1. Background
Dermatomycosis or fungal infection of skin and its appendages has different classifications but in this study, we consider only superficial type (tineaversicolor) and cutaneous one (dermatophytosis). Superficial type of the infection is limited to the outermost layer of skin and hair. The most important example is tineaversicolor, which is a fungal infection that commonly affects the skin of the young people, especially at the chest, back, upper arms and legs, excluding the face. This fungus produces spots that are either lighter than the skin or reddish-brown (1-3).
Cutaneous mycosis or dermatophytosis is a common disorder worldwide which can affect the skin and hair deeper into the epidermis. These infections lead to a variety of clinical manifestations, including tinea capitis (scalp), tine apedis (feet), tinea cruris (groin) and tinea corporis (other body areas) (4, 5).
In related studies,tineapedis (Athlete's foot) is the most common superficial fungal infection in adults and tinea capitis almost always occurs in children. Based on the literature, only three types of dermatophytes cause the majority of infections: Epidermophyton, Trichophyton and Microsporum (6-9). It is to be noted that in this study we use the broad title of superficial fungal infections (SFIs) for both superficial type and cutaneous one.
The prevalence and characteristics of SFIs directly relate to some important factors such as climate, hygiene, life style, etc. In military centers, The pattern of SFIs, as well as other cutaneous diseases, is quite different because of the presence of predisposing and precipitating factors, as well as other cutaneous diseases.
These factors consist of fewer bathrooms, poor hygiene, marching practice, wearing shower sandals, frequent use of ‘gummed’ shoes, recurrent trauma to the nails and hyperhidrosis during military maneuvers among young soldiers, particularly those with low literacy (9-11).
The burden of cutaneous diseases in US military force is about 3 million person-days, which is a shocking number in any military system (12). It is to be noticed that SFIs can be a health indicator of the community and represent its socioeconomic condition (13).
In the previous studies in Iran, SFIs prevalence was reported between 3-6% and almost always, tinea versicolor and tinea pedis have been the major causes (9, 11-15). Unfortunately, among Iran Army personnel, SFIs pose an important health problem that has been poorly controlled so far. Due to the lack of any comprehensive study in Iran Army to compare the prevalence between different situations, this study was designed to evaluate the epidemiologic profile of SFIs in Iran Army personnel.
2. Objectives
The main objective of this retrospective study was to assess the epidemiologic features of superficial fungal infections (SFIs) in Iran Army personnel from 2005 to 2011. We should emphasize that reporting SFIs is mandatory in the surveillance system of Iran Army, so data were gathered from archived records in the Department of Preventive Medicine, Deputy of Health, AJA University of Medical Sciences in Tehran.
3. Patients and Methods
Our inclusion criterion was any military person with confirmed diagnosis of SFI. Diagnosis of most cases had been confirmed by physicians and in controversial cases by potassium hydroxide (KOH) preparation test. At the end of each season we would be able to calculate the cumulative incidence rate of SFIs in different provinces, and in Triple Armed Forces based on the population of each center. Data analysis was based on t-test and analysis of variance (ANOVA) for quantitative variables and chi-square test for qualitative ones, which was carried out by the 11th version of Stata software.
4. Results
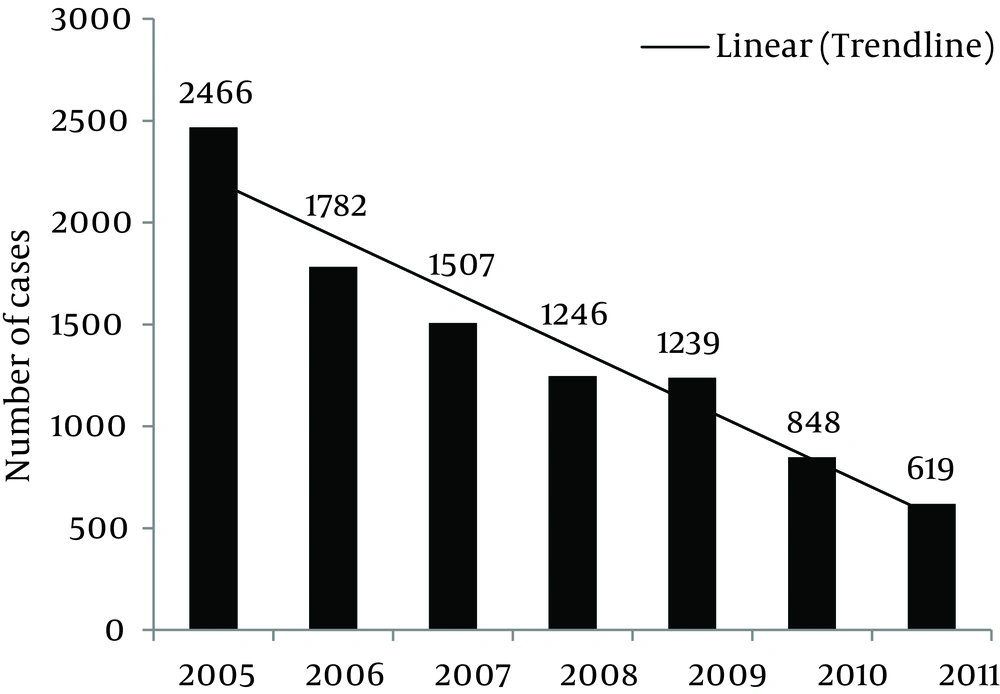
In this 7-year study (2005-2011), a total number of 9707 cases of SFIs were reported from 25 provinces. This distribution is illustrated in Figure 1. Given that the denominator of the incidence rate (total population) has been remained relatively fixed during these years, we can conclude that the prevalence has been decreased from 2005 to 2011 (linear trend-line in Figure 1).
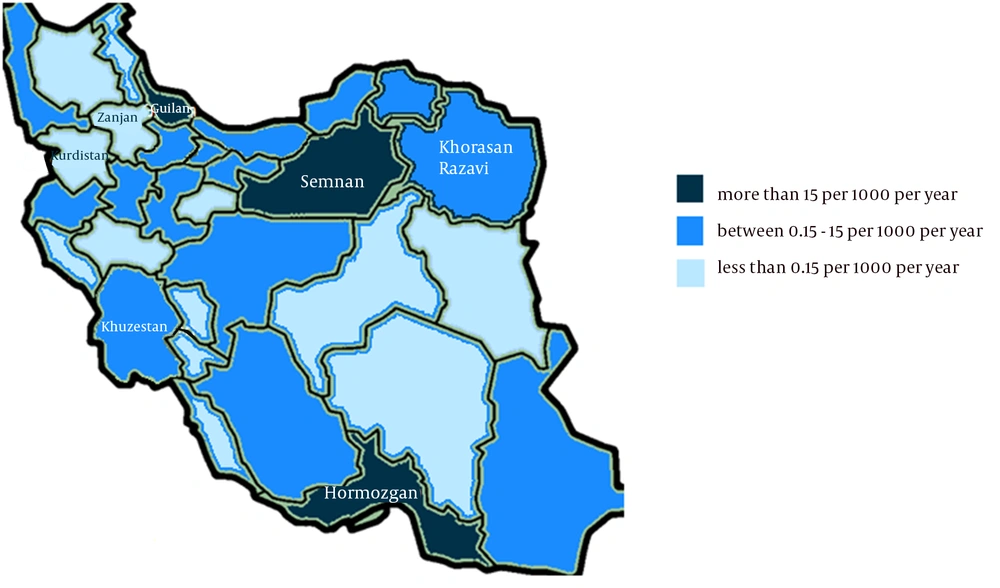
Figure 2 illustrates the geographical distribution of SFIs in different provinces. Major difference in incidence exists between the provinces, from more than 15 persons in 1000 (per year) in humid ones such as Guilan and Hormozgan to less than 0.15 persons in 1000 in some cold and mountainous ones such as Kurdistan and Zanjan.
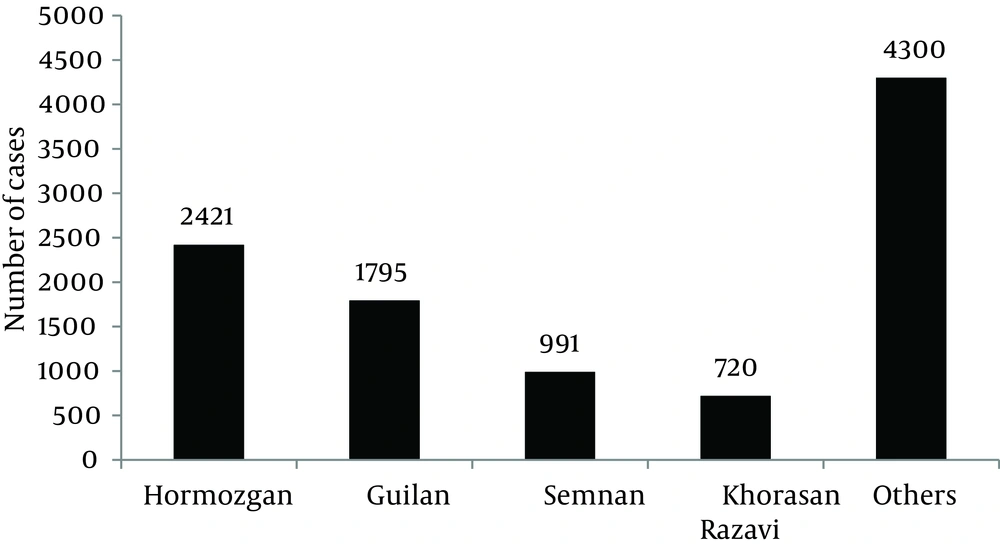
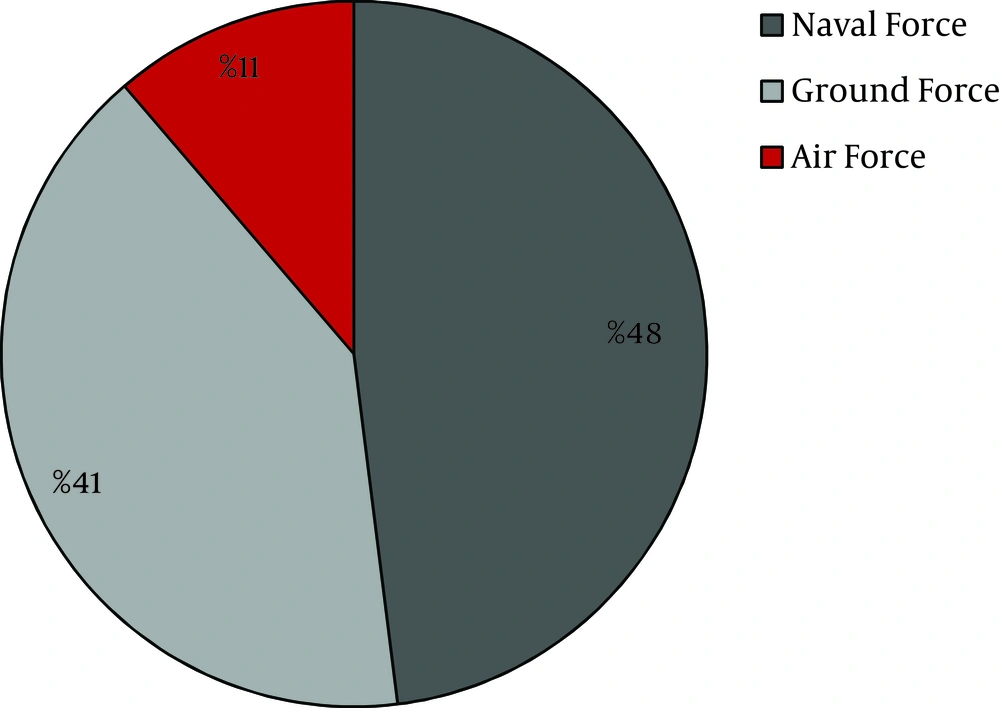
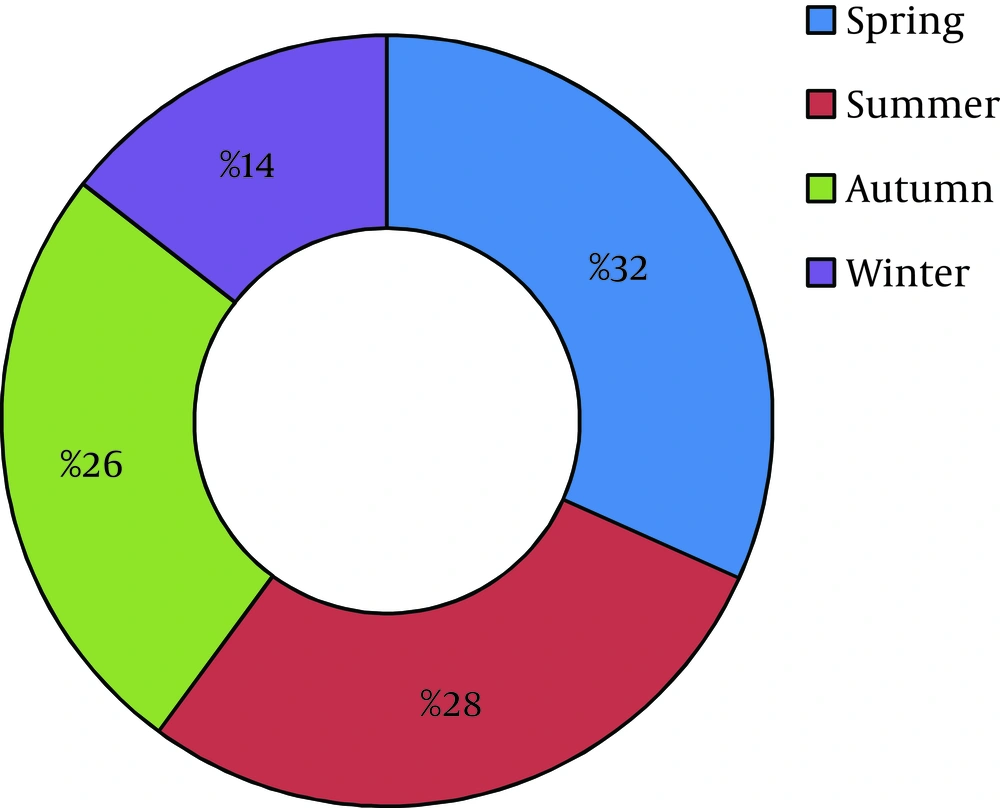
Around 58% of cases were reported from four provinces, including Hormozgan (24.9%), Guilan (18.5%), Semnan (10.2%), and Khorasan Razavi (7.4%) (Figure 3). Distribution of SFIs in Triple Armed Forces is shown in Figure 4. About half of the patients (4606 cases; 48%) were reported from Naval Force, yet its population is only 14% of total Army. Therefore, the incidence rate in this force is at least 5 times greater than the other forces, and it should be mentioned that this difference is statistically significant (P value < 0.001). Maximum incidence rate was in summer and spring (32% and 28% respectively), and only 14% of cases occurred in winter (Figure 5). The relationship between season and cumulative incidence rate was also significant (P value < 0.001).
5. Discussion
In this study, the calculated periodic prevalence was 2.1%, which is a little less than previous studies on military populations (3-6%) (10-17). Nevertheless; this calculation is not accurate enough since as Ingordo and Pau stated "something more than two-thirds of patients do not know their disease, have no complaint and will be missed. "Hence, we should add another 66% to our reported cases that increase our estimated real prevalence to more than 6% (a shocking number in any military system) (17, 18).
Among the provinces in this study, Hormozgan, Guilan and Semnan had the highest infection rate, and the least incidence rate belonged to Kurdistan and Zanjan. As we mentioned before, this difference could be due to various weather conditions (warm and humid in Northern and Southern provinces against cold and mountainous in Western ones) which is the most important risk factor for SFIs.
We also found that about half of the cases (48%) were members of Naval Force and it may be due to their services at the humidity of naval centers near sea side. This finding is clearly contrary to Ingordo's study, which claimed the incidence rate in Italian sailors not to be more than general population. This discrepancy can be explained by the fact that Italy is located near the Mediterranean Sea and has a warm and humid climate all over the country; so there will be no difference between SFI prevalence in its various areas (17).
As we mentioned earlier about seasonal distribution, the majority of cases (60%) had occurred during spring and summer similar to Welsh study, which claimed to observe most of the cases in the warmest months of the year from March to September (19).
Finally, it is important to say that overall trend of SFIs in Iran Army has been decreasing during recent years. This can be due to taking proper preventive measures in the military centers and paying more attention to health issues by army commanders. But the prevalence is still high enough considered as a major problem, especially in Naval Force and in the warm and humid provinces. We recommend reporting these results to the army health commanders for better planning, increasing health knowledge, improving personnel hygiene, and providing health facilities in different provinces to decrease the incidence of these easily preventable infections.