1. Background
The human masticatory system is an extremely complicated mechanism consisting of jaw basal bone, ligaments, muscles and teeth. It is widely accepted that the etiology of temporomandibular joint disorders (TMDs) is multifactorial and commonly related to a number of dental, medical and mental conditions; such as occlusion, posture, parafunctional habits, restorations, orthodontic treatment, emotional stress, trauma, anatomy of the disk, pathophysiology of the muscles, genetic and psychosocial factors (especially stress), age, and gender (1, 2). Typical signs and symptoms of TMD are pain (in masticatory muscles or in TM joint itself), joint sounds, limitation in mouth opening, bruxism, mandibular deviation and chewing disability. The mentioned symptoms may exist alone or in combination (2). It has been reported that 5%-12% of the general population have TMDs (3).
Parafunctional habits such as bruxism, teeth clenching, gum chewing, biting foreign objects, and prolonged nail biting might increase the risk of developing TMD (4, 5). Dental attrition is considered as a visible sign of physiological functional wear and a rather rapid onset in bruxism. It has been reported that bruxism may cause hypermobility of the masticatory muscles, leading to TMD (6). The mechanism is mainly attributed to the damage of the muscle fibers (7) and sometimes to the reduction of the muscle blood supply (8).
The association between TMD and psychosocial factors (e.g. stress) has also been widely reported. Numerous studies suggest that psychosocial factors, including stress, depression and anxiety, play some role in the predisposition, initiation, and progression of TMD and in the responses of TMD patients to treatment (9, 10). Sugisaki et al. (11) reported that the prevalence of TMD-related symptoms was higher (approximately 17%-18%) among the working population than the general population (5%-12%). They concluded that this difference was attributable to psychological aggravation resulting from duties in the workplace, changes in the work environment, interpersonal relations, and an achievement oriented climate.
2. Objectives
These conditions are frequently seen in the life of army personnel. Since there has been neither a report on the prevalence of TMD among army personnel of Iran and other countries, nor a comparison to the civilians, this study was planned to address the demand.
3. Patients and Methods
For this prospective study, we enrolled 400 patients seeking general dental treatment at Shahid Fallahi Dental Clinic and Be'sat Hospital between December 2013 and February 2014. Both centers are military based clinics. Out of the participants, 200 were army personnel (case group), and the rest were the civilians (control group). Patients with the following criteria were excluded from the study: having severe skeletal deformities, reverse overjet, and an edge to edge anterior occlusion.
We tried hard to match the control group with the case group, particularly with respect to age and gender. Since the above-mentioned clinics were both military ones, the majority of the male patients belonged to the army group. To match the groups, we mostly chose the wives of the included patients, because we believed that they best assimilate the case group with respect to the stress they suffered.
Data were collected by filling a checklist. The following criteria were included in the checklist: sex, age, army personnel, presence in the war, dental attrition, TMJ click on opening or closing the mouth, limitation in mouth opening, and pain or tenderness of TMJ or masticatory muscles on palpation. To avoid intra-examiner errors, all examinations were done by a single practitioner. Dental attrition was approved by observing attrition more than 1 mm on more than 2 teeth. Mouth opening was measured by a gauge. Limitation on mouth opening was approved if the patient could not open his or her mouth more than 3 mm. All statistical analyses were performed using the SPSS statistical software package, version 16.0 (SPSS Inc., Chicago, IL, USA). First of all, normal distribution of the data was approved by Kolmogorov-Smirnov test. Then chi-square test and Fischer exact test were used to evaluate the correlation between the variables. A P value < 0.05 considered statistically significant.
4. Results
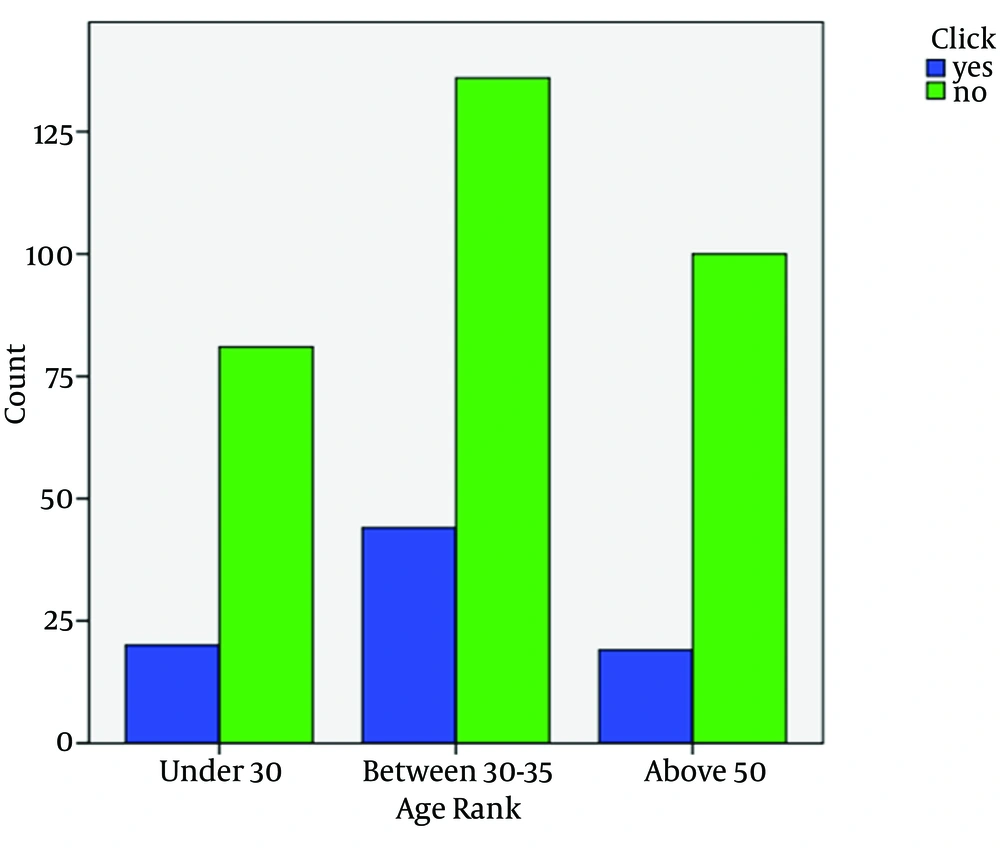
A total of 400 patients (222 males [55.5%] and 178 females [44.5%]) were enrolled in the study. The participants were divided into three age groups: under 30, 30 to 50, and more than 50 years old. Figure 1 shows the distribution and proportion of the army group in comparison to the control group. As seen in Figure 1, most of the participants in both groups were between 30 and 50 years old. Among the army group, 106 (53%) persons were participated in the war; most of them aged more than 50.
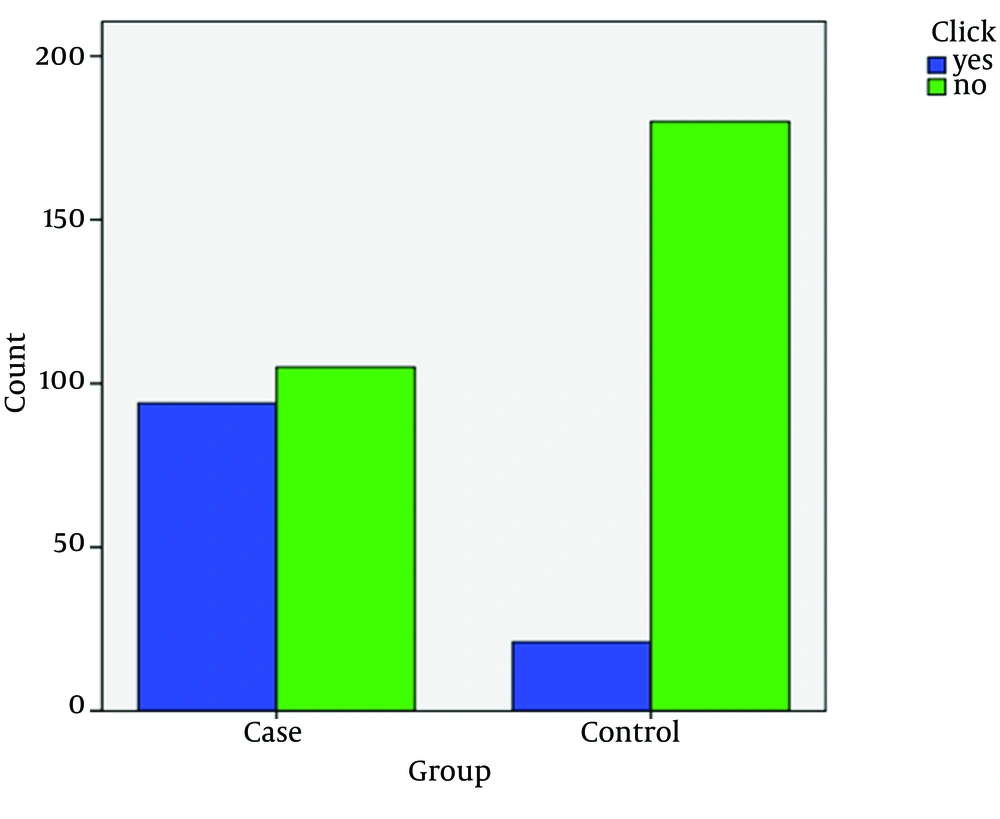
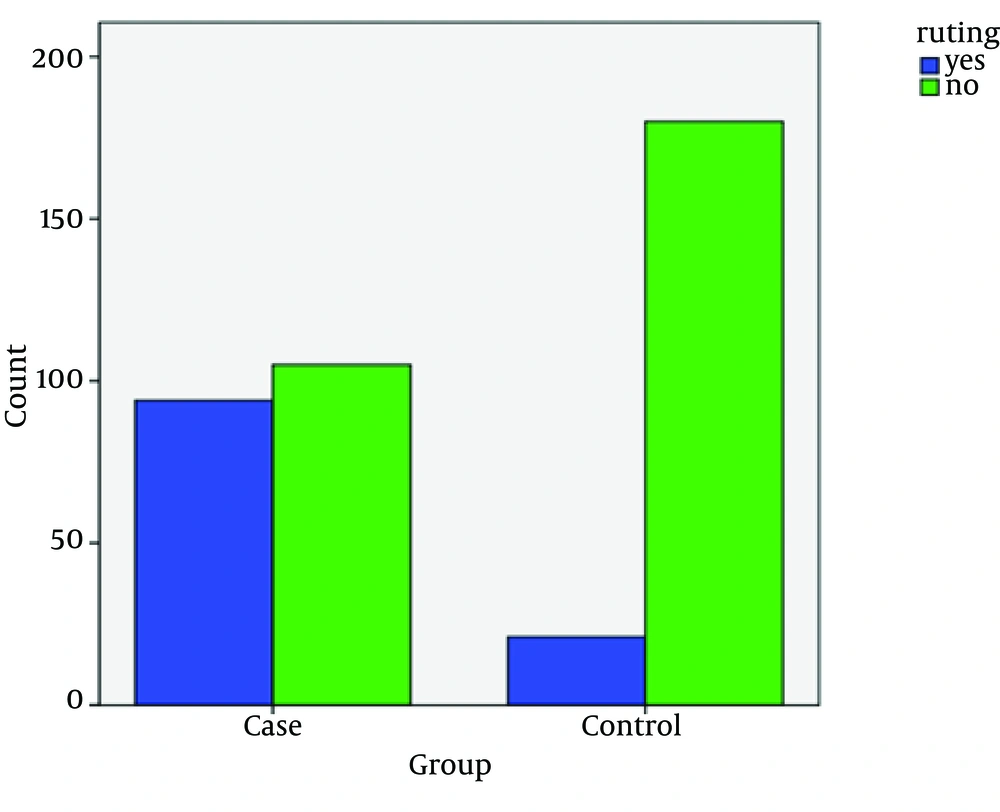
The prevalence of dental attrition was 9.9% in the patients under 30, 17.7% in the patients between 30 and 50 and 61% in the patients more than 50 (Figure 2). The differences between the age groups were statistically significant (P value = 0.001). Figure 3 shows dental attrition prevalence in army and civilian groups. The army group had statistically more significant dental attrition than the control group (P value = 0.001). Considering the army group, we observed statistically more significant dental attritions in those who have participated at war (P value < 0.05).
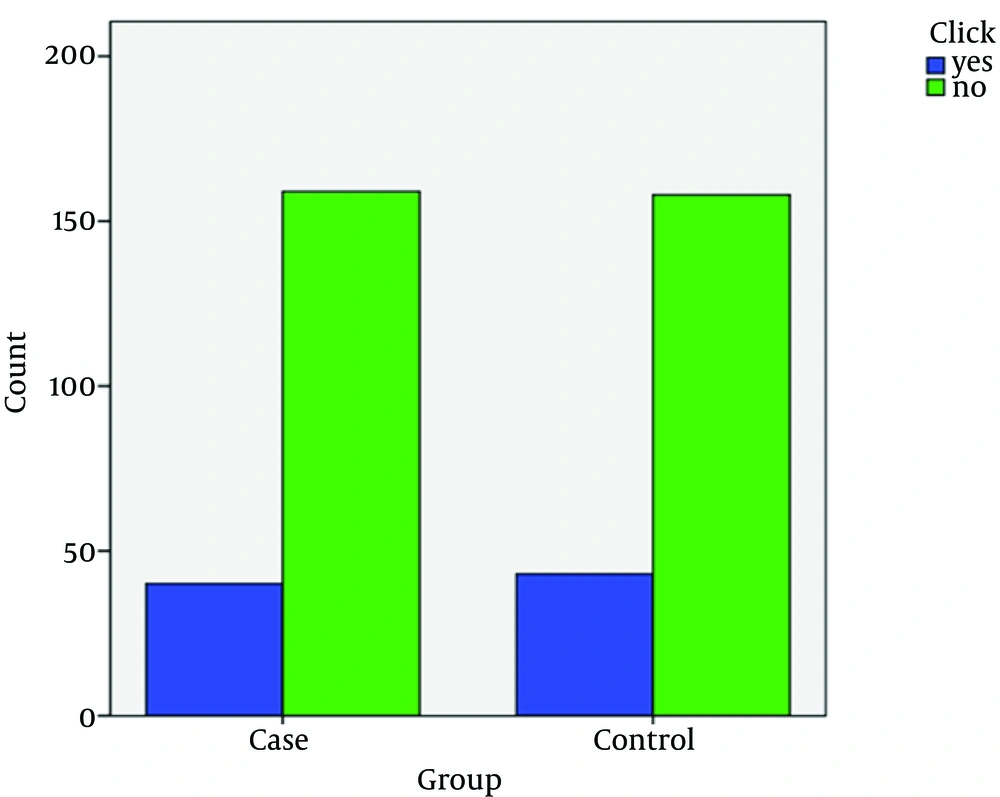
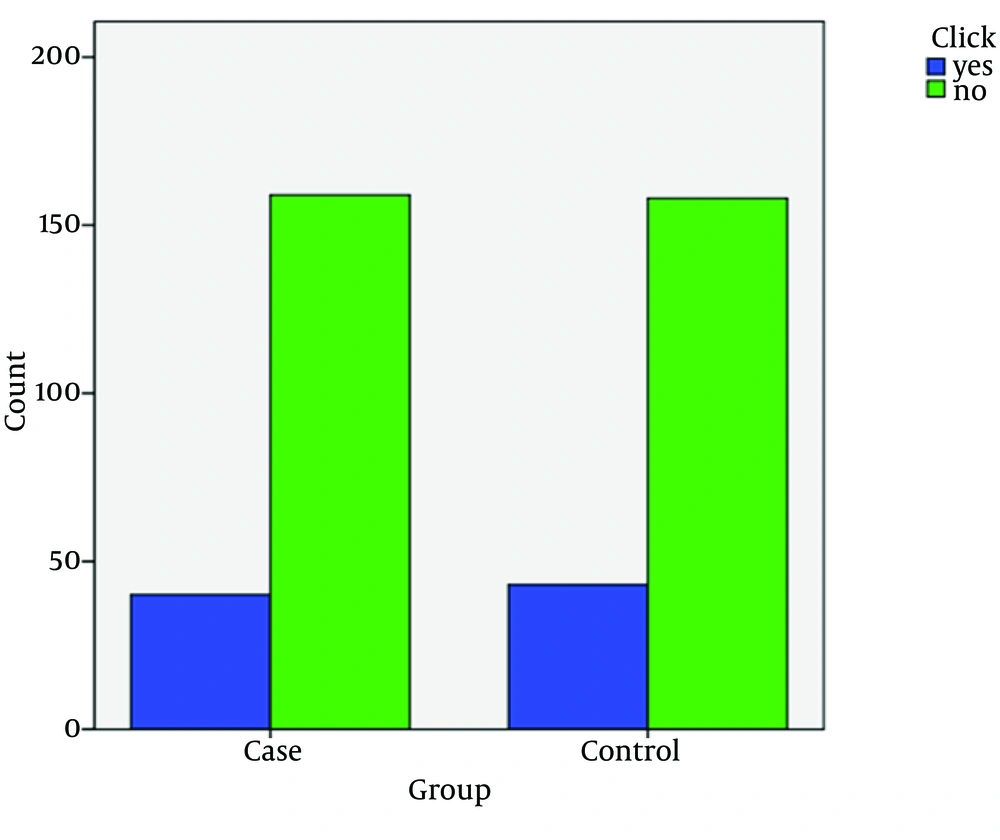
With regard to TMJ click, this condition was observed in 20.1% of the patients under 30, 24.4% of those between 30 and 50 and in 15.9% of the patients more than 50 (Figure 4). The differences between the groups were not significant (P value = 0.241). Figure 5 shows the prevalence of TMJ click in the army and civilian groups. Although the army group had slightly more TMJ click, but the difference was not significant at all (P value = 0.423). Pain or tenderness of the masticatory muscles and TMJ in palpation was infrequent. This condition was seen only in 1% and 4% of the patients under 30, 3.4% and 5% of those between 30 to 50, and 1.68% and 3.34% of the patients older than 50, respectively. No statistically significant difference was found between the age groups or between army and control group.
Out of 400 participants, only 1 had limitation in mouth opening; who was a 55-year-old man in the army group.
5. Discussion
Temporomandibular joint disorders (TMD) have been associated with numerous etiological factors, among them bruxism is the one, which requires delicate consideration. There are a few references in the literature to show the correlation between temporomandibular joint disorder and attrition. It is not certain whether attrition is the cause of TMDs or vice versa. Moreover, to the best of our knowledge, there has been no study about army personnel and the prevalence or severity of the TMDs or attrition among them. With this objective in mind, this study was conducted among the targeted population (army personnel) between 18 and 75 years of age to assess the prevalence of the TMDs and ascertain the interrelationship between these factors. The basic data from 400 participants consisting of 222 males and 178 females were statistically analyzed. The results showed that army personnel had statistically significant more dental attrition in comparison to the normal population. Moreover, this condition was significantly more prevalent in those who had participated at war (P value = 0.001).
As expected, the prevalence of dental attrition increased with age. This is in complete accordance to the findings of Yadav in 2011 (12). In fact, this is partly a result of the functional and physiologic function of the oral system and natural wear through the years; but the higher prevalence of dental attrition in army personnel, especially in those participated at war, strongly advocates the copious mental pressure and stress in those people. On average, 21.6% of the people participated in the present study had TMJ click on opening or closing. Akhter et al. (13), in their study on 1930 people of different ages, reported a 16.5% prevalence rate for TMJ click. Solberg et al. (14) also mentioned that 17% of the population in their study had TMJ click. In our study, the prevalence of TMJ click was higher in females (P value < 0.05). Many other studies reported the same findings (1, 2 and 28).
Regarding TMJ click, limitation in mouth opening, and pain or tenderness of TMJ or masticatory muscles on palpation, there was no statistically significant difference between army and civilian group. One reason may be the extremely infrequent prevalence of these conditions in healthy population. In fact, the mentioned conditions only exist in those with chronic, severe, and end-stage TMDs. Having in mind that TMDs or dental attrition may cause several problems, (hypersensitivity of the teeth, nerve involvement and pain, reduction in vertical dimension, and difficulty in prosthesis fabrication) it is urgent to screen the army personnel, especially those participating at war or other high stressful duties, for these ailments. The best treatment is to prevent or stop the condition at initial phase. One highly documented treatment for dental attrition is par-time wear of night guard. Night guard is a protective shield covering the occlusal surface of all the teeth. It is made of soft or hard acrylics, and the fabrication is extremely easy and inexpensive. Wearing the night guard, the patient is no longer capable of doing the bruxism involuntarily.
Dental attritions are significantly more prevalent among army personnel. Moreover, the prevalence of such problem was significantly more in those participated at war. Regarding other TMDs (TMJ click on opening or closing the mouth, limitation in mouth opening, and pain or tenderness of TMJ or masticatory muscles on palpation), no significant difference was found between army personnel or civilians. For those at high risk of initiation of dental attrition, part-time wear of a night guard is recommended.