creation (4).
Telemedicine represents a new field that uses this technology to exchange medical information (4). Recent technological advancements have expanded its role in medicine, making telemedicine increasingly vital for both doctors and patients. The goal is to eliminate unnecessary travel for patients seeking specialized medical expertise. The foundations of telemedicine include text, audio, and video communication between doctor and patient, as well as the exchange, storage, and processing of medical information (5). Unfortunately, despite its importance in medicine, telemedicine has not yet established its place in Iran. Researchers have questioned why telemedicine is not common in Iranian medical centers and why doctors do not utilize it as a treatment method. Identifying obstacles to telemedicine implementation is crucial, given its potential to accelerate remote medical services and significantly reduce service delivery times.
As information technology continues to develop in medicine, a significant transformation in healthcare service delivery can be expected. One of the primary applications of information technology is in healthcare (6). Additionally, telemedicine is a field where medicine has grown considerably and is significantly influenced by this technology (7). Telemedicine uses information and telecommunication technology to provide health services when there is a geographical or temporal distance between the service provider and recipient (8). Telemedicine supports services such as remote clinical care, health education for professionals and patients, public health initiatives, and health management (9).
The future of telemedicine and related teleconsultation has been discussed among health specialists for years, focusing on its potential to increase access to specialists for remote populations, reduce patient wait times, and improve referral systems and communication among primary, secondary, and tertiary service providers. The telemedicine network effectively covers large geographical distances, improving service delivery in both urban and rural hospitals. Teleconsultation has the potential to reduce the need for patients to travel for high-level services (10). The health system can leverage telemedicine and teleconsultation to benefit from specialists' knowledge and services in remote areas, reducing the need to establish new treatment centers and saving financial and human resources (11).
Numerous studies have addressed this topic both domestically and internationally. Mafi-Moradi et al. identified significant challenges in implementing telemedicine related to communication and information infrastructure, e-commerce, security, healthcare standards, regulations, and education. Despite these challenges, there are notable opportunities, particularly regarding the widespread adoption of communication technology, access to up-to-date information, and the elimination of technological gaps due to globalization, which can help overcome these obstacles (12). Barriers include the lack of clinical protocols, undefined telemedicine payment methods, and the absence of necessary certificates and regulations (13).
2. Objectives
This study aimed to design an entrepreneurial model using modern communication technologies in the health sector.
3. Methods
In this qualitative study, initial article searches were conducted using databases such as PubMed, Web of Science, and Scopus, with no time limitations until 2022. The search strategy combined MeSH terms and keywords related to telemedicine, new communication technologies, clinical medicine, and entrepreneurship, using AND and OR operators. Additional studies were identified by manually reviewing the references of relevant articles.
Inclusion criteria for articles were English and Persian publications focusing on the role of telecommunication technologies in clinical medicine. Articles without full-text availability were excluded. Two researchers independently reviewed the titles and abstracts of identified articles based on the inclusion and exclusion criteria, resolving disagreements through discussion or consultation with a third researcher. Data from the included articles were extracted using a standardized form. Content analysis was conducted to identify main themes and features of new communication technologies, which informed the development of a semi-structured interview guide comprising 10 questions.
The research community consisted of managerial faculty members from Iran University of Medical Sciences. The sample included faculty members selected through purposive sampling, followed by snowball sampling to include additional informed individuals. Individual interviews were conducted with willing faculty members and experts until data saturation was achieved. Interviews were scheduled according to participants' preferences and conducted in a quiet environment that respected personal space, with each session lasting between 10 to 30 minutes depending on the conditions.
Each interview began with a detailed explanation of the study's objectives and methods, followed by semi-structured interviews adhering to relevant principles and frameworks. Interviews with 18 university managers continued until data saturation was reached after 15 interviews. Data analysis began concurrently with the interviews, with coding performed using MAXQDA 10 software. The research team completed the schematic diagram extracted from the software, based on literature reviews and qualitative interviews. The draft entrepreneurial model for telemedicine in clinical medicine was finalized and validated during a three-hour expert panel session with 8 specialists.
Ethical considerations included obtaining ethical approval codes, coordinating interviews with university officials and faculty members, and maintaining honesty and integrity in the use of sources and the rights of participants. Participants consented to the recording of interviews, and confidentiality was ensured by assigning codes for participant identification. Participants were informed of their right to withdraw from the study at any time.
4. Results
In the initial search, a total of 26,421 articles were identified. In the first stage, after reviewing titles and abstracts, 13,401 articles were excluded due to duplication or lack of full text. In the second stage, another 10,472 articles were deemed irrelevant based on title and abstract review. In the third stage, after a thorough examination, 2,535 articles were excluded for not addressing remote medical indices. No additional articles were found using study sources. Ultimately, 13 articles focusing on remote medical indices were identified. Content analysis was conducted on these articles to identify the main themes and features of new communication technologies, which then informed the development of a semi-structured interview guide consisting of 10 questions.
After conducting the interviews, content analysis was used to analyze the qualitative data. Through coding and comprehensive data analysis, 357 codes were identified, resulting in 10 main themes and 57 sub-themes for content analysis.
Interview analysis revealed that participants discussed various aspects:
- In the technology and information technology domain: Resource provisioning, equipment and supplies, energy supply, energy sustainability, access to electronic health records, data aggregation, data volume, data security, data retrieval, internet bandwidth, monitoring, automation, infrastructure and hardware, software design for different age groups, integrated software design, team collaboration, condition-responsive software, easy software access, online support, and the creation of virtual meeting rooms within software.
- In human resource management: Service and support personnel, training personnel, legal and medical personnel.
- Regarding time: Service speed, management of specific and time-sensitive conditions, 24-hour service provision, simultaneous and non-simultaneous treatment.
- In geography: Distance, infrastructure in underserved areas, access, and extent.
- In supervision and support: Adherence to high-touch laws, data privacy, fairness, and accountability.
- In conditions and disease type: Specific conditions and influential treatment variables.
- In service type: Surgery, elderly care, acute patient care, health and treatment, and counseling.
- Budget discussion: Capital, cost, and profitability.
- In cultural promotion: Awareness and acceptance, encouragement, advertising and promotion, motivation creation, clinical education, non-clinical education, age, education, and facility access.
- Entrepreneurship discussion: Threats and opportunities, creativity and innovation, development and flexibility, and risk-taking.
This comprehensive analysis helped to identify key areas for the design of an entrepreneurial model using remote communication technologies in clinical medicine.
Table1 shows primary and sub-themes and quotations from study participants.
| Theme and Sub Theme | Quotation |
|---|---|
| Technology and information technology | |
| Ability to create a meeting room in the software | P 10: “Physicians and other healthcare staff need to view and review X-ray images, lab work, notes, and other video and visual content. Remote specialized teams must collaborate in a virtual meeting room to determine the best course of treatment.” |
| The possibility of online support | P 5: “To implement consulting services and primary care levels, there must be online support services available.” |
| Easy access to software | P 1: “Today, artificial intelligence technology has transformed the world and introduced various software in this field, such as self-care software, mental health care software, and software used in remote surgeries. For this software to be effective, it must be easily accessible.” |
| The software responds to the conditions | P 18: “With the design of intelligent communication software using artificial intelligence, if a patient has a question and the doctor is not available to respond online, the software bot can answer the patient's questions with pre-designed questions and answers.” |
| Software design with the ability of cohesion and team building | P 5: “Several minds are better than one, especially in healthcare. Considering this, technologies like Insta, Share and mobile devices, including smartphones, tablets, and laptops, should be used to create cohesive teams. |
| Software design for all ages | P6: “To increase the popularity of using remote communication methods, software should be designed to match each patient's age, education, and needs. For example, elderly individuals and children can easily communicate with their doctors through beginner-level training if needed.” |
| Infrastructure and hardware | P18: “In telemedicine, a series of technologies, including hardware, software, and auxiliary equipment, must be used for medical activities.” |
| Make smart | P11: “We must move towards smartening tasks; artificial intelligence simplifies various processes such as data analysis, image recognition, natural language processing, and virtual consultation, enhancing telemedicine.” |
| Monitoring | P11: “Healthcare professionals working in doctors' offices, emergency rooms, hospitals, and surgery centers need display technology to be efficient and well-informed, making the most of appointments and sessions by supporting multiple providers on one screen in the least amount of time.” |
| Internet bandwidth | P3: “Establishing a communication network is one of the requirements for using telemedicine. Choosing the most appropriate network depends on several factors, including the required bandwidth, the type of connection between two points (e.g., sea to land), network costs in the area, and the availability of local support services.” |
| Data and information recovery | P4: “In this method, it is necessary to create an electronic record with a unique code for each patient so that the doctor can easily access the patient's history and document the treatment process during follow-ups.” |
| Data privacy | P15: “Since patient data and information are exchanged among doctors and various service levels in this initiative, patient data privacy and confidentiality must be protected.” |
| Data volume | P15: “Like any other communication program, telemedicine requires data exchange. Data usage may vary based on internet connection, frames per second, screen sharing, sound, and clarity maintained during video calls.” |
| Aggregate information | P18:” The availability of patient data is crucial for the successful implementation of telemedicine services. Recent advancements in cloud management offer opportunities to collect, store, and access medical information from virtually anywhere at a lower cost.” |
| Access to electronic health records | P12:” One of the necessities of telemedicine is advanced access to comprehensive, accurate, and complete patient health records.” |
| Energy supply | P2:” The emergence of telemedicine has transformed the way medical care is received, especially in remote and underserved areas. However, since connectivity issues persist in these areas, ensuring a continuous power source to keep telemedicine systems active has become a challenge.” |
| Energy sustainability | P8:” Many areas lacking reliable power infrastructure face challenges in providing remote healthcare services. In such cases, solar energy or any other sustainable and reliable source should be used as a solution.” |
| Equipment and supplies | P15:” Telemedicine equipment can play a vital role in providing accessible and quality care to patients and streamlining operations in healthcare centers.” |
| Human resources management | |
| Service and support force | P16:” To maintain telemedicine services and solve the issues and challenges that arise in this type of service, both users and providers will need support, ideally available 24 hours.” |
| Training force | P17:” Given the development of existing technologies in telemedicine and the advancements in artificial intelligence, new and better software and methods are being created every day. For users and providers to become familiar with the latest technologies, there must be personnel to provide the necessary training.” |
| Legal force | P6:” As you are aware, there may be errors and risks in this technology; patients may be harmed due to various factors. To determine the responsibilities arising from these incidents and ensure no rights of the patient or provider are violated, there must be legal personnel defined for this purpose.” |
| Qualified physicians | P2:” Not all providers are qualified to use this technology. Physicians and healthcare professionals need to have or develop certain skills to stay updated and effective in performing their duties using remote health technology.” |
| Time | |
| Service speed | P1:” In health services, time is a crucial factor. The provider team must make decisions based on available evidence within a short period. Therefore, the speed of service delivery must be ensured.” |
| Management of special and time-sensitive conditions | P4:” In critical situations such as wars, natural disasters, or urgent and emergency needs, telemedicine can be effective in the shortest time and expedite the service delivery process.” |
| 24 hours service | P5:” Telemedicine guarantees access to doctors and treatment solutions around the clock.” |
| Simultaneous and asynchronous treatment | P17:” One of the important applications of telemedicine is that patients can share their clinical documents and preferences with their doctors through communication software and store them there. The doctor can provide necessary guidance at the first opportunity, and this can happen simultaneously if the doctor is available. These documents are often used for patient care or follow-up care.” |
| Geography | |
| Distance | P11:” With this communication method, a patient thousands of kilometers away from the doctor can receive quality services without dedicating a lot of time and cost to access medical services, thus eliminating distance as a limitation to patient health.” |
| Infrastructure in deprived areas | P2:” The use of telemedicine technology in underserved areas is limited due to lack of conditions and infrastructure. To develop this technology and improve the health of all people, equipping and providing infrastructure in underserved areas must be prioritized by the health system.” |
| Access | P16:” The COVID-19 pandemic caused even those who previously did not use remote technologies to turn to them. Studies have shown that since patients started using telehealth, they have had better access to care.” |
| The extent | P15:” Given the development of technology and the expansion of virtual services, geographical boundaries are no longer relevant, and healthcare services are provided in a broader geographical area.” |
| Monitoring and support | |
| Attention to upstream rules | P2:” Before implementing telemedicine plans, legal matters must be clarified. The legislation must be based on the higher laws of the countries, such as how costs are paid, issuing certifications, and commitments in this field.” |
| Attention to data confidentiality | P3:” Patients must be assured that in this method, their information is recorded and maintained solely by the relevant doctor, and the security of the communication software ensures that other people cannot access the electronic record and misuse patient information |
| Justice oriented | P17:” Various segments of society, regardless of their economic and social status, can easily consult their desired doctors. The infrastructure and financial resources for receiving services must be distributed based on need, not supply.” |
| Responsiveness | P2:” Responsibility must be clearly defined in this method. The question that can be raised is when the patient and doctor are at a distance, if an error or mistake occurs during the process, for example, if there is an issue with the operation of auxiliary devices, who is to blame? The specialist doctor, the hospital, the company selling the devices and accessories, or the network service provider?” |
| Condition and type of disease | |
| Special condition | P9:” Providing health services in special conditions such as wars, emergencies, drills, etc., can be done more easily, cost-effectively, and broadly with this method. |
| Variables affecting treatment | P4:” The treatment of diseases depends on having quality equipment, skilled workforce, and facilities. Telemedicine, in addition to having all these conditions, by preserving the golden time, increases the likelihood of successful treatment.” |
| Type of service | |
| Surgery | P3:” It is true that this practice is not yet widespread in many countries, but one of the most important tasks is surgeries that are performed remotely using advanced robots.” |
| Elderly care | P18:” Telemedicine is a convenient and cost-effective way to provide healthcare services to the elderly, who may have significant health needs or mobility and transportation limitations, making access to healthcare provider offices difficult.” |
| Serving acute patients | P1:” Since experienced and skilled doctors are in various locations and physical access to them is difficult, telemedicine can enable patients with urgent needs to benefit from their services.” |
| Healthcare | P4:” A wide range of health services, from education and consultation to advanced surgeries, can be provided through telemedicine.” |
| Counseling | P4:” Using email, video software, conferences, and virtual communication, many consultations and training can be provided remotely. |
| The budget | |
| Fund | P13:” The cost of telemedicine equipment can vary from a few hundred to several thousand dollars depending on the specific devices and the number needed. Additional costs such as software programs, training, and maintenance should also be considered.” |
| Cost | P8:” This method (telemedicine) reduces intercity travel and prevents unnecessary visits, leading to cost reduction.” |
| Profitability | P3:” Providing services at different levels, reducing overhead costs, and travel expenses are among the financial benefits of using and developing telemedicine.” |
| Cultural promotion | |
| Awareness and acceptance | P16:” Explaining the positive aspects and benefits of telemedicine to the public, convincing them of the possibility of providing remote services when needed, and ensuring the quality of services in this method can increase public acceptance of this technology.” |
| Persuasion | P3:” Encouraging and informing healthcare staff and patients in need of non-in-person services about the significant reduction in unnecessary travel and costs due to telemedicine will be very beneficial in developing this initiative.” |
| Advertisement and promotion | P8:” Given the low awareness among the general public, especially the less educated population, about the existence and use of telemedicine, health authorities can use mass media like television and radio to inform the public about the benefits of this technology and facilitate its promotion.” |
| Motivating | P10:” By comparing the benefits of telemedicine with existing classic methods and explaining the use cases of this type of communication, motivation to use this method will be created among the people.” |
| Clinical education | P13:” Low knowledge and awareness of how telemedicine works among healthcare providers, insurance companies, and patients are significant obstacles. Educating and increasing knowledge for these stakeholders will be very effective.” |
| Non-clinical training | P11:” Another important factor is the level of skill required to work with this technology. For telemedicine to be used effectively, physicians and patients must possess a certain level of skill and knowledge. Therefore, there is a need to train both parties for the effective use of this technology.” |
| Age | P2:” Young people have more capacity to accept and use remote medicine and health compared to older people. But the treatment needs are more felt in the elderly due to their physical conditions and having chronic diseases. Measures should be taken to improve the skills of the elderly in this area.” |
| Education | P13:” With the increase in the level of education, the use of virtual space and access to online services becomes easier. It is recommended that people with a low level of education also receive training on the use of modern technologies for online communication with doctors.” |
| Having facilities | P4:” The use of this technology requires basic equipment and facilities. To expand telemedicine, especially in deprived areas; Baycity equipment, hardware and software should be provided in the service delivery environments and people's access to these facilities should be facilitated.” |
| Entrepreneurship | |
| Threats and opportunities | P11:” Telemedicine creates a series of opportunities, such as speeding up the launch of the referral system, speeding up the patient's access to treatment, etc., but it also creates a series of threats, such as the possibility of lowering the quality of service delivery, the loss of patient privacy.” |
| Creativity and innovation | P15:” Among the latest innovations in telemedicine technology is artificial intelligence, which is helping medical providers work more efficiently and even using robotics to deliver specialized care to places they've never been. |
| Development and flexibility | P1:” Telemedicine can be used for a wide range of medical examinations and procedures, including electronic prescribing, video consultations, and remote monitoring. As a result, physicians may be able to meet the specific needs of patients and provide them with a wider variety of services. Body presentation” |
| Risk taking | P14:” Despite the many benefits of remote communication, in some cases, without creating the necessary infrastructure, there may be threats to the health of patients, for example, a distance is created between the patient and the doctor, and the possibility of correct diagnosis and prescription is denied to the doctor, and it is possible that some people may not have this type of communication. Replace visiting the doctor in person even in acute cases” |
Abbreviation: P, participant.
Table 2 demonstrates the frequency of sub-themes in semi-structured interviews, categorized by interview participants. Table 2 shows that all interviewees mentioned sub-themes such as "infrastructure and hardware," "internet bandwidth," "access to electronic health records," "equipment and supplies," "data privacy," "qualified physicians," and "counseling."
| Theme and Sub Theme | Participants | Total | Percent | |||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 | 13 | 14 | 15 | 16 | 17 | 18 | |||
| Technology and information technology | ||||||||||||||||||||
| Ability to create a meeting room in the software | * | * | * | * | * | * | * | * | * | * | * | 11 | 61 | |||||||
| The possibility of online support | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 15 | 83 | |||
| Easy access to software | * | * | * | * | * | * | * | * | * | * | * | * | * | 13 | 72 | |||||
| The software responds to the conditions | * | * | * | * | * | * | * | * | 8 | 44 | ||||||||||
| Software design with the ability of cohesion and team building | * | * | * | * | * | * | * | * | * | * | * | * | * | 13 | 72 | |||||
| Software design for all ages | * | * | * | * | * | * | * | * | * | 9 | 50 | |||||||||
| Infrastructure and hardware | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 18 | 100 |
| Make smart | * | * | * | * | * | * | * | * | * | * | * | * | 12 | 66 | ||||||
| Monitoring | * | * | * | * | * | * | * | * | 8 | 44 | ||||||||||
| Internet bandwidth | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 18 | 100 |
| Data and information recovery | * | * | * | * | * | * | * | * | * | * | * | * | 12 | 66 | ||||||
| Data privacy | * | * | * | * | * | * | * | * | * | * | * | * | * | 13 | 72 | |||||
| Data volume | * | * | * | * | * | * | * | * | * | * | * | * | 12 | 66 | ||||||
| Aggregate information | * | * | * | * | * | * | * | * | * | * | * | * | * | 13 | 72 | |||||
| Access to electronic health records | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 18 | 100 |
| Energy supply | * | * | * | * | * | * | * | * | * | * | 10 | 55 | ||||||||
| Energy sustainability | * | * | * | * | * | * | * | * | 8 | 44 | ||||||||||
| Equipment and supplies | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 18 | 100 |
| Human resources management | ||||||||||||||||||||
| Service and support force | * | * | * | * | * | * | * | * | * | 9 | 50 | |||||||||
| Training force | * | * | * | * | * | * | * | * | * | * | * | 11 | 61 | |||||||
| Legal force | * | * | * | * | * | * | * | 7 | 38 | |||||||||||
| Qualified physicians | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 18 | 100 |
| Time | ||||||||||||||||||||
| Service speed | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 16 | 88 | ||
| Management of special and time-sensitive conditions | * | * | * | * | * | * | * | 7 | 38 | |||||||||||
| 24 hours service | * | * | * | * | * | * | * | * | 8 | 44 | ||||||||||
| Simultaneous and asynchronous treatment | * | * | * | * | 4 | 22 | ||||||||||||||
| Geography | ||||||||||||||||||||
| Distance | * | * | * | * | * | * | * | * | 8 | 44 | ||||||||||
| Infrastructure in deprived areas | * | * | * | * | * | * | * | * | * | * | * | 11 | 61 | |||||||
| access | * | * | * | * | * | * | * | * | * | * | 10 | 55 | ||||||||
| The extent | * | * | * | * | * | * | * | * | * | 9 | 50 | |||||||||
| Monitoring and support | ||||||||||||||||||||
| Attention to upstream rules | * | * | * | * | * | * | * | * | * | 9 | 50 | |||||||||
| Attention to data confidentiality | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 18 | 100 |
| Justice oriented | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 14 | 77 | ||||
| Responsiveness | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 15 | 83 | |||
| Condition and type of disease | ||||||||||||||||||||
| Special condition | * | * | * | * | * | * | * | * | * | * | * | * | 12 | 66 | ||||||
| Variables affecting treatment | * | * | * | * | * | * | * | 7 | 38 | |||||||||||
| Type of service | ||||||||||||||||||||
| Surgery | * | * | * | * | * | * | * | * | * | * | * | * | 12 | 66 | ||||||
| Elderly care | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 15 | 83 | |||
| Serving acute patients | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 15 | 83 | |||
| Healthcare | * | * | * | * | * | * | * | * | * | * | * | 11 | 61 | |||||||
| Counseling | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 18 | 100 |
| The budget | ||||||||||||||||||||
| Fund | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 16 | 88 | ||
| Cost | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 15 | 83 | |||
| Profitability | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 14 | 77 | ||||
| Cultural promotion | ||||||||||||||||||||
| Awareness and acceptance | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 14 | 77 | ||||
| Persuasion | * | * | * | * | * | * | * | * | * | * | 10 | 55 | ||||||||
| Advertisement and promotion | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 14 | 77 | ||||
| Motivating | * | * | * | * | * | * | * | * | * | 9 | 50 | |||||||||
| Clinical education | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 16 | 88 | ||
| Non-clinical training | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 15 | 83 | |||
| Age | * | * | * | * | * | * | * | * | * | * | 10 | 55 | ||||||||
| Education | * | * | * | * | * | * | 6 | 33 | ||||||||||||
| Having facilities | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 17 | 94 | |
| Entrepreneurship | ||||||||||||||||||||
| Threats and opportunities | * | * | * | * | * | * | * | * | * | * | * | * | * | * | 14 | 77 | ||||
| Creativity and innovation | * | * | * | * | * | * | * | * | * | * | * | * | 12 | 66 | ||||||
| Development and flexibility | * | * | * | * | * | * | * | * | * | * | 10 | 55 | ||||||||
| Risk taking | * | * | * | * | * | * | * | 7 | 38 | |||||||||||
Table 2 demonstrates the frequency of sub-themes in semi-structured interviews, categorized by interview participants. Table 2 shows that all interviewees mentioned sub-themes such as "infrastructure and hardware," "internet bandwidth," "access to electronic health records," "equipment and supplies," "data privacy," "qualified physicians," and "counseling."
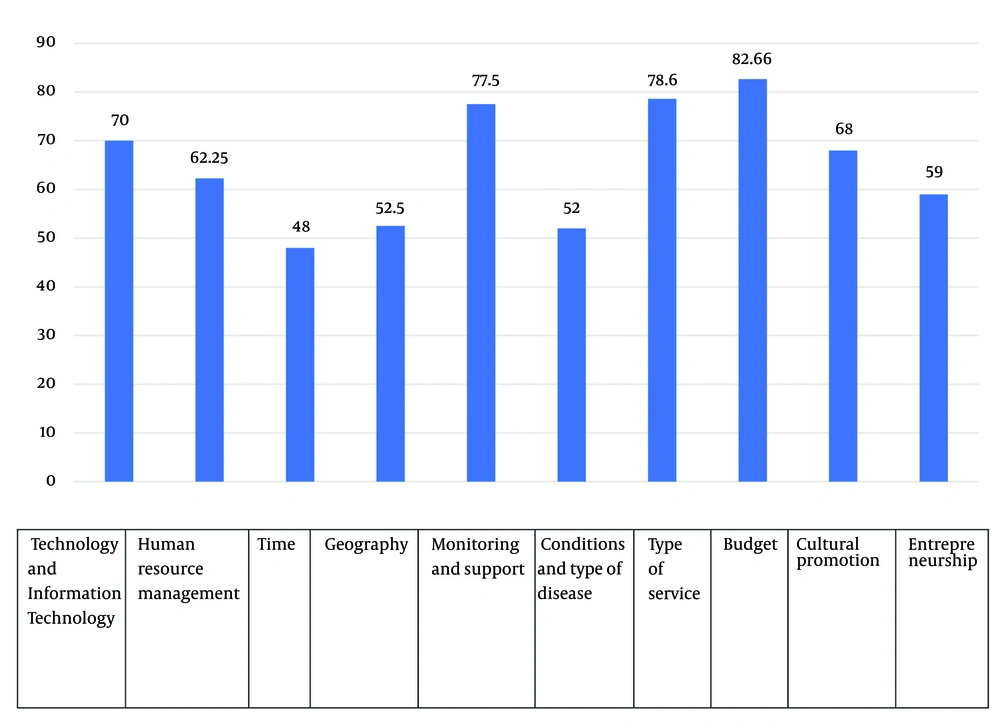
Figure 1 illustrates the percentage frequency of themes related to the requirements and features of remote medical deployment as discussed by study participants.
Based on Table 2 and Figure 1, the frequency of sub-themes and the percentage frequency of themes regarding requirements and features of remote medical deployment prioritized the themes as follows: "Budget," "Type of Service," "Monitoring and Support," "Technology and Information Technology," "Cultural Promotion," "Human Resource Management," "Entrepreneurship," "Geography," "Conditions and Type of Disease," and "Time."
5. Discussion
This study aimed to design an entrepreneurial model for innovative remote communication technologies in clinical medicine. Telemedicine leverages information and communication technologies to deliver healthcare services to individuals who are distant from healthcare providers. Previous studies in this field, most of which were conducted around 2017, primarily focused on security, architecture, feasibility assessments, implementation experiences, awareness, stakeholder attitudes, and the application of telemedicine in clinical settings. The results highlighted several challenges, including a lack of awareness, insufficient facilities and equipment, inadequate budget allocation, inappropriate software and hardware infrastructure, and weak privacy protection methods. These findings underscore the need for restructuring and developing specific guidelines for implementing this technology (14-25).
Various obstacles to the implementation of remote healthcare were categorized into three perspectives:
(1) Communication issues: These include diverse technical standards and inadequate communication infrastructures.
(2) Medical challenges: These encompass disparities between national and international communication systems, cultural differences among healthcare providers, methodological variations, and differing medical standards.
(3) Socio-economic barriers: These include disparities in medical technology and equipment, administrative and political obstacles, language and literacy differences, cultural differences in accepting healthcare providers, issues related to payment and reimbursement, legal concerns in medicine, lack of patient trust in the accuracy of this method, inadequate patient-physician communication, startup costs, and time constraints.
Overall, the extracted indices from various studies pointed out recurring issues across entrepreneurial, social, economic, political, and cultural domains. These issues include service type (consultation, treatment, care, etc.), infrastructure development, budget and costs, time, human and non-human resource supply chains, technology-related factors, healthcare data privacy principles and regulations, clinical training, technology use training, software and application design for telemedicine service providers and recipients, treatment effectiveness variables, supervision and support, promotion, persuasion, and cultural advocacy for telemedicine utilization, as well as its development and flexibility.
According to various entrepreneurial definitions, entrepreneurs identify opportunities and threats in business and innovate creatively. Entrepreneurial individuals recognize economic opportunities in remote healthcare and novel technologies, which necessitate commercialization.
Currently, healthcare faces challenges related to geography, access, service speed, equipment limitations, and other constraints. Fortunately, with the aid of technology and innovative communication technologies, remote healthcare can address many of these limitations and deficiencies. It has the potential to provide more equitable and higher-quality services at lower costs, particularly to patients and the elderly in medically underserved communities, leading to improved public welfare and satisfaction among both service providers and recipients.
Various factors influence the implementation of telemedicine across different healthcare systems globally, and our country's challenges with implementing this technology are no exception. Overall, the benefits of remote healthcare outweigh the existing obstacles, which policymakers, financial leaders, and healthcare managers must address seriously to create a suitable environment for utilizing innovative medical technologies such as telemedicine within healthcare systems (19, 26-33).
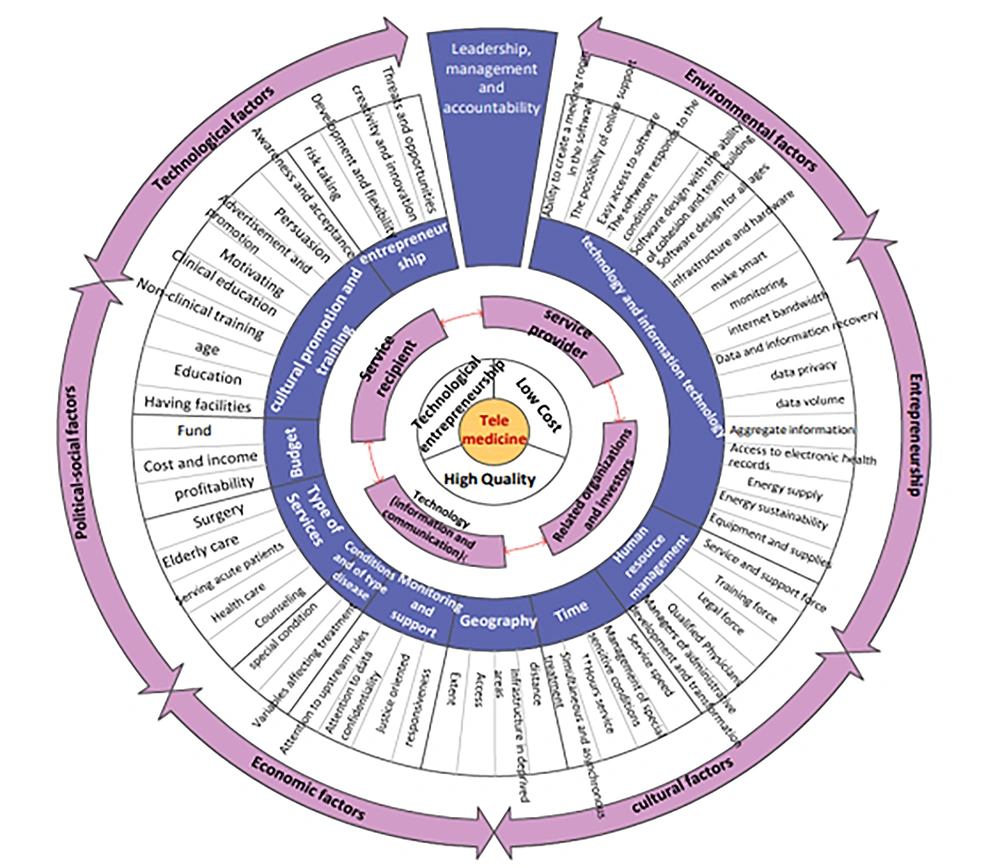
This research employed specific tools and methods to extract influential components of entrepreneurship, innovative communication and information technologies, and telemedicine (Figure 2).
By leveraging existing models and identifying the entrepreneurial components of innovative communication technologies and remote clinical medicine in healthcare, this study aimed to intelligently streamline remote medical treatment and healthcare through innovative communication and information technologies. The goal was to subsequently change lifestyles, improve quality of life, enhance social welfare, and ultimately achieve public satisfaction. The study also took into account sustainable development in designing an entrepreneurial model for innovative remote communication technologies in clinical medicine.
5.1. Limitations
The study faced several limitations, including the difficulty in accessing expert opinions in the fields of entrepreneurship, telemedicine, and innovative communication and information technologies. Additionally, the process of interviewing managers was time-consuming, with some individuals reluctant to express explicit opinions.
In implementing and expanding telemedicine, several barriers and challenges were identified, such as inadequate communication infrastructures and basic facilities, particularly in underserved areas. Addressing these challenges requires significant investment and government cooperation and support. Establishing telemedicine in these regions could greatly enhance service delivery, reduce transportation and other related costs, and allow for the sharing of diverse medical expertise.
Another significant concern is the general public's unfamiliarity with innovative communication technologies and the lack of acceptance of telemedicine. Many people believe that medical consultations must be conducted face-to-face to ensure the effectiveness of treatment, a belief that is also held by some physicians. Therefore, cultivating awareness among both the public and healthcare providers is essential for the broader acceptance and approval of telemedicine.
Service providers and recipients also have concerns regarding costs, data privacy, security, and potential operational issues such as internet disconnections and medical equipment malfunctions. To address these concerns, clear laws and regulations need to be established to protect the interests of both service providers and recipients.
5.2. Conclusions
The Ministry of Health, Treatment, and Medical Education, supported by the government and media, can play a crucial role in encouraging and supporting the implementation and development of telemedicine. By providing the necessary tools, techniques, and support, they can foster a sense of need for acceptance, innovation, and change, ultimately improving the sustainable quality of telemedicine systems.