1. Context
These days the global community is facing an international emergency and everyday hears bad news about Ebola victims. By October 8, 2014, a total of 8033 infected cases have been reported including 3845 death from Ebola virus disease (EVD) (1). The dimensions of this humanitarian crisis were broad enough to motivate United Nation Security Council for launching an emergency health mission and military intervention (2) because of the situation that was called “a threat to international peace and security” (3). However, there have been several criticisms about the military engagement for the epidemic control. While a limited number of options remained for the health authorities, this issue should be appropriately discussed in military medicine organizations in order to make the best possible policy. From the military perspective, the clarification of the mission and gathering information is the first priority for this combat. Then, assessing the resources and preparedness and constructing battle strategies and control measures would be the next steps.
2. Evidence Acquisition
A comprehensive review was accomplished on all important reports, articles, statistics and guidelines about the current EBV outbreak from official internationally reputed authorities including World Health organization (WHO) and Centre of Disease Control (CDC). Also, literature search for military contribution in the EBV outbreak control programs and military missions to the epidemic regions was executed. The evidence for and against the potential roles of military units in the current war against Ebola outbreak were searched and critically appraised.
3. Results
3.1. Ebola Outbreaks
The current outbreak is the 25th known outbreak of Ebola virus (EBV). EVD first appeared in 1976 in two outbreaks in African remote villages. The virus adopted its name from a river in this region. In contrast to previous epidemics of EBV, which were limited to urban districts in the central Africa, the current outbreak in West Africa, which was officially announced on March 23, 2014, involved both rural and urban area and was the largest and most complex Ebola outbreak ever with a considerable number of death that exceeded the total mortality of all previous outbreaks (2). It has spread across the land borders in West African states, namely, Guinea, Sierra Leone, Liberia, Nigeria, and Senegal, where are known to have a weak health system and fragile human and infrastructure resources. Importantly, EVD is spreading via air travel that has distressed global community to feel this threat, as noted in some warnings like “Ebola, only a plane ride away”. Therefore, the WHO director-general declared the EVD epidemic as a “public health emergency of international concern” on August 2014 (4, 5). Unfortunately, several cases of transmission to health workers and international aid workers have been reported, including more than 100 infected medical practitioners with about 50% mortality (6). Consequently, apart from the infection epidemic, an epidemic of fear is of concerns for the authorities, which has turned to a barrier for entering aids to the infested area, particularly the “Red Zones”, which has been described too unsafe to travel by the Doctors Without Border Organization.
EVD would turn to endemic in the affected areas where become a reservoir for the virus spread to other regions (2). The devastating course of this round of EVD epidemic is attributed to the malfunctioning health system and lacking of infrastructure due to long-term instability and armed conflict rather than to the biologic characteristics of the virus. It seems that the present epidemic is exceptionally large, not principally due to biologic characteristics of the virus, but because of the affected population, insufficient control efforts, and lack of infrastructure (7) leading to rapid geographic dissemination of EVD. Unfortunately, experts criticized the current responses “too slow, poorly founded, conservative, and ill prepared” (2). This makes the world more prone to future epidemics by emerging and re-emerging diseases (Figure 1).
3.2. Ebola Transmission
The fruit bats of the Pteropotidae family have been supposed as the natural host of the EBV (1). EBV is introduced to human population by direct contact to blood, body secretion, or organs of infected wild animals. EVD then can be transmitted from one human to another through direct contact to an infected person’s blood, body fluids (8) including semen and milk, or surface and materials contaminated with these fluids (1).
Although infected individuals are not transmitting infection until they develop symptoms, the body fluids of a patient might play a role in transmission up to seven weeks after recovery (1). Recently contaminated objects, floor, or bed linens could be a source for transmission (9); however, airborne transmission has not been documented (10). It is important to note that the disease could be transmitted during an unprotected burial ceremony from the direct contact to deceased person. Since the patients are unknown at presentation to the medical centers, healthcare workers are prone to contract the disease (1). The estimated basic reproduction number (R0) ranged from 1.20 to 2.02 in the outbreak regions (7), which was similar to previous epidemics.
3.3. Ebola Clinical Aspects
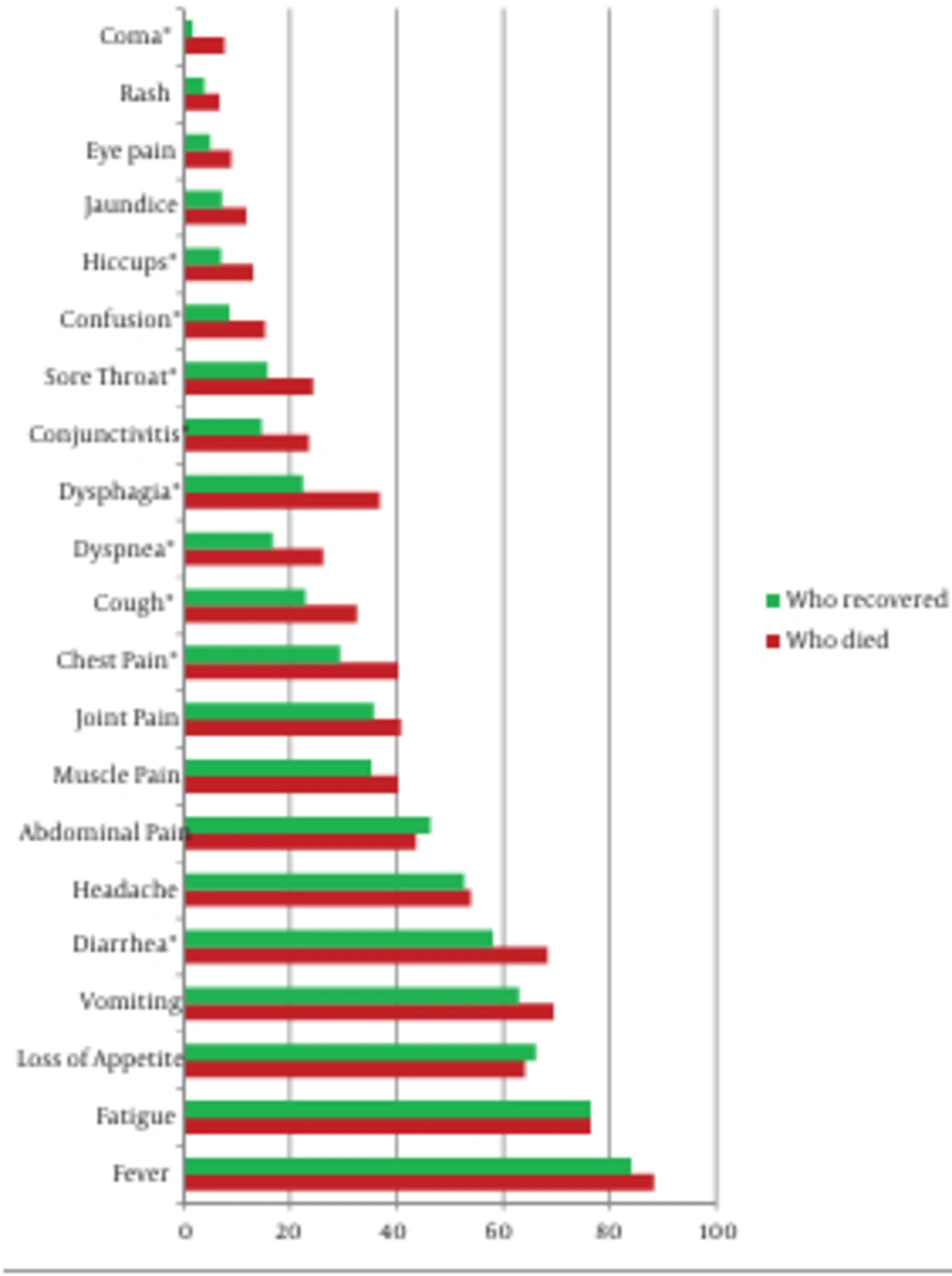
EVD is more frequent among 15- to 44-year-old individuals with no gender dominancy (7). The incubation period ranges from two to 21 days (11.4 days in average in recent reports) (7, 8). EVD firstly presents with nonspecific manifestations such as a sudden onset of fever, fatigue, muscular pain, headache, and sore throat that are followed by vomiting, diarrhea, and rash. Moreover, signs and symptoms of impaired renal and liver function might exhibit in conjunction with elevated liver enzymes and leukopenia (1). Although previous epidemics were associated with considerable frequency of internal and external bleeding, specific hemorrhagic symptoms were rarely reported in the current outbreak (7). This diversity might be due to limitations in reporting from the affected areas. A recent study reported a difference between some presentations in the fatal and nonfatal cases as illustrated in the Figure 2 (7). The main risk factors of death are age (> 45 years old), a number of general symptoms (e.g. diarrhea, dyspnea, dysphagia, conjunctivitis, and impaired consciousness), and hemorrhagic symptoms (7).
The case fatality rate has been estimated as being 70.8% (95% confidence interval [CI], 69-73) in the current outbreak (7). Surprisingly, more than 44% of cases and 52% of all deaths from EVD in this epidemic were reported from healthcare workers. The case fatality rate among this group ranged from 56% to 80% in the affected regions (7). Differential diagnosis from other infections including malaria, typhoid fever, shigellosis, leptospirosis, dengue, yellow fever, and meningitis could be done by virus isolation through cell culture, reverse transcriptase polymerase chain reaction (RT-PCR), and enzyme-linked immunosorbent assay (ELISA) (1, 10).
3.4. Treatment
Supportive care including intravenous fluid replacement is necessary. Furthermore, blood products, immune therapies, and drug therapies would be essential in some cases (1); however, there is no specific treatment for EBV. Two potential vaccines are undergoing human safety test but they have not been licensed yet.
3.5. Control Strategies
The current epidemic highlighted this fact that classic “outbreak control” efforts are no longer sufficient for an epidemic in this size (2). Holistic coordinated humanitarian as well as social and medical measures should be formed against this crisis. Nevertheless, from medical points of view, because EBV is spread mainly through contact with body fluid of symptomatic patients, transmission can be stopped by a combination of early diagnosis, contact tracing, patient isolation and care, infection control, and safe burial (1, 7). These responses must be complemented by the development of diagnostic tests, therapies, and vaccines as a priority (2).
3.5.1. Surveillance
Suspected, probable, and laboratory-confirmed cases and their contacts, and demographic, geographic, and clinical information must be recorded (7). The guideline for suspected and probable cases is indicated in the Table 1.
| Responses | Military Forces | Military Medicine Systems |
|---|---|---|
| Humanitarian aid | * | * |
| Crisis management | * | |
| Technical support | * | * |
| Logistic and equipment | * | |
| Communication and transport | * | |
| Training and education | * | |
| Case management | * | |
| Diagnosis | * | |
| Treatment | * | |
| Surveillance | * | |
| Personal protection | * | * |
| Social mobilization | * | * |
| Security | * | |
| Emergency response center | * | * |
| Establishing infrastructure | * | |
| Information management | * | * |
| Research | * | |
| Product development | * | |
| Crisis management | * | |
| Burial | * | |
| Quarantine | * | * |
| Preventive strategies | * | * |
3.5.2. Risk Management
For an effective risk management and control of transmission, one must focus on reducing the risk of wildlife-to-human as well as human-to-human transmission and outbreak containment measures. Direct contact with or handling of wild animals such as infected fruit bats or monkeys/apes or their body fluids, meat, or blood should be prohibited. Similarly, a proper protection against body fluids of infected patients must be applied (1). Sexual intercourse with an infected man is forbidden for at least seven weeks after his recovery (10).
The risk of EBV transmission to travelers to the epidemic areas is extremely low; however, travelers are advised to avoid blood and secretions of the infected persons or direct contact with dead victims (10). In the airports, seaports, or ground cross-borders, infrared screening equipment should be implemented to detect febrile passengers and symptomatic patients must be quarantined. Visitors who return from affected areas should be informed that they might develop the symptoms within three weeks of their arrival or their risky exposure to the virus. Adequate facilities for water and soap or alcohol-based hand rub personal protective equipment (PPE), safe injection and waste management, and medical services should be provided in the ports (10). Travelers should be informed of places to obtain medical assistance in their destination.
Healthcare workers and laboratory staff are at risk and should apply infection control measures according to the WHO guidelines including head cover, face shield, goggle, fluid-resistance mask, respirator (when required), double gloves, gown (preferably disposable), waterproof apron, and foot wear. However, beware of heat stress, particularly in warm humid weather (10) (Box 1). Sterile gloves are not required except for sterile procedure. Nitrile gloves are preferred over latex gloves for health workers because they are resistance to chemicals. Use of tape to attach gloves to gowns should be avoided due to its interference with safe gown removal (10).
The fear of spreading the epidemic, particularly after the detection and death of some healthcare volunteers in developed countries, led local governments to an extreme quarantine response for the doctors, nurses, and other health workers who return from epidemic regions. This response was supposed offensive for the volunteers who were risking their lives to help others and was followed by a massive apposition movement by scientists (9). It is noteworthy that asymptomatic patients are not contagious. Then, quarantine should be limited to symptomatic individuals, particularly for healthcare workers who return from infected areas (9); otherwise, it becomes a barrier for volunteer health workers to contribute in the epidemic control. However, they must be followed up for 21 days for any symptoms, based on a scientific protocol rather than a blind fearful response (Figure 3).
| Standard Precautions | Healthcare workers |
|---|---|
| Hand hygiene | Risk assessment of work place |
| Point of care risk assessment for appropriate PPE | Adequate control measures for workers at risk |
| Respiratory hygiene | Informing healthcare workers of the risk |
| Prevention of needle-stick or sharp injuries | Educating healthcare workers for using appropriate PPE |
| Safe waste management | Considering climate and cultural barriers for PPE use |
| Cleaning and disinfection of patient care equipment and linen | Providing sufficient PPE for healthcare workers |
| Cleaning and disinfection of the environment | Follow-up up to 21 days after returning from epidemic zones |
a Abbreviation: PPE, personal protective equipment.
3.6. Laboratory
Laboratory diagnosis could be made by antibody-capture enzyme-linked ELISA, antigen-capture detection tests, serum neutralization tests, RT-PCR assay, electron microscopy, or virus isolation by cell culture (1). PCR would be positive two to three days after symptoms onset (9). Suspicious samples are considered as extremely hazardous and particular caution and precise instruction must be applied during transferring samples to the laboratory centers (10).
In order to protect laboratory personnel, PPE (e.g. plexiglass splash guard, eye protection, double gloves, fluid resistance gown, and mask) should be properly applied (10). The proper donning and removing PPE is essential for workers' safety, and strict adherence to protocols is expected. It is noteworthy that changing to unfamiliar equipment or PPE without sufficient training and practice might lead to breaches in safety practices and might increase a person’s risk of contaminating their clothes, mouth, or eyes, especially when removing PPE (10, 11).
A minimum volume of 4-mL whole blood in plastic collection tubes can be used to submit specimens for testing for EBV. Do not submit specimens to CDC in glass containers or in heparinized tubes. Whole blood, preserved with EDTA, is preferred but whole blood preserved with sodium polyanethol sulfonate (SPS), citrate, or clot activator is acceptable. It is not necessary to separate and remove serum or plasma from the primary collection container. Specimens should be immediately stored or transported at 2℃ to 8°C on frozen or cold-packs to the referral laboratory (11).
For decontamination purpose, no particular disinfectant has been introduced and EBV is sensitive to a broad range of routine hospital disinfectants. Laboratory wastes must be processed according to the standards for the category an infectious substance (11). During transport, specimens should be placed in a durable, leak-proof secondary container for transport within a facility. To reduce the risk of breaking or leaks, do not use any pneumatic tube system for transporting suspected specimens (11).
3.7. Education
Education is the key element in combat against Ebola. Lack of education and misunderstanding the transmission are important barriers to the outbreak control. This should cover public, health providers, community hygiene workers, flight crew, airport personnel, social activists, burial service workers, and of most importance, military forces.
3.8. Assessment of Preparedness
There have been extreme claims of a lack of preparedness or a complete preparedness among nations (5); however, a realistic assessment is required for every nation against emerging and re-emerging outbreaks. In addition to the “healthcare preparedness capabilities” (8), Ebola planning and response requires readiness in six key public health preparedness capabilities including:
- Emergency public information and warning
- Information sharing
- Nonpharmacologic interventions
- Public health laboratory testing
- Public health surveillance and epidemiologic investigation
- Responder safety and health
WHO has released a preparedness checklist, which includes laboratory testing capacities, treatment capacities, contact tracing, safe burial, and social mobilization. Preparedness is the key factor in controlling the outbreak. While the risk of the disease might be very low in countries with no or limited connection to the epidemic areas, every hospital should have a plan for detection, isolation, treatment, communication, and reporting as well as disposal of body fluids and control measures for suspected cases. Required precaution must be considered for ambulance staff, admission offices, and waiting rooms (5).
3.9. The Ebola Threat for Military Services
Military units encounter a general risk for Ebola because of their environment with close contacts between individuals. Nevertheless, since asymptomatic patients are not contagious, the risk would be controlled if proper control strategies were applied. From different perspective, armed forces would be affected by Ebola as a biologic weapon. The former Soviet Union investigated Ebola as a biologic weapon during the Cold War, but did not mass-produce the virus as a weapon (12). It is assumed that the Japanese cult AumShinrikyo group tried to acquire samples of Ebola in 1993 for bioterrorism purposes. Then, the biodefense organizations started efforts against this risk (12). As a result, military forces should be prepared to combat naturally occurring outbreaks as well as biologic warfare containing the virus. Finally, military forces are vulnerable to EVD during their deployment to the affected areas. Therefore, effective education for self-care and prevention must be considered for all soldiers and military personnel before their mission. They must also know about Ebola response roadmap to help in prevention of the disease transmission, caring of the patients, supporting their relatives, and approaching to deceased patients.
3.10. The Potential Role of Military Units
Since the UN Security Council declared EVD as a threat to international peace and security, the epidemic became a military mission. Consequently, for instance, the US military has mobilized 3000 troops and 750 $ million in defense funding to combat Ebola and run a 25-bed hospital in the epidemic region (3). Germany has asked its military personnel to volunteer for duty in West Africa, and France and Britain have sent their forces to the region (3). These missions and securitization of the Ebola epidemic have been opposed by several health organizations and medical experts including the “Doctors Without Borders”. The affected regions have suffered from incompetent health system, fragile infrastructures, and insufficient education. Furthermore, healthcare workers and volunteers have not enough security in those districts (13). While some people accused governments for spreading the disease deliberately (as it was for the Swine Flu and SARS epidemics), and bizarre reports in media and among people introduced mysterious armed men who poisoned wells to kill people in the name of Ebola (13), the cultural and social believes must be taken into account for any decision about military deployment to the affected states. Then, oppositions indicated that civil humanitarian aid, social support, and strengthen local government instead of a massive military intervention would have bigger advantages. As a result, prioritization of military deployment has been assumed as the worse outcome of the crisis (3). There would be no need for military inclusion in the war against EVD, if timely response were initiated for this epidemic. In fact, education is the main solution (13).
Although there are objections against military deployment, authorities considered military contribution as the only solution left (3). The mortality due to EVD is comparable to the civil war that the region experienced a decade ago. Furthermore, the disease social burden and economic impact on the already-poor affected countries and the potential of spreading the disease to the neighbor states and even to Asian high-populated countries, have urged using military capacities in the disease control programs as the last resort, in order to control epidemic at its source (10).
Then, the recent international plans for EVD epidemic control include contribution of military organizations, “when appropriate” (2). In other words, military intervention must be applied in appropriate time, for appropriate job, and with appropriate quality; however, there is a wide diversity in interpretation of the word “appropriate”. Given the main pathways demonstrated in the WHO roadmap for EVD control roadmap (4), the potential role of military organizations in general, and military medicine authorities in particular, must be revised. We illustrated these roles in the following table.
The great capacities of military services in logistic, mobilization, constructions, communication, and human resources could be shared with civic organizations for humanitarian aids and strengthen infrastructure in the diseased regions. In addition, the medical facilities of the armed forces could be presented to the public and the military or defense research institutes must contribute to the development of effective treatments and vaccines. Moreover, military forces could contribute in the education and health promotion, if there were good education for their own in first place, in conjunction with health authorities and civil defense. Finally, their role in security establishment could be critical in some regions.
4. Conclusions
Ebola is an international threat and a global action is required against this outbreak. Particularly the epidemic zones deserve humanitarian aid as well as medical assistance from international community. Then, military units could play major role in the context of a global action against this epidemic; however, there are criticisms of the way of action and the potential roles that armed force should take. This must be discussed by military medicine authorities and requires an integrated responsive network of international community.