1. Context
Aiming to provide patients with comprehensive and holistic treatment, the synergy among various professions within hospital health teams is essential. This collective, which includes doctors, nurses, nursing technicians, nutritionists, physiotherapists, and, not least importantly, dentists, is fundamental for an integral health approach (1, 2). In military hospital settings, a significant gap is evident: The absence of the dentist as an active member of the clinical team. The practice of Hospital Dentistry (HD) challenges this paradigm, advocating for the indispensable inclusion of the dentist in the clinical core of hospitals. This professional, equipped with specific competencies, plays a crucial role in the care of hospitalized patients, focusing on the diagnosis and eradication of infectious foci, whether acute or chronic in nature, in addition to preventing opportunistic infections and relieving painful symptoms (3, 4).
To preserve oral health, HD implements a range of essential practices, including accurate diagnoses, the establishment of preventive protocols, biofilm management through chemical (antiseptics) and mechanical techniques, surgical procedures, and the treatment of oral lesions. These interventions are vital not only for maintaining oral health but also for reducing hospital costs, decreasing the length of hospital stays, and preventing complications that impact the patient's systemic and overall well-being (5-8). It is crucial to distinguish these practices from those of oral and maxillofacial surgeons, whose focus is predominantly on trauma treatment (9, 10).
The Armed Forces, comprising the Navy, Army, and Air Force, are permanent and regular national institutions dedicated to providing comprehensive care to hospitalized military patients and their families, while adhering to a hierarchical and disciplined structure. The integration of HD into the interdisciplinary health practices of the Armed Forces represents a promising yet underexplored field in current scientific literature. Although studies emphasize the importance of a holistic health approach, including oral health as a critical component of overall well-being, the specificity and depth of HD's contributions within the military context remain largely unexamined. Specifically, the distinction between general dental practices and the specialized interventions provided by HD in military hospital settings has not been sufficiently addressed.
Additionally, existing literature rarely explores how HD practices directly affect health indicators of military patients, such as reducing hospitalization time, preventing postoperative complications, and improving quality of life. This gap highlights the need for more comprehensive studies that not only clarify the role and potential impact of HD in the Armed Forces but also investigate how its integration can enhance health outcomes for military patients and their families. Consequently, this study aims to conduct the first integrative review, combined with a case report, focusing on HD interventions within the Armed Forces and illustrating this approach through a clinical case study conducted in a Brazilian Army hospital.
2. Evidence Acquisition
2.1. Methodological Approach
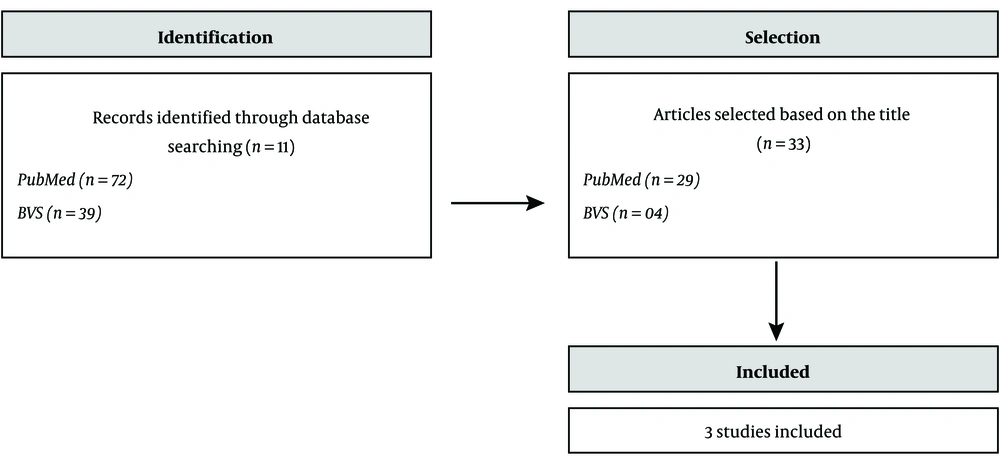
This study employs a mixed-methods approach, combining a case report with an integrative review, aiming to assess the availability of HD services within Armed Forces organizations. To achieve this objective, a detailed search strategy was implemented using the PubMed/MEDLINE and Scielo databases, with Boolean operators applied to refine the results. The specific combination of search terms used was: (Dental) AND (Treatment) AND (Hospital) AND (Dentistry) AND (Medicine) AND (Military Forces).
2.2. Selection Criteria
The inclusion and exclusion criteria for this study were carefully established to guide the literature review. Scientific articles were included without language restrictions and without limitations on the publication date. The focus was directed towards research examining dental interventions conducted in hospital settings, particularly bedside procedures. Regarding the exclusion criteria, studies focusing on clinical interventions performed by oral and maxillofacial surgery teams on patients with facial trauma, specific dental procedures conducted exclusively within military dental practices without integration into the hospital setting, and works not available in full online were excluded. By defining these criteria, the literature review aimed to achieve a balance between being comprehensive and specifically targeting relevant HD practices in military installations, enabling an analysis that is both broad and focused.
2.3. Review Process
To ensure maximum comprehensiveness and minimize the risk of omitting relevant research, the authors also reviewed the bibliographic references of the selected articles. Initially, a preliminary screening was performed based on the titles and abstracts available in the databases to identify publications potentially meeting the established criteria. Subsequently, the full texts of pre-selected articles were reviewed to confirm their adherence to the study's objectives. Finally, the articles included in the review were systematically cataloged by author, year, hospital institution, type of study, and objectives related to HD interventions in the Armed Forces, along with a summary of their main findings and conclusions.
3. Results
3.1. Case Report
The case report presents an 87-year-old male patient diagnosed with a stable pulmonary infection and a suspected odontogenic infection, who was referred for dental evaluation at the Brazilian Army facility in Campinas. The patient faced additional challenges, including normal pressure hydrocephalus, Alzheimer's disease, hypertension, and type 2 diabetes mellitus. He was under an extensive pharmacological regimen that included diovan (valsartan) 80 mg, januvia (sitagliptin phosphate) 50 mg, memantine hydrochloride 10 mg, donepezil 10 mg, quetiapine 25 mg, citoneurin 5 mg, vitamin D3 50,000 IU, and acetylcysteine 600 mg.
The dental clinical examination revealed concerning conditions, such as suppuration and a coronal fracture in the lower right molar, along with dental roots and crowns presenting traumatic edges. An additional X-ray indicated a distal root fracture in the lower left molar, severe cavities, periapical lesions, significant bone loss in the lower right molars, and signs of an infection center around the second lower molar. The diagnosis was further supported by laboratory tests showing leukocytosis and elevated C-reactive protein levels, confirming the presence of an active infectious process.
Based on these findings, an oral surgical treatment plan was developed, which included the extraction of the affected teeth under general and local anesthesia in the hospital's surgical center. This procedure required pre-anesthetic evaluation and laboratory tests in accordance with the protocols established by the hospital's dental team. The dentist in charge, a Lieutenant of the 11th light infantry brigade, led the dental team during the intervention.
After nasal intubation performed by the anesthesiologist and proper patient preparation, the surgical procedure was conducted in the surgical center under local anesthesia. A 2% mepivacaine solution with epinephrine at a concentration of 1:100,000 was used. The team removed teeth with inflammatory or infectious lesions, fractured and residual roots, as well as granulation tissue, and performed ridge regularization using burs under saline irrigation. The wound was sutured with 5 - 0 absorbable thread (P.G.A, BRAUN®, BR), completing the procedure in approximately one hour and thirty minutes.
Following the surgery, the patient spent 24 hours in the intensive care unit (ICU) for monitoring. During the hospital stay, there was continuous interaction between the dental and medical teams, ensuring integrated care. After 7 days of postoperative clinical follow-up, satisfactory healing and resolution of the infection foci were observed. The patient demonstrated significant improvements in feeding capacity and sleep pattern, with the medical team noting a positive impact on his overall systemic condition.
3.2. Literature Review and Discussion
The method for article selection, as depicted in the flowchart in Figure 1, was based on a precise search strategy. By applying the inclusion and exclusion criteria outlined in the methodology of this integrative review, three relevant articles were selected. These articles are organized chronologically in Table 1, which provides details on authors/countries, year, methodology, institution, sample size, objectives, main results, and conclusions.
| Authors (y) | Type of Study | Hospital | Objectives | Case Studies | Main Results | Conclusions |
|---|---|---|---|---|---|---|
| Chiu et al. (2021) (11) | Cohort study | General hospital of the Armed Forces of Taoyuan, Taiwan | To assess whether interventions for dental problems have potential impacts among dialysis patients. | Men and women. endodontic therapy group: 2633 patients and non-endodontic therapy group: 9821 patients | The non-endodontic therapy group had a higher mortality rate than the endodontic therapy group. infectious diseases played a significant role in mortality among dialysis patients. | Appropriate interventions for dental problems may increase survival among dialysis patients. |
| Kim et al. (2020) (12) | Case report | Dental hospital of the Armed Forces capital, Republic of Korea | To assess the applicability of quantifying fluorescence induced by light for the diagnosis and treatment of necrotic lesions in intraoral soft tissues. | A healthy 21-year-old male with pain in the left jaw and limited mouth opening. Diagnosed with necrotic lesion. | The fluorescence method was an effective auxiliary diagnostic tool. A treatment plan was established and monitored in the hospital. | Successful case resolution through conservative treatment. The method allowed for the assessment of progression and determination of the treatment period. |
| Chen et al. (2013) (13) | Case report | General hospital of the Armed Forces of Taoyuan, Taiwan | To report the complete resolution of a pontine abscess in a patient with dental caries and previous dental interventions. | 59-year-old male with a history of dental caries, diagnosed with pontine abscess. | Hemoculture and cardiology evaluations were negative, aiding the diagnosis. | Successful non-surgical treatment of the abscess. Early diagnosis and prompt treatment with corticosteroids and broad-spectrum antibiotics were crucial. |
Hospital dentistry, aimed at providing dental care to hospitalized patients to treat diseases or improve quality of life, remains a scarcely explored area within the context of the Armed Forces. Few studies detail the application of HD in military environments (11-14). This context positions the present article as a pioneering integrative review investigating the practice of HD within the Armed Forces. The findings reveal that dentists and interdisciplinary teams play a fundamental role not only in diagnosing and treating odontogenic conditions but also in preventing potential infectious foci that could impact the patient’s overall health. This level of dental interconsultation is crucial, as it enables the rapid identification and elimination of infections of oral origin, facilitating a more effective focus on treating systemic comorbidities and aiding in the patient’s recovery (13).
An illustrative example of this collaboration is the diagnosis and management of abscesses in the cranial region (13), underscoring the interconnection between oral conditions and broader health complications. Timely intervention in such cases, facilitated by dental interconsultation, is essential for the swift elimination of infections of oral origin, significantly contributing to the focus on systemic comorbidity treatments and enhancing patient prognosis.
A cohort study demonstrated that dental interventions in patients with nephrological disorders, specifically endodontic treatments, are associated with reduced mortality, highlighting the vital role of dentists in hospital environments and the impact of untreated oral disorders on the mortality of patients with chronic kidney disease (11). Furthermore, in patients with liver disease awaiting transplants, it was observed that the evaluation and management of dental foci are critical prior to the transplant procedure due to the increased risk of microbial infections and immunosuppression (14). Individuals with liver disease require precise surgical techniques that address systemic and local hemostatic challenges to effectively prevent complications related to common coagulation disorders in this patient population. This necessitates training a dentist qualified to operate in a hospital environment (15).
In military hospitals, in addition to HD, oral and maxillofacial surgeons treat trauma and perform complex procedures, including orthognathic surgery (8-10, 16). There is a misconception that HD and oral and maxillofacial surgery are indistinct; however, HD seeks to collaborate with other medical specialties in the hospital environment, emphasizing the complementarity between the fields.
Hospital dentistry plays an integral role in treating patients across various hospital settings, including wards, ICUs, operating rooms, outpatient clinics, and emergency departments. This specialty is responsible for diagnosing and treating oral disorders, managing pain, controlling hemorrhages, and eliminating infectious foci, providing a comprehensive approach that connects oral health with the patient's overall well-being (17, 18). In this context, the presence of a dentist in the hospital environment is essential not only to promote oral health but also to prevent oral complications that could impact the patient’s overall recovery. Their role significantly contributes to reducing the length of hospital stays and decreasing the costs associated with medical treatment (19, 20).
Despite the recognized importance of dentists within interdisciplinary teams in military hospitals, there is a gap in documenting this practice in the specialized literature, particularly within the Brazilian context. This observation underscores the need for greater recognition and documentation of the vital role of HD in ensuring the integral health of patients in the military sphere. This integrative review reveals a notable scarcity of literature on the practice of HD within the Armed Forces, highlighting an underexplored area of oral health. The inclusion of dentistry in an interdisciplinary care model is emphasized as a critical element, particularly in documented cases where compromised dental conditions, such as infections, directly influence the prognosis of systemic disorders. This finding underscores the complex interaction between oral and general health, reinforcing the need for an integrated approach in patient treatment.
4. Conclusions
It is clear that there is a need to expand research on HD within the military context to develop advanced techniques and effective practices that can be integrated into interdisciplinary healthcare. Additionally, greater dissemination and awareness of the importance of HD are essential, both among health professionals and the general public, to promote integral health that acknowledges the inseparable connection between oral and systemic health.
Through this review, it is concluded that enhancing and integrating HD into the practices of the Armed Forces would not only improve the oral health of military personnel but also positively impact their overall health and well-being. This underscores the imperative need for further investigations and collaborative efforts in this field.