1. Background
As a multidimensional concept, empathy consists of an individual’s ability to feel, understand, and perceive others’ emotional states (1). Scholars have addressed empathy as the drive to effectively respond to another individual’s psychological state (2, 3). In some cases, empathy is considered to play a substantial role in healthcare provision, leading to more efficient diagnosis and treatment measures and eventually enhanced patient satisfaction (4). Various fields of research have provided different connotations and definitions for the notion of empathy (5-7).
Psychosis indicates a separation from reality and is among the most controversial symptoms experienced by humans (8). Approximately 5% of individuals present with severe psychiatric disorders in every society (9). Understanding the condition of patients with psychiatric disorders is difficult for the families and caregivers of these patients (10, 11). Relationships with family in these patients can lead to satisfaction or, conversely, become a psychological burden (12-15).
A large body of literature aims to increase empathy to ultimately promote patient care; however, empathy has often been evaluated with researcher-made tools that lack well-determined psychometric properties, seriously challenging the comparison of intervention results (16-22). An obstacle in evaluating empathy among caregivers is the existence of various definitions for empathy in different healthcare settings (6, 23).
2. Objectives
Accordingly, the present study aimed to develop and validate a tool to measure caregivers’ empathy toward patients with psychotic disorders.
3. Methods
3.1. Study Design
The present study is methodological research that was carried out cross-sectionally. Initially, the tool was designed using the steps suggested by Waltz et al. (24). The first version of the tool, consisting of 120 items, was reviewed by the research team and 10 experts to ensure accuracy and eliminate any overlaps and repetitions. Eventually, the initial draft of the caregiver’s empathy for patients with psychotic disorders scale, consisting of 60 items, was developed.
3.2. Psychometric Analysis
3.2.1. Step 1: Qualitative and Quantitative Face Validity (Item Impact Method)
To determine the impact score of each item, 10 caregivers of patients with psychotic disorders were asked to assess the comprehensibility of each item. A five-item Likert scale was used (5 = completely comprehensible; 4 = comprehensible; 3 = slightly comprehensible; 2 = incomprehensible; 1 = completely incomprehensible). The item impact score was calculated using the following formula.
Frequency refers to the proportion of respondents who rated 4 or 5 on the Likert scale, and Comprehensibility is the average score for each item. Items that scored less than 1.5 were revised. For items that scored less than 1.5, caregivers were asked to explain the reasons for the items being incomprehensible in terms of at least three indicators: Difficulty level, appropriateness and ambiguity.
3.2.2. Step 2: Qualitative and Quantitative Content Validity
In the qualitative content validity (Qual-CV), the researcher requested 10 experts to review the tool based on Haynes’s criteria (25, 26). To evaluate the quantitative content validity (Quan-CV) of the scale, the content validity ratio (CVR) and Content Validity Index (CVI) were utilized. To determine CVR, 10 relevant experts were asked to evaluate each item using a three-point Likert scale. A score of “Essential” was considered acceptable. Scores were analyzed using the Lawshe formula, and items with a CVR score lower than 0.62, based on the Zareiyan and Lawshe table, were removed (27). To determine the item-CVI (I-CVI), 10 experts were asked to assess the relevance of each item using a four-point Likert scale. Items with a CVI score below 0.78 were removed (28).
3.2.3. Step 3: Construct Validity
Factor analysis was employed to assess construct validity. Factors were extracted using the principal component analysis (PCA) method. In this study, a factor loading of 0.32 was set as the minimum acceptable correlation threshold between each item and the extracted factors.
3.2.4. Step 4: Reliability
In this study, reliability was evaluated using two methods: Internal consistency (Cronbach’s alpha and McDonald’s omega) and stability (test-retest).
3.3. Population and Sampling Method
The population of this study consisted of the main caregivers of patients who experienced the onset of psychosis in the preceding ≥ 12 months and were referred to Razi Psychiatric Center in Tehran. Participants for the study were selected using the convenience sampling method.
3.4. Sample Size
In this study, given the criterion of the minimum ratio of subjects to variables as 10 to 1 according to the number of 21 items, at least 210 samples were required; however, to achieve the required reliability of the data, a sample size of 300 subjects was considered (29).
3.5. Inclusion Criteria
The inclusion criteria for the study included a definitive diagnosis of one of the most severe mental health disorders, necessitating care for the patient by a family member in the preceding 12 months. The age range for patients was 18 - 65 years, and for caregivers, it was 25 - 60 years. Caregivers were required to be actively living with the patient.
3.6. Ethical Considerations
The present study was approved by the Ethics Committee of the University of Rehabilitation and Social Health Sciences (IR.USWR.REC.1400.080) before the commencement of the study. All participants were informed about the study, and those who agreed to participate filled out the informed consent form.
4. Results
4.1. Face Validity
The qualitative assessment of the face validity of the scale led to the review and modification of 28 items that received scores below 1.5.
4.2. Content Validity
After calculating the CVR, 30 items from the initial version were removed, resulting in the development of the second version of the tool with 30 items. After calculating the Item Content Validity Index (I-CVI-K*), 5 items were removed. The Scale Content Validity Index/Average (S-CVI/Ave) score was 0.988, and the validity of the content of the general agreement of the tool (S-CVI/UA) was calculated as 0.80, which was categorized as excellent. After these modifications, a 25-item tool was prepared.
4.3. Item Analysis
In the item analysis phase, the Cronbach’s alpha coefficient for the total 25-item tool was found to be 0.823 among 32 participants. Given that the corrected total item correlation was below 0.3, 4 items were removed. Finally, the 21-item tool was considered for the construct validity assessment stage.
4.4. Construct Validity
In the present study, the factor analysis method was implemented to determine construct validity.
4.4.1. Demographic Characteristics
The demographic characteristics of participants are mentioned in Table 1.
| Characteristic | Construct Validity (N = 300) |
|---|---|
| Mean age | 41.43 ± 12.84 |
| Gender | |
| Male | 175 (58.3) |
| Female | 125 (41.7) |
| Educational status | |
| Under diploma | 136 (45.3) |
| Diploma | 100 (33.3) |
| Associate degree | 28 (9.3) |
| Bachelors | 26 (8.7) |
| Post graduate | 10 (3.3) |
a Values are expressed as mean ± SD or No. (%).
4.4.2.Factor Analysis
The KMO measurements and the results of Bartlett’s test of sphericity obtained from the implementation of the developed tool are presented in Table 2.
| Variables | Values |
|---|---|
| Kaiser-Meyer-Olkin measure of sampling adequacy | 0.838 |
| Bartlett’s Test of Sphericity | |
| Approx. chi-square | 1844.604 |
| df | 210 |
| P-value | < 0.001 |
Therefore, after performing PCA with Promax rotation according to Kaiser’s criterion, five factors were extracted. As shown in Table 3, the eigenvalues of the five factors are greater than one, and the percentage of variance explained by the five extracted factors is 55.86%.
| Factors | Eigenvalue | % of Variance | Cumulative % |
|---|---|---|---|
| Paying attention and caring for the patient | 5.533 | 26.346 | 26.346 |
| Lack of empathy | 2.113 | 10.063 | 36.410 |
| Empathetic identification | 1.785 | 8.502 | 44.911 |
| Sadness at the lack of empathy shown by others | 1.217 | 5.797 | 50.709 |
| Empathetic understanding of the patient’s delusions | 1.083 | 5.158 | 55.866 |
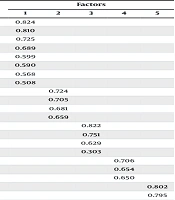
Therefore, it was determined that by extracting 5 factors and rotating the factors, all 21 items loaded significantly and purely on the 5 factors (Table 4).
| Items | Factors | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| In stressful situations I try to make her/him feel comfortable. | 0.824 | ||||
| I comfort her/him when she/he is under pressure and stress. | 0.810 | ||||
| I’m trying to find ways to connect with her/him. | 0.725 | ||||
| When I see someone abusing her/him, I try to protect her/him. | 0.689 | ||||
| Her/his feelings are really important to me. | 0.599 | ||||
| I enjoy helping her feel better. | 0.590 | ||||
| When she/he talks about her worries, I try to understand them. | 0.568 | ||||
| I would like to fully understand how she/he feels as a human | 0.508 | ||||
| I think she/he is deliberately harassing those around her/him. | 0.724 | ||||
| I get angry when she/he does not admit that she/he is sick. | 0.705 | ||||
| It is better for them to be isolated from society due to dangerous behaviors. | 0.681 | ||||
| I get angry at her/his irrational words. | 0.659 | ||||
| Before I make fun of her/his unusual words and behavior, I try to put myself in her/his shoes for a moment. | 0.822 | ||||
| I think she/he is having a hard life due to her/his illness. | 0.751 | ||||
| I try to put myself in her/his shoes to better understand her/his situation. | 0.629 | ||||
| I understand her when she/he is aggressive due to pessimism. | 0.303 | ||||
| I get upset when people avoid her/him because of her /his behavior. | 0.706 | ||||
| I get upset when she/he is worried and scared. | 0.654 | ||||
| I get upset if someone makes fun of her/his behavior. | 0.650 | ||||
| I can imagine someone who says she/his hears voices that others do not. | 0.802 | ||||
| I comfort her/him when she/he is under pressure and stress. | 0.795 | ||||
4.5. Reliability
After establishing the tool’s construct validity, the reliability coefficients were evaluated by the internal consistency and stability. The results are shown in Table 5.
| Factors | α | ω | ICC | 95% CI | P-Value |
|---|---|---|---|---|---|
| Paying attention and caring for the patient | 0.842 | 0.839 | 0.939 | 0.872 - 0.971 | < 0.001 |
| Lack of empathy | 0.651 | 0.638 | 0.865 | 0.671 - 0.940 | < 0.001 |
| Empathetic identification | 0.675 | 0.681 | 0.891 | 0.773 - 0.948 | < 0.001 |
| Sadness at the lack of empathy shown by others | 0.587 | 0.614 | 0.925 | 0.785 - 0.969 | < 0.001 |
| Empathetic understanding of the patient’s delusions | 0.595 | - | 0.799 | 0.584 - 0.904 | < 0.001 |
| Total | 0.804 | 0.795 | 0.951 | 0.876 - 0.978 | < 0.001 |
Abbreviations: α, Cronbach’s alpha coefficient; ω, McDonald omega; ICC, intraclass correlation coefficient.
The reliability coefficient of each subscale was calculated, indicating that all subscales have the desired reliability coefficient, based on Cronbach’s alpha coefficient, McDonald’s omega, and the intraclass correlation coefficient (ICC).
5. Discussion
Despite the significant importance of improving patient care, empathy is often assessed with researcher-made tools that lack sufficient validation. This issue emphasizes the need to design a valid tool with acceptable validity and reliability. Thus, the current study developed and assessed the psychometric properties of a tool to evaluate caregivers’ empathy toward patients with psychotic disorders.
Unlike the scale developed and assessed in this research, the Schwartz Center Compassionate Care Scale (30) and Fogarty’s Compassion Scale (1999) particularly address physicians (31). Healthcare professionals, including physicians and nurses, experience different perceptions of patients’ needs, attributed to their responsibilities (32), compared to non-expert caregivers, such as patients’ relatives. Given their different professional roles, physicians and nurses have different understandings of the needs of patients. Also, nursing care, which lasts longer, is of a different nature than medical care (33). Thus, the present study applied various methods to evaluate the psychometric properties of the designed tool.
Eliminating inappropriate items led to the approval of the content by the experts. According to DeVellis, the number of suitable items for the tool is less than 40 (34). Finally, five extracted factors explained more than 55% of the concept variance. The explained acceptable cumulative variance is 50%, per Hair et al. (35). According to the internal consistency coefficient (Cronbach’s alpha coefficient: 0.842, McDonald’s omega: 0.839), the reliability of this subscale was approved. Factor analysis data revealed that the items under factors have similar meanings and are correctly placed together. Factor 5 accounts for only two items. Although consistent with the establishment of developing and validating assessment tools, it is better to load at least three items per factor; however, sometimes, the theoretical foundations of a two-item factor are so strong that, accordingly, Robert Ho argued that in cases where the factor load is more than 0.7, that factor could be considered significant in both items (36).
Thus, the factor validity of the tool was confirmed due to the existence of an appropriate and logical factor solution.
5.1. Conclusions
The results of the present study indicate that the developed tool is accurate, valid, reliable, and culturally appropriate. Therefore, it can be effectively used to measure the extent of empathy in caregivers of patients with psychotic disorders. Furthermore, applying this scale facilitates the design of therapeutic interventions for this group of patients by emphasizing the influential role of caregivers’ empathy in improving quality of life, adherence to treatment, and recovery.