1. Background
Among professional violinists, neck pain is the second most common musculoskeletal pain reported (1). While playing, violinists raise their left shoulder and bend it to the side. Simultaneously, rotation of the cervical vertebrae C1 to C7 is required to hold the instrument in place with the jaw against the shoulder. This asymmetric posture, maintained over the long term, increases pressure on the neck and shoulder muscles, eventually leading to neck pain (2, 3). Violinists are prone to musculoskeletal damage due to repetitive movements during bowing and playing melodies. Repeated movements and stress on ligaments, tendons, muscles, and fascia result in pain, irritation, burning sensations, and, ultimately, limited mobility (4).
Among musicians, string players are the most vulnerable to these issues. The primary challenges stem from abnormal posture and inadequate posture control. According to research by Lee et al. (as cited by Gallo), the prevalence of musculoskeletal problems among string players ranges between 75% and 95% (5).
The economic and personal costs associated with neck pain are considerable. In 2016, treatment costs for only 154 patients with back and neck pain in the United States amounted to $134.5 billion, marking the highest healthcare expenditure that year (6).
Additionally, neck pain leads to significant productivity losses; in 2012, 25.5 million Americans missed an average of 11.4 workdays per month due to pain. In 2017, the global prevalence of neck pain by age was 1.3551 per 100,000 people, and the incidence was 6.806 per 100,000 people (7).
When muscles become tight, weak, or restricted, an imbalance occurs, leading to damage and alterations in soft tissue, which may disrupt movement patterns. Prolonged abnormal posture and repetitive motions result in musculoskeletal and biomechanical defects (8). Furthermore, neck pain reduces the accuracy of neck movements and proprioception, creating confusion about proper body positioning (9).
The deep flexor muscles of the neck are crucial for maintaining cervical segment stability (10, 11). Electromyography studies of patients with neck pain have demonstrated decreased activity in the deep flexors and compensatory overactivation of superficial flexors such as the sternocleidomastoid and anterior scalene muscles. Craniocervical flexion tests emphasize the significant role of deep and superficial neck muscles in neck pain (11, 12). Such muscular dysfunction is also prevalent in violinists with neck pain (13).
An asymmetrical neck posture has become a necessity for violinists, who must activate deep neck flexors to stabilize the instrument during performance. In violinists experiencing neck pain, superficial muscles interfere with the function of the deep neck muscles. Studies have demonstrated that cervical vertebrae stabilization exercises significantly improve pain, disability, range of motion, and endurance of neck flexors (14-16).
Many articles addressing non-specific chronic neck pain highlight the significant impact of exercises on this condition. However, during the research process, no study was found that specifically compared neck stabilization and yoga exercises among violinists and violists with non-specific chronic neck pain while assessing all the factors mentioned in this study. If such studies exist, their number is likely very small. Furthermore, over the past ten years, the number of articles exclusively examining neck pain in violinists has been notably low. In the research reviewed, studies often focused on a single independent variable or, in cases of comparative studies, differed in the combination of independent and dependent variables from those in the present study (1, 16-20).
Different segments of society are interconnected like links in a chain, with artists, as disseminators of culture and art, forming vital parts of this chain. The impact of neck pain on unemployment, instrument abandonment, and high medical costs is a widespread issue among musicians. Therefore, this investigation was undertaken.
2. Objectives
This study seeks to answer whether stabilization exercises and yoga targeting the neck can effectively improve movement precision, reduce non-specific chronic pain, and enhance the range of motion in the neck region of violinists.
3. Methods
This realization was a semi-experimental study with pre-test and post-test. The present study included 89 violinists with non-specific chronic neck pain.
3.1. Participation
After selecting 45 men, the subjects were divided into three equal groups in terms of 15 subjects in the yoga training group, 15 in the neck stabilization training group, and 15 in the control group. The sampling method was purposeful and available. At first, an experimental study with nearly 10% of the sample size and a variable, the accuracy of head movements, was conducted for one week and then the main project was carried out. Before the project was implemented, participants read and signed a written consent form on how to research and its conditions.
3.1.1 Measure the Range of Motion of the Neck
To measure the range of motion of the neck, neck movements to the back, front, right, and left side of the left rotation and right rotation were used by a universal goniometer. In the check of reproducibility within the tester, the reliability coefficient values for flexion motion 0.94, for extension motion 0.94, for moving the lateral flexion to the left 0.92, for moving the flexion to the right 0.88, for moving the wheel to the right 0.89, and for moving the wheel to the left 0.89 (4). The subject sat calmly in the chair after 5 minutes of warmth and preparation. The middle point of the goniometer was placed in the middle of the ear canal. The fixed arm was perpendicular to the ground, and the moving arm was placed in the direction of the end of the nose. In neck flexion measurement, the subject was asked to move the chin to the sternum. The goniometer axis was placed in the middle of the ear canal, the fixed arm of the goniometer was vertically positioned, and its moving arm was placed in the direction of the nostrils. Also, in measuring the angle of the neck reaction, the subjects were asked to move the chin to the sky.
Measurements were performed at the beginning and endpoints. The lateral flexion amplitude of the neck was calculated quantitatively based on the degree of range of motion of the neck. The middle of the goniometer was placed on the C7 vertebrae. The fixed arm of the goniometer was parallel to the earth's surface, and the moving handle was placed on the outer prominence of the back. The subject was asked to move his ear toward the shoulder. At the beginning and the moment the neck was flexed, the lateral flexion rate was measured and recorded according to the degree of the different categories. The measurement was performed at the vertical or horizontal level and was done by moving from zero degrees. Head to a vertical position and looking in front, the researcher stood behind the subject and chair and placed the goniometer on thirty-seven degrees. The center was placed precisely on the vertex head, the fixed arm of the goniometer parallel to the last line on the subject's side, and the moving arm of the goniometer in line with the tip of the nasal blade. After completing the movement, the displacement was recorded on the goniometer (21).
To measure the accuracy of head movements, the wall plate method was used. The subjects were asked to warm their bodies and necks for 4 - 5 minutes. To measure the accuracy of neck movements or head reconstruction, the subject sat in the chair, the page was hung four by four in front of him at a distance of two meters on the wall. The subject was asked to rely on the chair in a way that would be located along the ruler listed. The taekwondo cap, on which the indicator laser light was attached, was placed on the subject's head.
3.1.2 Visual Pain Intensity Scale
A line of approximately 10 cm is numbered from 0 to 10. The higher the number the patient indicates, the greater the pain intensity. Its validity is excellent, and its reliability is ICC = 0.91 (22).
3.2. Ethical Considerations
Following the principles of research ethics, the research proposal was approved by the Deputy of Research and Technology, and the Ethics Committee approved the study (Ethics ID: IR.SSRC.REC.1401.034). Written informed consent was obtained from all participants. All research participants were assured that their personal information would remain completely confidential and that they could withdraw from the study at any time without any consequences.
3.3. Protocols Used in the Research
3.3.1. Yoga Group
(1) The participant sits in a fixed and relaxed position with closed eyes.
(2) Inhales slowly and turns their head to the right for 4 to 6 seconds.
(3) Exhales slowly and turns their head back to the center for 4 to 6 seconds while creating the sound "Aah."
(4) Inhales slowly and turns their head to the left for 4 to 6 seconds.
(5) Exhales slowly and turns their head back to the center for 4 to 6 seconds while creating the sound "Uu."
(6) Inhales slowly and raises their head straight for 4 to 6 seconds.
(7) Exhales slowly and brings their head back to the center for 4 to 6 seconds while making the sound "Eee."
(8) Inhales slowly, lowers their head, and touches their chest with their chin for 4 to 6 seconds.
(9) Exhales slowly and brings their head back to the center for 4 to 6 seconds while making the sound "Mmm" (14).
3.3.2. Experimental Group Stabilization
Ten minutes a day with a 10-second rest between each set, gradually increasing the number of sets to 6 per day.
- A: Neck extension exercise
- B: Practice
- S: Axial stretching exercise
- C: Rowing practice
- Y: Neck flexion exercise (16)
To measure the range of motion of the neck, movements including flexion, extension, lateral flexion (right and left), and rotation (right and left) were assessed using a universal goniometer. The reliability coefficient values were: Flexion motion 0.94, extension motion 0.94, lateral flexion left 0.92, lateral flexion right 0.88, rotation left 0.89, and rotation right 0.89 (4).
4. Results
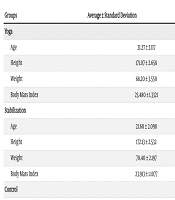
The demographic characteristics of the research subjects are presented in Table 1. The Shapiro-Wilk test was used to check the normality of the data distribution for all variables in this research. A significance level less than 0.05 indicates the normal distribution of the data.
| Groups | Average ± Standard Deviation |
|---|---|
| Yoga | |
| Age | 21.27 ± 2.117 |
| Height | 171.07 ± 2.658 |
| Weight | 68.20 ± 3.550 |
| Body Mass Index | 23.480 ± 1.3321 |
| Stabilization | |
| Age | 21.60 ± 2.098 |
| Height | 172.13 ± 2.532 |
| Weight | 70.40 ± 2.197 |
| Body Mass Index | 23.913 ± 1.1077 |
| Control | |
| Age | 20.93 ± 1.831 |
| Height | 173 ± 2.299 |
| Weight | 67.60 ± 3.135 |
| Body Mass Index | 23.507 ± 7.025 |
In the comparison section, the effect of yoga and stabilization exercises derived from the Bonferroni test was as follows:
- Neck flexion amplitude: Among the mean post-test stabilization and yoga groups (P > 0.05) and control and stabilization groups (P > 0.05), it was found that the percentage of recovery in stabilization exercises was higher than in yoga exercises.
- Neck extension range: There was a significant effect among the mean post-test of control and stability groups (P > 0.05). In the study of averages, it was found that the percentage of recovery in yoga exercises was higher than in stabilization exercises.
- Left lateral bending amplitude: Among the mean post-test control and stabilizer groups (P > 0.05), it was found that the percentage of recovery in stabilization exercises was higher than in yoga exercises.
- Right rotation range: Among the mean post-test control and yoga groups (P > 0.05), it was found that the percentage of recovery in yoga exercises was higher than in stabilization exercises.
- Accuracy of head movements: There was a significant effect between the mean post-test of control and yoga groups (P > 0.05) and control and stabilization groups (P > 0.05). In the study of averages, it was found that the percentage of recovery in yoga exercises was higher than in stabilization exercises.
- Pain intensity: There was a significant effect between the mean post-test of control and yoga groups (P > 0.05) and yoga and stabilization groups (P > 0.05). In the study of averages, it was found that the percentage of recovery in yoga exercises was higher than in stabilization exercises.
5. Discussion
Performing a course of yoga exercises and neck stabilization increases the range of motion, improves accuracy in head movements, reduces pain, and enhances the endurance of neck muscles in neck pain sufferers. By incorporating neck muscle strengthening exercises, including strength exercises, the function of the connective tissue around the neck area can be improved. Strengthening the spine's muscles enhances bone muscle function and decreases pain. Analytical results in Tables 2 and 3 demonstrate that stabilization exercises and yoga targeting the neck region had a positive impact on movement accuracy, range of motion, and pain reduction in the neck region of the research participants.
| Variables | Effect Size | Significance Level | F | Average of Squares | Degrees of Freedom |
|---|---|---|---|---|---|
| Intensity of pain | 0.636 | 0.001 | 635.786 | 40.678 | 2 |
| Accuracy of head | 0.327 | 0.001 | 12.446 | 11.980 | 2 |
| Flexion | 0.742 | 0.001 | 16.194 | 385.156 | 2 |
| Extension | 0.197 | 0.011 | 5.033 | 193.998 | 2 |
| Right flexion | 0.194 | 0.012 | 4.945 | 95.232 | 2 |
| Left flexion | 0.155 | 0.032 | 3.747 | 63.519 | 2 |
| Right rotation | 0.240 | 0.006 | 5.733 | 65.924 | 2 |
| Left rotation | 0.382 | 0.001 | 12.692 | 287.136 | 2 |
| Variables | Effect Size | Significance Level | t | Difference of Means | Degrees of Freedom |
|---|---|---|---|---|---|
| Intensity of pain | 0.841 | 0.001 | 5.772 | 1.600 | 44 |
| Accuracy of head | 1.85 | 0.001 | 6.013 | 2.467 | 44 |
| Flexion | 0.98 | 0.001 | 10.159 | 12.622 | 44 |
| Extension | 0.86 | 0.001 | 5.653 | 8.788 | 44 |
| Right flexion | 2.13 | 0.001 | 4.080 | 3.444 | 44 |
| Left flexion | 2.30 | 0.001 | 7.807 | 7.133 | 44 |
| Right rotation | 0.811 | 0.001 | 4.321 | 3.800 | 44 |
| Left rotation | 1.16 | 0.001 | 5.638 | 6.267 | 44 |
The normal range of motion in the neck significantly reduces the energy required for neck movements and plays a crucial role in maintaining the correct position of the head. The complexity and variability of short or weak neck muscles mean that any dysfunction in muscles associated with neck movements can impact the neck and, subsequently, the spine, leading to disruption in the kinetic chain. This dysfunction also affects proprioception and accuracy in head movements, which are naturally influenced by the neck. Malfunctioning neck muscles may result in improper movement patterns, further exacerbating issues (14).
Comerford and Mottram stated that round exercises, in addition to reducing pain, also improve coordination between deep and superficial neck flexors. The close relationship between pain intensity and proprioception can be attributed to errors in head reconstruction and pain during neck exercises (23). Knag et al. reported that persistent neck pain causes biomechanical changes in the cervical spine. About 60% of patients with neck pain were reported to exhibit forward head posture, which increases the energy and force demands on the dorsal structures of the neck, such as ligaments, articular capsules, bones, and muscles (24). Palmgren et al. showed that increased forward head posture leads to cervical respiratory dysfunction. Forward head posture causes shortening and atrophy of the sternocleidomastoid muscles, scalene muscles, trapezius, and levator scapulae, thus limiting the range of motion in the neck (25).
Falla et al. demonstrated that patients with neck pain struggle to maintain correct neck and head posture. However, after undergoing neck-specific training, improvements were observed in range of motion, mobility, and accuracy in maintaining head position (12). Argus et al., in their research, stated that the prevalence of musculoskeletal pain among violinists during the past six months was 6.86%. Pain in the neck area accounted for 3.53%, and 50% of participants reported that most injuries were related to the neck, back, and left shoulder. Neck range of motion, particularly in violinists who trained for more than one hour daily, was significantly affected due to repetitive movements in the upper body during practice (26). Li et al. assessed the effect of stabilization exercises on pain, ability, strength of respiratory muscles, and range of motion. After six weeks of training, they reported significant improvements due to stabilization exercises (27). Arif et al., in a meta-analysis and systematic review, examined the effects of yoga exercises on chronic neck pain compared to other interventions (such as Pilates and CAM exercises). While all methods were effective in reducing pain, disability, and improving neck range of motion and quality of life, the effect of yoga was considered to be above average (28).
5.1. Conclusions
Based on Table 2, the differences between groups were evaluated using analysis of covariance (MANCOVA) and the Bonferroni test. Additionally, in Table 3, intragroup differences were analyzed using the paired t-test. In the analysis of covariance, the pre-test result was considered as a covariate (intervening variable). The paired t-test was analyzed with Cohen's coefficient (Cohen's d).
The results of this study indicate that strengthening the lateral flexors, deep internal neck muscles, and extensors of the neck vertebrae significantly increases the likelihood of pain reduction. Consequently, the yoga and stabilization exercise protocols presented in this study are validated as non-invasive, drug-free, and surgery-free methods. It is recommended that therapists in physical therapy, rehabilitation movement clinics, well-being centers, occupational therapy centers, and related fields use the methods described in this research to reduce non-specific neck pain in patients.