1. Background
Stroke refers to all abnormal functions of the central nervous system that occur as a result of a sudden disruption of the normal blood supply to a region of the brain due to a pathological process. It mainly occurs following the formation of a blood clot in the brain vessels, embolism following atrial fibrillation, or intracranial or subarachnoid hemorrhage. This disorder is often observed in patients in two main types: Ischemic (86%) and hemorrhagic (13%). Stroke is the second most common cause of death after ischemic heart disease, with approximately 5.6 million deaths annually. It is one of the leading causes of long-term disability worldwide and significantly affects the quality of life of affected individuals. In addition, the direct and indirect costs of treatment, lifelong care, and rehabilitation impose a huge financial burden on these patients and their families, with an estimated cost of $140 billion in the United States by 2030 (1-4). Although stroke mortality has decreased significantly in recent years, the situation in developing countries is still not favorable, and more than 80% of the total stroke mortality in the world occurs in developing countries (4).
In Iran, as in other developing countries, the incidence of stroke is high (between 23 and 103 per 100,000 population), with the difference that in our country, the occurrence of stroke almost a decade earlier (in terms of age) leads to disability and incapacity at younger ages and greater potential years of life lost, imposing a heavy socioeconomic burden on Iranian society. Although the extent and rate of growth of the infarcted area in ischemic stroke varies greatly from patient to patient, evidence suggests that the effectiveness of existing therapeutic strategies (including cerebral reperfusion and neuronal protection or repair) and long-term clinical outcomes in these patients are highly dependent on "time" (5, 6). In this regard, the most appropriate treatment introduced for reperfusion of the infarcted area in ischemic stroke is the use of intravenous recombinant tissue plasminogen activator (r-tPA), and the benefits of its timely injection (within the first 4.5 hours from the onset of symptoms to injection) have been well established (5-9).
Although in recent years, many clinical successes have been achieved in thrombolytic therapy in ischemic stroke management of patients eligible for IV r-tPA, and new guidelines have taken important and effective steps to facilitate the use of IV r-tPA by limiting contraindications and extending the time period for injecting this drug from 3 hours to 4.5 hours, evidence shows that many prehospital and hospital factors lead to delays in patients’ referral to the hospital after the onset of symptoms and prevent them from receiving IV r-tPA in a timely manner (10, 11). Less than 20% of eligible patients referred to emergency departments in developed countries are successful in receiving IV r-tPA within the designated time of 4.5 hours, and in less than a third of them, the recommended one-hour in-hospital "Door-to-Needle" time limit has been met.
Given that the time intervals between in-hospital events for the management of patients with ischemic stroke are always longer than the explicitly recommended time goals, healthcare providers and practitioners face great pressure to manage the obstacles ahead and plan for effective interventions aimed at improving the quality of care and clinical outcomes of these patients. To address this challenge, many hospitals have established multidisciplinary teams of clinical specialists (emergency medicine specialists, neurologists, nurses, etc.) and developed rapid response protocols called “stroke codes” to achieve the goals recommended by the American Heart Association and the American Stroke Association (12-14).
Similarly, in Iran, the stroke management emergency code (SAMA or 724) program in hospitals (neurology centers) was placed on the agenda of the Deputy Minister of Health of the Ministry of Health and Medical Education since 2015, and its implementation steps were subsequently communicated to all medical universities in the country. The program aimed to use an organized team approach to provide timely, safe, and effective care for patients with ischemic stroke. However, evidence indicates that there are gaps, differences, and discrepancies in the work, and adherence to the time goals of this program is problematic (15).
Therefore, by conducting systematic studies to continuously assess the operational capacity of emergency departments in stroke management and measure the time intervals of emergency health care services for patients with ischemic stroke, the necessary information can be provided to offer timely, accurate, and context-based feedback (patient, hospital, and treatment team members); identify areas in need of improvement; make appropriate decisions and actions; minimize unproductive trial and error methods to discover and correct deficiencies; and subsequently facilitate accountability (16, 17).
2. Objectives
Therefore, the present study aimed at comprehensively investigating the time performance of the Emergency Department of Imam Khomeini Educational and Medical Center, Urmia, Iran in relation to patients with ischemic stroke and the obstacles and problems in this field so that we can take a positive step in planning and improving processes in the field of operations management, education, and research.
3. Methods
This descriptive-analytical study was conducted using a cross-sectional method and census sampling on patients with an ischemic diagnosis referred to the Emergency Department of Imam Khomeini Hospital in Urmia in the first six months of 2022, which included 56 individuals. At the beginning of the study, a series of inclusion and exclusion criteria were established:
3.1. Inclusion Criteria
- Confirmation of the diagnosis of ischemic stroke by a neurologist.
- Exclusion of other causes (e.g., hemorrhagic strokes) using a CT scan of the head without contrast agent.
3.2. Exclusion Criteria
- Not finding the patient’s file
- File not being readable
- Incomplete files
- Distortion of the file
- Confirmation of the diagnosis of other types of hemorrhagic stroke by a neurosurgeon.
Information was collected using a checklist that included demographic information (age, gender, place of residence), disease-related characteristics (method of admission, triage level, month of referral, clinical symptoms, final patient outcome, and vital signs), and time characteristics (time of admission to the emergency department, time of first visit by the emergency medicine service, time of CT scan, etc.). After collection, the data were entered into SPSS18 and analyzed using descriptive statistics (frequency, percentage, mean, and standard deviation).
4. Results
A total of 56 individuals participated in this study, with the majority being female (64.3%). Most participants resided in the city (71.4%), and a significant portion were referred from the outpatient emergency department (60.7%). The majority were classified as triage level two (76.8%). The month of referral was predominantly October (21.4%). The average age of the patients was 71.46 ± 12.52 years (Table 1).
| Variables and Subgroups | No. (%) |
|---|---|
| Gender | |
| Man | 20 (35.7) |
| Woman | 36 (64.3) |
| Residence | |
| City | 40 (71.4) |
| Rural | 16 (28.6) |
| How to go to the emergency room | |
| Outpatient | 34 (60.7) |
| Dispatch | 10 (17.9) |
| Ambulance | 12 (21.4) |
| Triage level | |
| One | 13 (23.2) |
| Two | 43 (76.8) |
| Month of referral | |
| October | 12 (21.4) |
| November | 12 (21.4) |
| December | 9 (16.1) |
| January | 12 (21.4) |
| February | 6 (10.7) |
| March | 5 (8.9) |
| Age (mean ± SD) | 71.46 ± 12.52 |
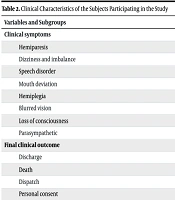
Most of the patients referred had hemiparesis symptoms 16 (28.6%), the final outcome was discharge 48 (85.7%) (Table 2).
| Variables and Subgroups | No. (%) |
|---|---|
| Clinical symptoms | |
| Hemiparesis | 16 (28.6) |
| Dizziness and imbalance | 11 (19.6) |
| Speech disorder | 10 (17.9) |
| Mouth deviation | 3 (5.4) |
| Hemiplegia | 4 (7.1) |
| Blurred vision | 1 (1.8) |
| Loss of consciousness | 7 (12.5) |
| Parasympathetic | 4 (7.1) |
| Final clinical outcome | |
| Discharge | 48 (85.7) |
| Death | 5 (8.9) |
| Dispatch | 1 (1.8) |
| Personal consent | 2 (3.6) |
The mean systolic blood pressure was 161.82 mmHg, the mean diastolic blood pressure was 97.82 mmHg, the mean heart rate was 85.07 beats per minute, and the mean oxygen saturation was 93.51% (Table 3).
| Variables | Mean ± SD | Range |
|---|---|---|
| Systolic blood pressure | 161.82 ± 35.56 | 93 - 240 |
| Diastolic blood pressure | 97.82 ± 35.56 | 58 - 140 |
| Heart rate | 85.07 ± 14.16 | 62 - 128 |
| Oxygen saturation percentage | 93.51 ± 6.6 | 50 - 100 |
According to Table 4, the average time interval from patient entry to triage to case formation was 6.78 minutes. The shortest interval was 1 minute, while the longest was 0.40 minutes. The average time from case formation to an emergency medicine specialist visit was 17.33 minutes, with the shortest interval being 1 minute and the longest 0.80 minutes. The average interval from triage entry to an emergency medicine specialist visit was 23.83 minutes, with the shortest being 2 minutes and the longest 0.83 minutes. The average time from triage entry to a neurologist visit was 116.55 minutes, with the shortest interval being 2 minutes and the longest 0.800 minutes. The average interval from an emergency medicine specialist visit to a neurologist visit was 0.90 minutes, with the shortest being 1 minute and the longest 0.460 minutes. The mean time from an emergency medicine specialist visit to a CT scan was 62.26 minutes, with the shortest interval being 25 minutes and the longest 480.0 minutes. Four patients were prescribed r-tPA, with the mean time from patient arrival to r-tPA injection being 47.5 ± 5.6 minutes.
| Variables | Mean ± SD | Range |
|---|---|---|
| Time interval from entering triage to filing | 6.78 ± 6.96 | 1 - 4 |
| Time interval from filing to emergency medicine specialist visit | 17.33 ± 7.94 | 1 - 80 |
| Time interval from entering triage to emergency medicine specialist visit | 23.83 ± 19.15 | 2 - 83 |
| Time interval from entering triage to neurologist visit | 116.55 ± 128.02 | 2 - 83 |
| Time interval from emergency medicine specialist visit to neurologist visit | 90 ± 9.7 | 1 - 460.40 |
| Time interval from emergency medicine specialist visit to CT scan | 62.26 ± 7.13 | 25 - 480 |
| Time interval from entering emergency medicine specialist visit to CT scan | 86.05 ± 15 | 30 - 600 |
5. Discussion
Among the neurological diseases that occur throughout human life, stroke clearly ranks first in frequency. Stroke accounts for at least half of the neurological disorders in a general hospital. Prompt and timely treatment after stroke onset and avoiding further delay, especially more than 3 hours in ischemic stroke patients, and blood pressure control in patients with hemorrhagic stroke are very valuable. Although the use of rtPA and recombinant factor 7 is very beneficial, these patients do not use these treatments frequently due to the delay in hospital discharge. Of the 7.5 million stroke patients who died in 2005, 87% were from countries with low to moderate healthcare, of which Iran is classified as a middle-income country according to the World Bank classification, and recent reports indicate a higher prevalence of stroke in Iran compared to western countries (18, 19).
The present study was designed and implemented to determine the time status of providing emergency services to patients with acute ischemic stroke who referred to the Emergency Department of Imam Khomeini Educational and Medical Center in Urmia in the second half of the year 2022. In the present study, the mean age of the patients was 71.46 ± 12.52 years, with 64.3% being female and 35.7% male. In the study by Ghiathian et al. (18), which aimed to investigate the factors affecting the delay in hospital admission after acute stroke, the mean age of the patients was 70.12 years, which is close to the mean age of our study. However, in the study by Ghiathian et al. (18), contrary to the results of our study, a higher percentage of the patients were male. In the study by Mirzadeh et al. (20), which aimed to investigate the causes and barriers to non-receipt of tPA, the mean age of the patients was 65.92 years, which is slightly lower than the mean age of the patients in our study. In the study by Hatamabadi et al. (21), consistent with the results of our study, a higher percentage of patients were women.
In the present study, 71.4% of patients were urban residents and 28.6% were rural residents. In the study by Ghiasian et al., nearly 75% were urban residents and 25% were rural residents, which is a frequency close to our study (18). In the present study, 60.7% were outpatients, 17.9% were referred from other medical centers, and 21.4% were referred to the emergency department by ambulance. In the study by Siddiqui et al. (2008), in terms of mode of transportation, only 46 (27.9%) of the patients were referred by ambulance, while 119 (72%) were referred by public or private car (22). In this study, similar to the results of our study, a small percentage of patients were referred by ambulance. Also, in the study by Koksal et al., 63.7% of patients were referred to the hospital by private vehicle and 36.03% by ambulance (23), which is a higher percentage of patients referred by ambulance than in our study.
The most common clinical symptoms of patients referred to the emergency department were hemiparesis, dizziness and imbalance, speech disorder, and loss of consciousness, respectively. In the study by Ghiasian et al. (18), the most common symptoms that patients with cerebral palsy had were right-sided focal motor deficits with a frequency of 22.6%, followed by multiple concurrent neurological symptoms with a frequency of 20%, and in third place were patients with left-sided focal motor deficits with a frequency of 16%. In the study by Mirzadeh et al. (20), the most common clinical symptoms of patients were hemiplegia and hemiparesis. In the study by Daneshfard et al. (24), the most common clinical symptom was hemiparesis.
In the present study, the average time interval from patient entry to triage to file creation was 6.78 minutes, the average time interval from file creation to emergency medicine specialist visit was 17.33 minutes, the average time interval from triage to emergency medicine specialist visit was 23.83 minutes, the average time interval from triage to neurologist visit was 116.55 minutes, the average time interval from emergency medicine specialist visit to neurologist visit was 90.0 minutes, and the average time interval from emergency medicine specialist visit to CT was 62.26 minutes. Four patients were prescribed r-tPA. The average time interval from patient entry to r-tPA injection was 47.5 ± 5.6 minutes. In the study by Mirzadeh et al. (20), which was conducted to investigate the causes and barriers to not receiving tPA, the average time interval from the patient’s arrival at the emergency room to the visit to the neurologist was 432 minutes, which is a longer average than in our study. Also, in the study by Mirzadeh et al. (20), the average time interval from the patient’s arrival at the emergency room to the CT scan was 45 minutes, which is a shorter time interval than in our study. Also, in this study, the average time interval from the patient’s arrival at the emergency room to receiving tPA was 176 minutes.
It should be noted that the appropriate and recommended time for performing CT scanning in patients with suspected acute stroke according to ASA/AHA is 20 minutes, but in our study, CT scanning was delayed by an average of 40 minutes. Also, in the study by Ayromlou et al. (25), the average time interval from the patient’s arrival at the emergency room to the CT scan was 91 minutes, and in the study by Hatamabadi et al. (21), the average time interval from the patient’s arrival at the emergency room to the CT scan was 89 minutes, which is a higher average than in our study and reflects the fact that the average time interval from the patient’s arrival at the emergency room to the CT scan in our study was more favorable. In the study by Hatamabadi et al. (21), the average time interval between the patient’s arrival at the emergency room and the visit to the neurologist was 100 minutes, which is a higher average than in our study and indicates that the patients in our study were visited by a neurologist in a shorter time interval.
One of the strengths of this study is the lack of such a study at the provincial and city levels, as well as on an important issue such as treating stroke patients, which is vital and important. One of the weaknesses of this study was the incompleteness and emptiness of some files, which were excluded from the study. It is suggested that these studies be conducted on other diseases such as heart patients, surgery, etc., and that these studies be conducted periodically to improve the conditions.
5.1. Conclusions
According to the results of the study, it is essential to develop a plan to identify the influential factors and implement appropriate actions for the faster treatment of these patients. Delays in prompt treatment can lead to adverse consequences or even death.