1. Background
Iran has faced economic and international policy turmoil in recent years, exacerbated by intensified sanctions and the outbreak of COVID-19. These conditions have resulted in both direct and indirect deaths (1). Razavi Khorasan, a cultural and religious province located near Afghanistan and Turkmenistan in Iran's northeastern region, is one of the nation's largest. Due to these strategic conditions, particularly Afghanistan's recent issues and its massive migration, the residents of our province have suffered significantly. The combination of these problems could result in 61,949 deaths in 2020 - 2022, while the estimated number was 43,600.1 (36,102.5; 51,097.7). This indicates that, for 2021 and 2022, the total death count exceeded the projected death count by 33.35% and 51.33%, respectively. Additionally, there were 16,633 deaths from infectious and parasitic diseases, including COVID-19, in 2020 - 2022, with an estimated death count of 12,512.9 (0; 28,992.4), resulting in higher-than-expected death counts by 1,199.06 in 2021 and 1,740.99% in 2022 (1). The situation is more sensitive to demographic characteristics such as age and gender. In the first year of the COVID-19 outbreak, males experienced higher mortality, but in the second year, female mortality increased exponentially. Initially, the elderly were more susceptible, but in the second year, individuals aged 16 - 64 (and children) experienced greater mortality. Different causes of death have varying mortality rates (MRs), however (1). Summary measures of population health (SMPH) are necessary for assessing health profiles, diseases, injuries, and deaths, but they no longer adequately reflect communities' health during times of demographic and epidemiological transition (2). Accurate information about these events, their etiology, and trends is crucial for reinforcing policies and making appropriate decisions. Consequently, both the level of health and its distribution across society can be measured using a limited number of quantitative indices, such as the number of years lost due to disease (YLLs), a measure of the global burden of disease (GBD) (2).
2. Objectives
As a result of the major changes in community health during those four years (two before and two during the outbreak of COVID-19), we aim to identify the neglected areas based on standard expected years of life lost (SEYLL) by age and sex groups.
3. Methods
3.1. Data Sources
Based on the yearly vital statistics reports (2018 - 2022), we analyzed death counts by gender and age, as well as specific causes of death. Using YLLs, we re-ranked the causes of death. Our estimate of premature death included all deaths, cardiovascular deaths (ICD-10: I00-I99), certain infectious and parasitic diseases (ICD-10: A00-B99), and positive COVID-19 lab results (ICD-10: U07.1). The assignment of U07.2 should be given to patients with negative COVID-19 lab results where physicians confirm the diagnosis as "COVID-19". Other categories included cancers and neoplasms (ICD-10: C00-D48); injuries, unintentional and transport accidents (ICD-10: W00-X59, Y40-Y98 & V00-V99); diseases of the digestive system (ICD-10: K00-K93); diseases of the respiratory system (ICD-10: J00-J99); endocrine, nutritional, metabolic diseases, and immunity disorders (ICD-10: E00-E90); diseases of the genitourinary system (ICD-10: N00-N99); and diseases of the nervous system (ICD-10: G00-G99).
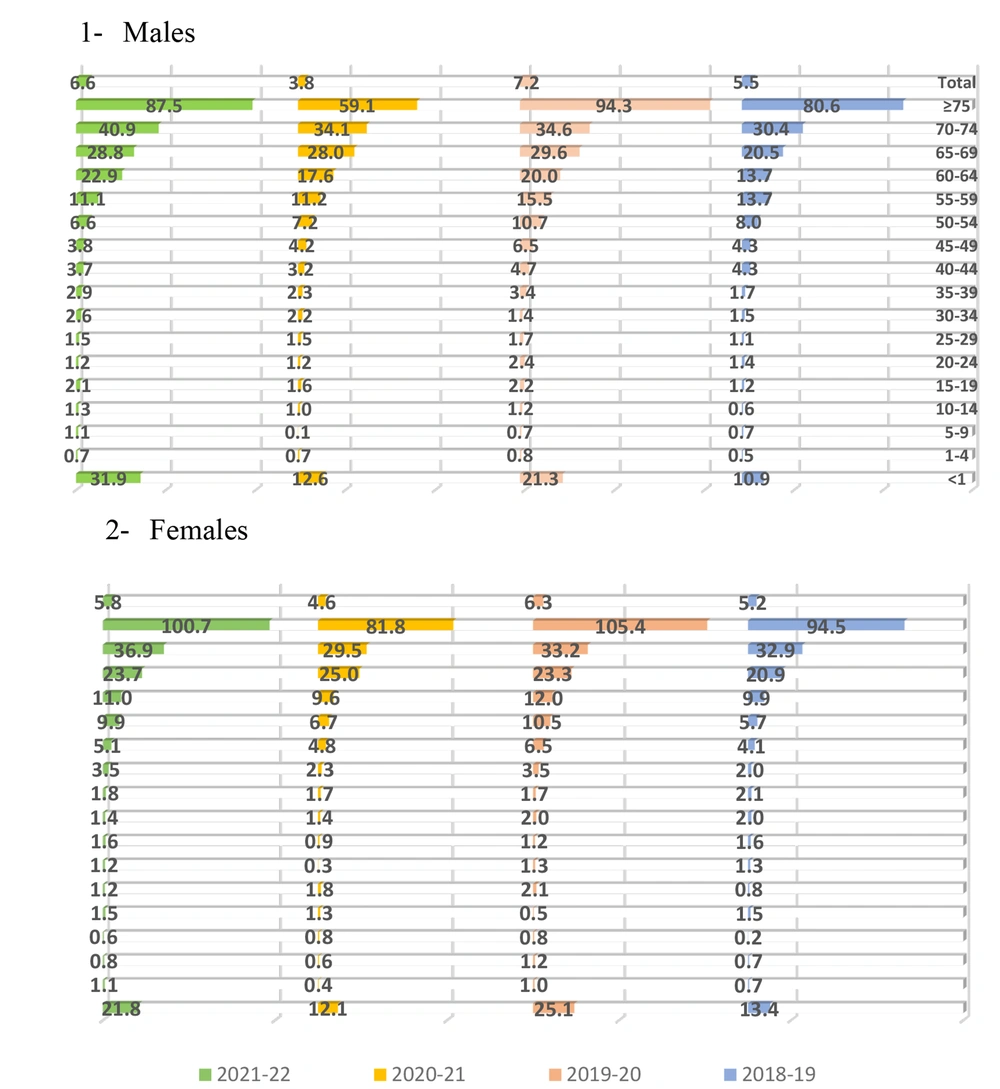
We grouped the data by seventeen-year age groups (< 1 year, 1 - 4 years, 5 - 9 years, 10 - 14 years, 15 - 19 years, 20 - 24 years old, 25 - 29 years old, 30 - 34 years old, 35 - 39 year old, 40 - 44 year old, 45 - 49 year old, 50 - 54 year old, 55 - 59 year old, 60 - 64 year old, 65 - 69 year old, 70 - 74 year old, and 75+ years old).
3.2. Calculating Years of Life Losts
Using this formula, we calculated the number of years lost to early death (Equation 1):
When N is the number of deaths at a specific age and gender, L is the standard life expectancy at that age and gender. It refers to the maximum national life expectancy in 2000, and the difference between male and female life expectancy is assumed to be 2.5 years. Instead of using YLLs, the SEYLL is calculated by subtracting the age at death from the standardized life expectancy for the same age in the same gender in order to calculate the SEYLL.
The life expectancy tables in provide the standardized life expectancy of each case measured by age and gender, along with estimates of YLLs for each year.
GBD calculates the present value of lost years of life with a discount rate of 3%, so that for one year of living with health in early and terminal years of life, it considers a weight less than for a year in the middle years.
Through the following exponential function, one can demonstrate the weight of different ages (Equation 2):
In the Excel model of the World Health Organization for calculating YLLs, the values for β, C, and the discount rate were 0.04, 0.1658, and 0.03, respectively; these values were also used in this study (3).
4. Results
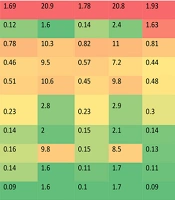
Figures 1 and 2 illustrate the transition of death rates two years before and two years during the COVID-19 outbreak for males and females, respectively. Compared to the crude MR, the YLL index provides a more accurate measurement of the burden of the problem. In 2018 - 2019 (prior to COVID-19 and the introduction of heightened investment sanctions), the total MR in men was approximately 5, but it sharply increased to nearly 7 in the two recent years (during the outbreak). A similar pattern was observed in women, albeit at a lower rate. Women's YLL was higher in the first year of the outbreak (2020), but in the second year, men's mortality occurred approximately 28 years sooner than expected, while women's mortality occurred 10 years sooner in the first year and 26 years sooner in the second year. Cardiovascular diseases (CVDs) caused the most lost years of life in men according to YLL scores in 2018 - 2019. Other significant causes included injuries, unintentional accidents, neoplasms (CA), prenatal mortality, diseases of the respiratory system (DRSs), endocrine, nutritional, and metabolic diseases, with parasitic and infectious diseases at the end of the table. In 2019 - 2020, CVDs, neoplasms, injuries, unintended accidents, prenatal mortality, and respiratory diseases contributed most to life lost, with infections and parasites rising to the 7th position. In 2020 - 2021, deaths were primarily attributed to CVDs, infectious diseases, parasitic diseases, COVID-19, injuries and accidents, prenatal mortality, neoplasms, and respiratory diseases. In 2021 - 2022, infectious and parasitic diseases, along with COVID-19, were responsible for the majority of the disease burden, followed by CVDs, injuries and unintended accidents, neoplasms, prenatal mortality, and diseases of the respiratory system (Figure 1).
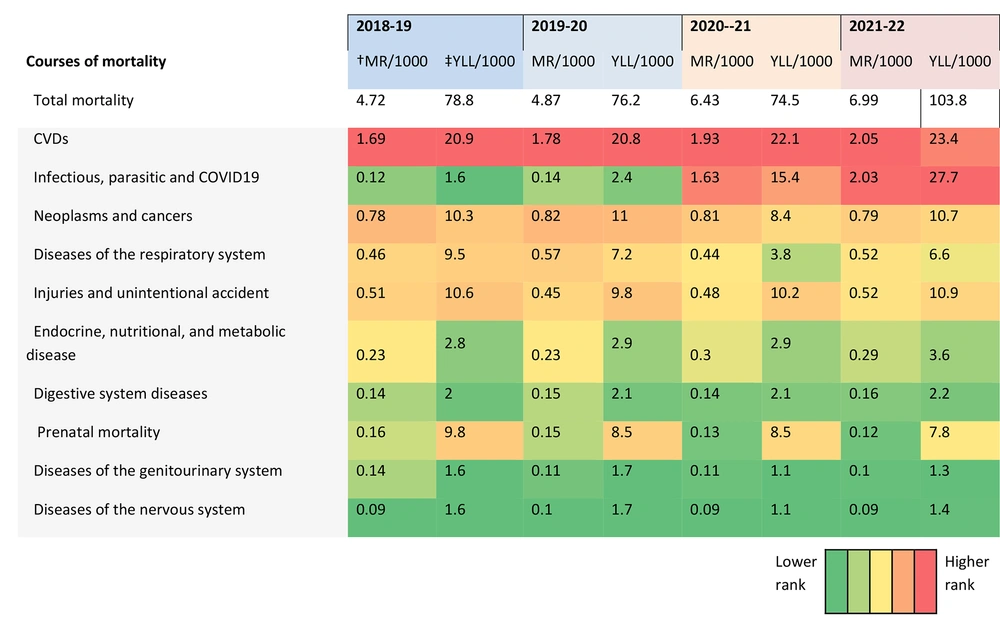
Figure 2 illustrates the transition in women's mortality over four years according to YLL. In 2018 - 2019, CVDs, neoplasms, prenatal deaths, respiratory diseases, injuries, and unintentional accidents accounted for the most deaths, with infections and parasites ranked ninth. In 2019 - 2020, CVDs, neoplasms, prenatal mortality, respiratory diseases, and endocrine, nutritional, and metabolic diseases accounted for the majority of life lost, with infections and parasites rising to seventh place. In 2020 - 2021, the burden of disease was primarily due to CVDs, infectious and parasitic diseases including COVID-19, neoplasms, prenatal deaths, and respiratory diseases. In 2021 - 2022, COVID-19, CVDs, neoplasms, prenatal deaths, and respiratory diseases were the leading causes of disease burden.
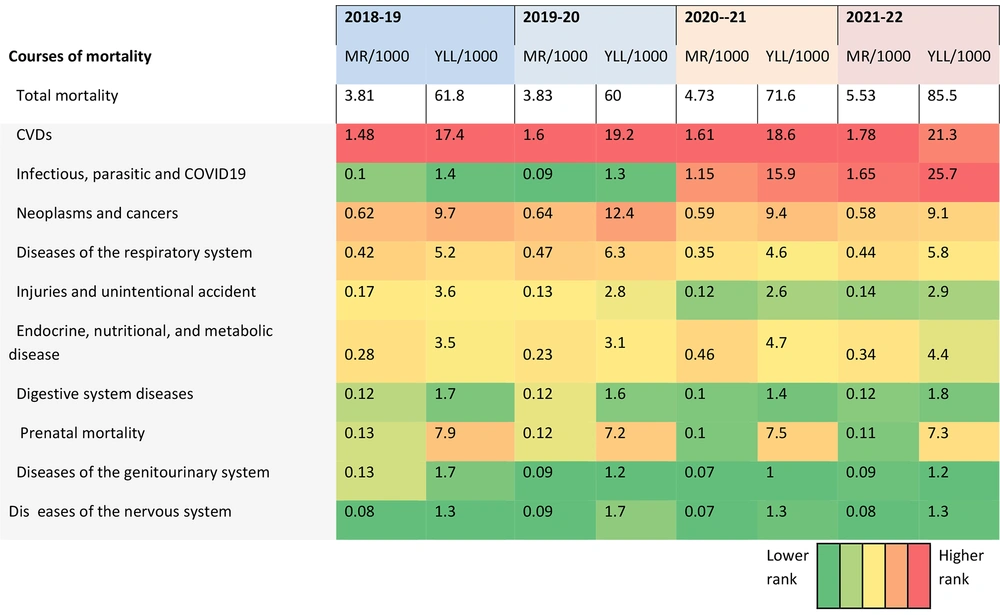
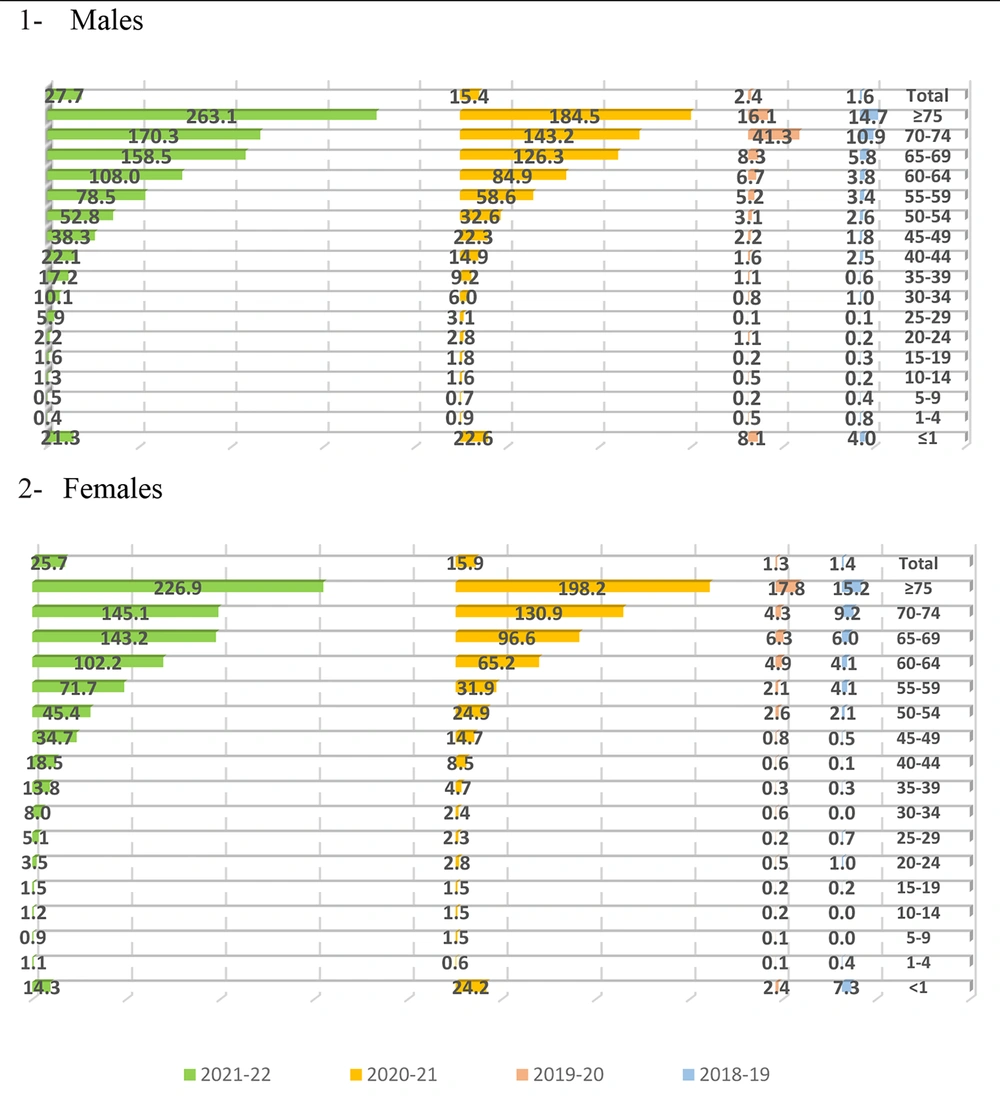
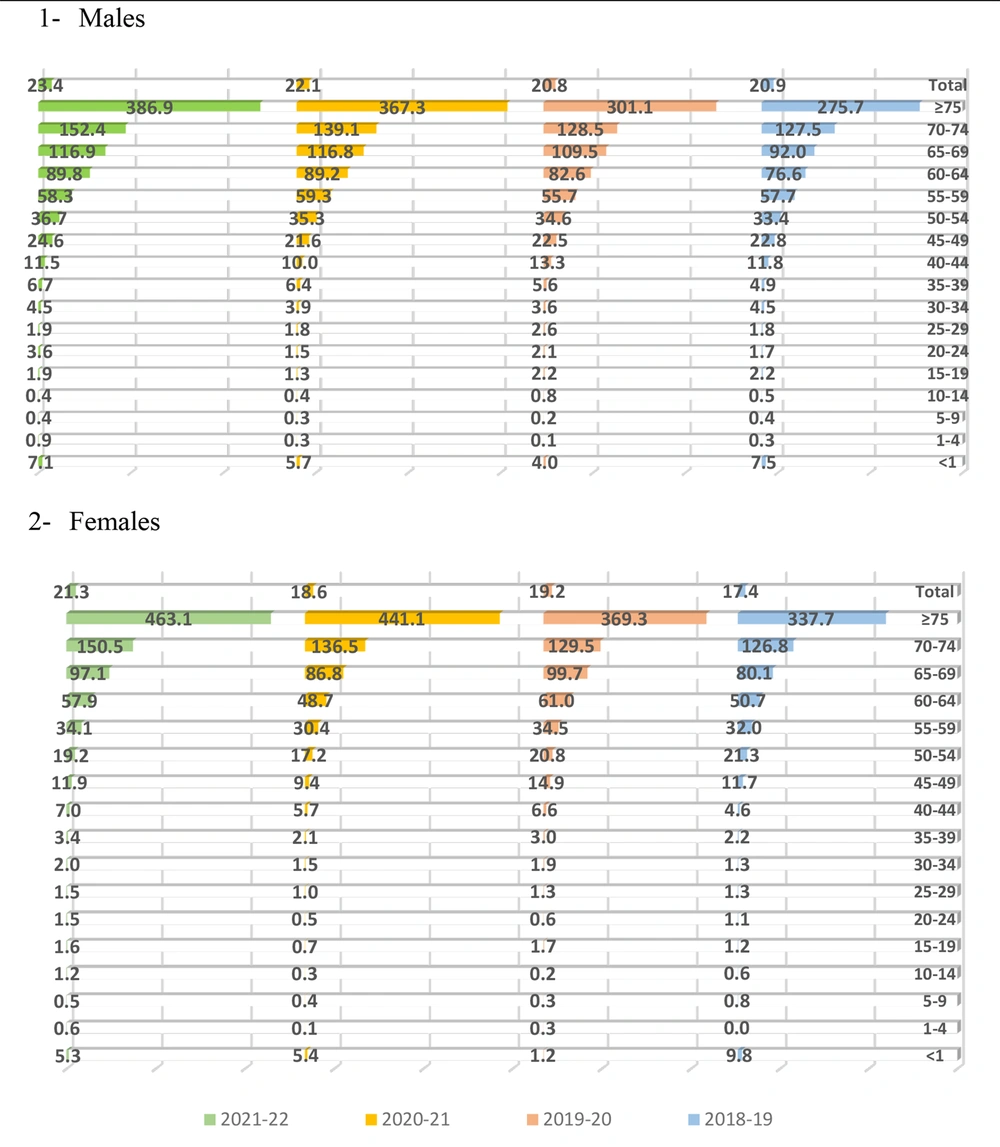
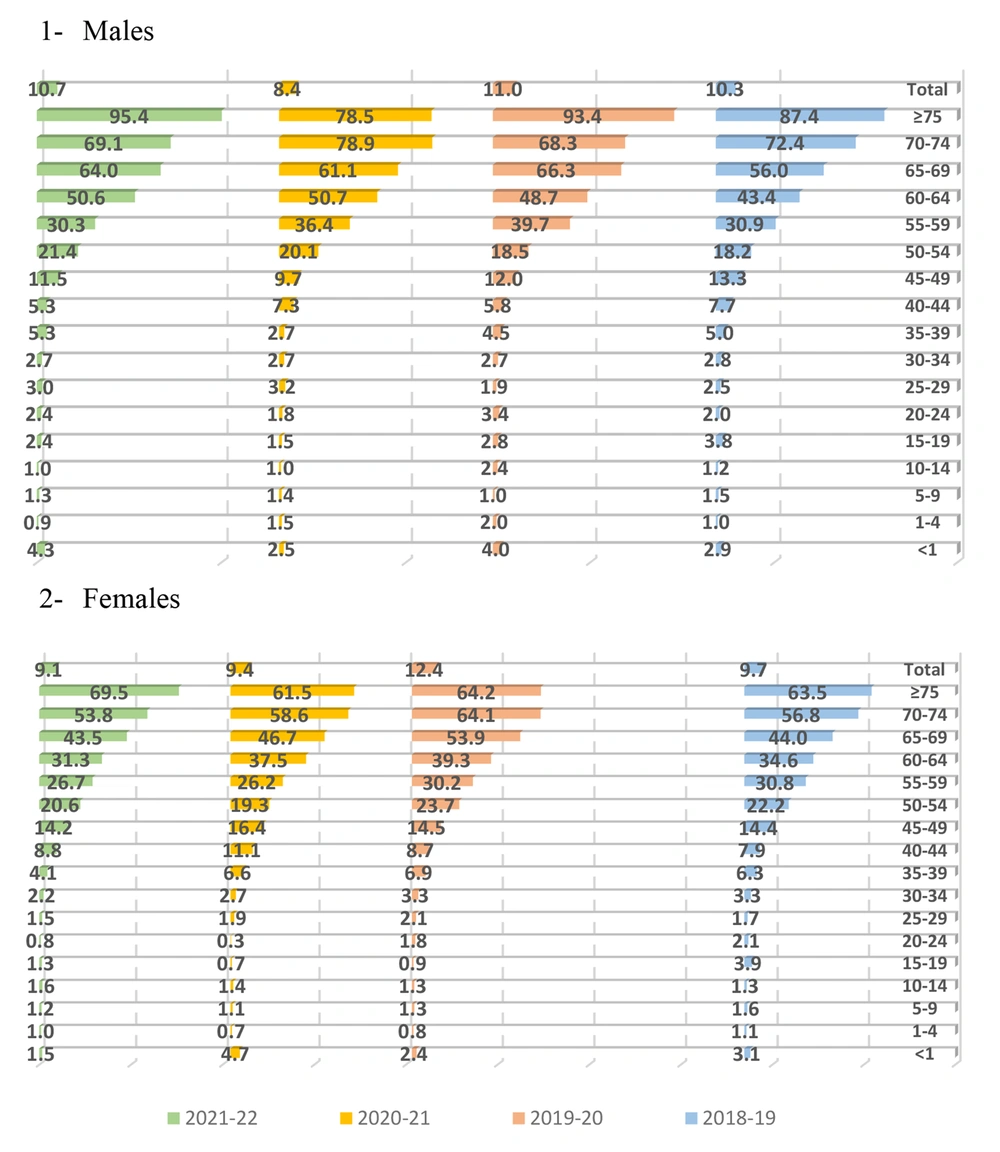
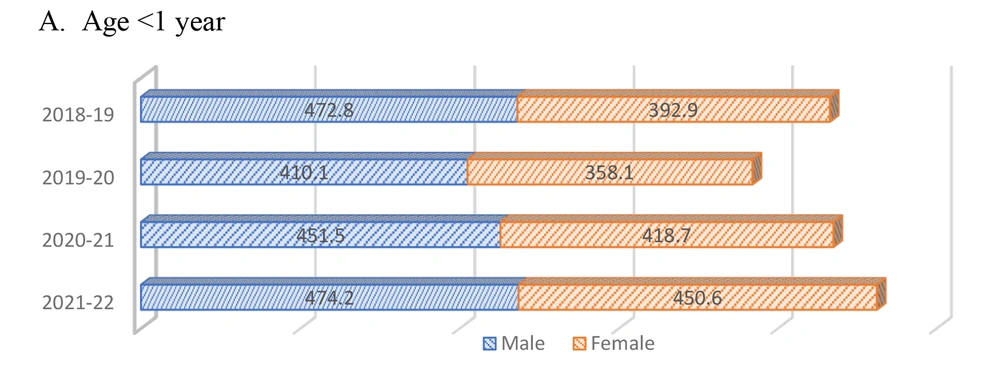
The number of YLL for men increased from 188,006 years in 2018 to 268,106 in 2022, and from 147,750 to 214,296 in women (Figure 3). Generally, older adults (≥ 75 years old) were more vulnerable two years ago, especially women. Men aged 30 - 60 and women aged 40 - 60 experienced increases in YLL. During the COVID-19 spread, infectious and parasitic diseases led to more lives lost among middle-aged and elderly individuals of both sexes. Since the COVID-19 outbreak, these diseases have become leading causes of death, particularly in middle-aged and elderly individuals (Figure 4). Men over 60 years of age are more likely to die from CVDs than women (Figure 5). Although cancers and neoplasms have consistently had a high YLL, infectious or parasitic diseases have recently played a greater role in early life loss, causing cancers and neoplasms to be ranked lower (Figure 6). Despite a reduction in overall prenatal mortality, it has increased in the under-one-year-old age group (Figure 7). Figure 8 shows that respiratory diseases maintained a regular pattern until the COVID-19 outbreak in 2020. During the first year of the outbreak, there was a significant reduction in respiratory disease deaths (YLL in 2021 = 3.8 compared to more than 5 in other years for men, and 4.6 in 2021 compared to more than 5 in other years for women), resulting in decreased mortality from these causes, with older women experiencing higher MRs.
5. Discussion
Policymakers and managers require a tangible way to express the burden of diseases and pathologies in society. Disability-adjusted life years (DALY) serve this purpose by quantitatively representing the disease burden through the calculation of years lost due to early death or disability. To calculate DALYs, the number of YLLs due to early death from disease is summed with the number of years lived with disability (YLDs) or diminished health (4). In this paper, YLDs and DALYs for causes of mortality during the COVID-19 outbreaks are not calculated due to the lack of firm data available to assess its long-term effects. However, histological, imaging, and epidemiological evidence from COVID-19 survivors suggests a significant future disease burden (5-7).
The COVID-19 pandemic has deeply affected all segments of society within just two years, straining healthcare systems worldwide due to mitigation strategies (1, 8). The determinants of health related to cancers (CA), CVDs, and DRSs remain consistent over short periods, except when major events disrupt social, economic, and environmental health determinants (9). COVID-19, being contagious and severe, places a heavy burden on the healthcare system's human and technical resources (1, 10). Most pre-hospital care, consultations, diagnostic services, general inpatient beds, and intensive care beds are reserved for COVID-19 patients (11). Factors such as population age distribution, failure to adhere to policy measures, and lack of healthcare system preparedness may have worsened the population's condition (8).
COVID-19 may increase YLL beyond expected levels, even beyond the direct burden of the disease, paralleling pandemic control. This may be due to a lack of clinical follow-up, screening, postponed surgeries, diagnostics, and hesitancy to seek healthcare. Although this study did not measure the direct effects of COVID-19 on disease burden, unexpected changes in YLL across age and gender subgroups indicated catastrophic effects. There is a tendency for acute diseases to affect older individuals, many of whom are disabled or have comorbid conditions, leading to rapid mortality. The results of this study should be interpreted cautiously. The YLL calculations were not age-adjusted, and due to data grouping, some analyses, such as confidence interval calculations, were not possible. Critical conditions may lead to incorrect cause of death records.
Accordingly, a rise in YLL could be linked to conditions that require high levels of care, but for which effective treatments remain elusive, potentially increasing health care costs. So, a healthcare system's ability to adapt and respond to COVID-19 and non-COVID-19 diseases determines the number of excess YLL.