1. Background
General health status and quality of life today are closely associated with oral and dental health (1, 2). Oral and dental diseases such as dental caries and periodontal disease are common and can lead to physical, functional, and biological complications. Moreover, these conditions affect other aspects of a person’s life, including economic, social, and psychosocial aspects (3).
Collection of data on the prevalence and incidence of oral and maxillofacial diseases among the military forces is important because it facilitates the design of interventions and management of the dental care system in the forces (4). This is of higher importance in relation to submarine crews because of the specific working conditions they experience when on missions (5).
Submarine crews are prone to experience oral and dental problems. There is a variety of reasons for this, including the restrictions on oral hygiene measures when they are on missions (6). Moreover, crews that are on missions live are in isolated environments without access to dental care services (5). According to reports, five dental emergency cases per 100000 persons per day occur during submarine operations (5).
Stressful occupational conditions may lead to the occurrence or aggravation of some oral lesions, including oral lichen planus and aphthous stomatitis (7-10). Moreover, sleep disorders related to the disruption of the day-night cycle are frequently observed in submarine crews; this in turn can lead to the occurrence of oral problems such as oral lichen planus and burning mouth syndrome (11, 12). Stress can also lead to myofacial pains and temporomandibular joint (TMJ) disorders because of hormonal changes (13, 14). Stress can also be related to dental caries, through the establishment of dry mouth (15, 16).
2. Objectives
Due to the lack of studies on the prevalence of oral and maxillofacial diseases in Iranian submarine crews, our objective was to compare the clinical examinations, questionnaire results, and radiographic examinations of such a crew with a marine group. If necessary, the results could be used as a basis for future interventions and recommendations for appropriate measures to reduce the rate of oral and dental problems in submarine crews.
3. Materials and Methods
This cross-sectional study was performed on 102 Army personnel. The study population consisted of a submarine crew of 74 and a marine cohort of 28. All participants signed a written informed consent statement prior to the study. The samples were selected by simple random sampling. The data were collected using a questionnaire that contained items of demographic data, medical and dental history, behaviors related to oral and dental health, and the probability of emergency dental conditions occurring during a mission. The questionnaire was based on available questionnaires in this field (17, 18) and the consensus of three faculty members of the school of dentistry. To fill out the questionnaire, all participants were examined by a dentist. Since panoramic radiographic images are considered to be acceptable for screening (19, 20), and considering the need to take periodic radiographs for check-ups, panoramic images were obtained from all the participants. The radiographs were evaluated by two dentists using a negatoscope in a room with appropriate light.
In this study, the DMFT index (decayed, missing, and filled teeth), rates of root canal filling, pulp involvement and periapical lesions, oral lesions, tooth wear, dental fluorosis, dental calculus, dental trauma, clicking in the TMJ, problems during the mission, health behaviors, the rate of dental visits, and public health condition were evaluated in the both groups.
In terms of dental fluorosis, the participants were categorised as follows: lack of fluorosis (normal and questionable), mild fluorosis (very mild and mild), and defined fluorosis (moderate and severe) (21). The participants were classified by lack of dental attrition (grade 0), mild dental attrition (grades 1 and 2), and defined dental attrition (grades 3 and 4) (22).
The data collected from the questionnaires were analyzed by SPSS version 20 using appropriate statistical tests such as the independent t-test, Fisher’s exact test, chi-square, and Mann-Whitney U. Any P values of less than 0.05 were considered statistically significant.
4. Results
The mean age of the submarine and marine groups were 3.30 ± 28.5 and 4.62 ± 29.85 years, respectively. According to the results obtained by the independent t-test, the two groups were not significantly different in this regard (P = 0.163).
The DMFT index of the submarine group was lower than that of the marine group, and the difference was statistically significant (P = 0.01) (Table 1). Among the submarine and marine groups, 52.7% and 53.6% had root-filled teeth, respectively.
aData are presented as mean ± SD.
bIndependent t test.
cThe difference is significant.
The frequency of periapical lesions in the submarine and marine groups were 21.6% and 10.7%, respectively, showing a significantly higher value for the submarine group (P = 0.034). The two groups were not significantly different in terms of pulp involvement (P = 0.276) (Table 2).
aData are presented as mean ± SD.
bIndependent t test.
cThe difference is significant.
It was observed that the prevalence of aphthous stomatitis in the submarine group was significantly higher than that of the marine group (29.7% vs. 3.6%) (P = 0.003) (Table 3).
The two groups were significantly different in terms of dental attrition rate, with the marine group having the higher rate (P < 0.001). The two groups were not significantly different in terms of dental fluorosis, calculus and trauma, and TMJ click (P > 0.05) (Table 4).
aData’s unit is %.
bMann-Whitney U test.
cThe difference is significant.
dChi-square test.
eFisher’s exact test
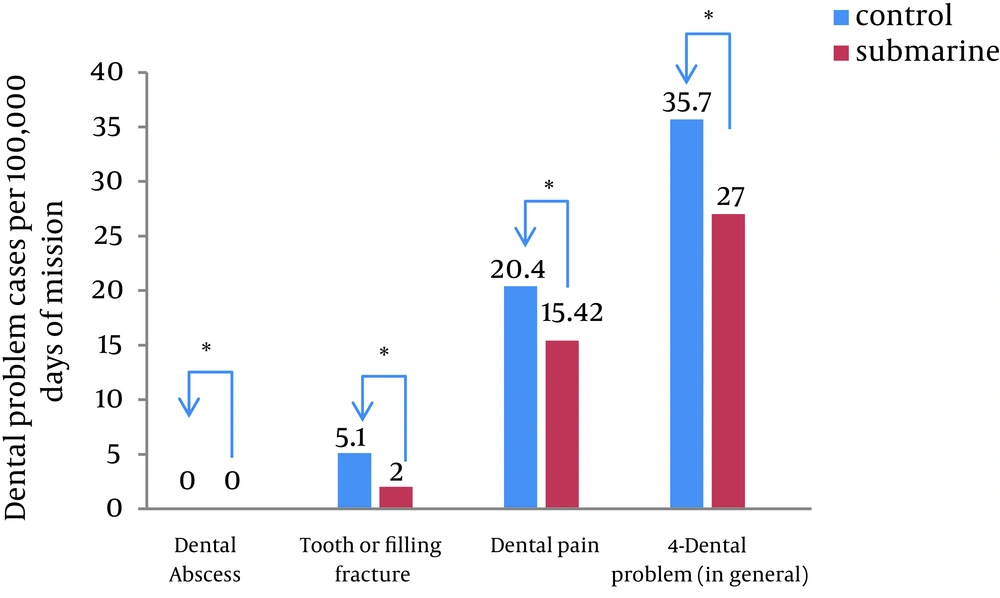
The incidence rate of dental problems per 100000 days of mission was 27 and 35.7 for the submarine and marine groups, respectively (Figure 1).
Frequency rates for appropriate tooth brushing technique in the submarine and marine groups were 14.9% and 21.4%, respectively. The difference was not statistically significant (P = 0.30). Frequency of behaviors related to oral and dental health, including using dental floss and tooth brushing, in the two groups are shown in Table 5.
aData’s unit is %.
bMann-Whitney U test.
cChi-square test.
The two groups were not significantly different in terms of the rate of dental visits (P = 1.66). Among the submarine and marine groups, 63.6% and 75% had regular dental visits of at least once every two years (Table 6).
It was found that the level of expressed stress in the submarine group was significantly higher than the marine group (P < 0.001). Moreover, none of the participants in the marine group received medications for long-term illnesses, while 10.8% of the participants in the submarine group took medications for long-term illnesses (46.1% psychiatric drugs, 38.4% GI drugs, and 15.5% other medications) (P = 0.01) (Table 7).
aData’s unit is %.
bFisher’s exact test.
cThe difference is significant.
dChi-square test.
5. Discussion
The objective of the current study was to determine the prevalence of oral and maxillofacial diseases among a submarine crew. According to the results, the DMFT index and the number of missing teeth were significantly lower in the submarine group than in the marine group. Periapical lesions were significantly more prevalent in the submarine group (P < 0.05). Moreover, the level of stress, rate medication consumption for long-term illnesses, and prevalence of aphthous stomatitis were higher in the submarine group than the marine group (P < 0.05). The two groups were not significantly different in terms of behaviors related to oral and dental health (P > 0.05).
In two different studies that Hopcraft et al. performed on the Australian military staff in 2003 and 2005, they reported the DMFT index to be 7.07 ± 5.16 (D: 1.32, M: 1.21, F: 4.54) and 5.48 ± 4.85 (D: 1.5, M: 0.34, F: 3.68), respectively, among the staff in the age range of 26 - 30 years (23, 24). The mean values obtained in the current study were 5.24 ± 4.16 (D: 1.69, M: 0.74, F: 2.81) and 8 ± 5.94 (D: 2.04, M: 3.57, F: 2.53) for the submarine and marine groups, respectively. This indicates that the population of the current study had less of a chance for a decayed tooth to be repaired than that of Hopcraft et al.’s studies. This could be attributed to the lack of regular dental care programs, lack of required treatment facilities, or lack of correct attitude toward necessity of treatment for decayed teeth in the population of the current study.
Skudutyte-Rysstad et al. performed a study in Oslo, Norway in 2006 and reported that 23% and 16% of the individuals studied had root-filled teeth and periapical lesions, respectively (25). In a 1995 study in Oslo, Norway, Eriksen et al. reported that 53% and 30% of the individuals studied had root-filled teeth and periapical lesions, respectively (26). In the present study, 52.7% and 53.6% of the individuals in the submarine and marine groups had root-filled teeth, respectively, while periapical lesions were observed in 21.6 % and 10.7%, also respectively.
Fluorosis may have destructive effect on dental enamel. It has been shown that mild fluorosis occurs in 12 - 33% of the population in areas where fluoride concentration in the drinking water is in the range of 0.9 - 1.2 mg/L (21). In the present study, 18.9% and 17.9% of participants in the submarine and marine groups, respectively, had mild fluorosis, and 5.4% of subjects in the submarine group had moderate to severe fluorosis. The rate of fluorosis in the population of the current study could be explained by the high concentration of fluoride in the drinking water of some areas in the southern part of the country.
In a 2011 study, Yadav et al. reported that 18.5% of the individuals in the age range of 25 - 35 years had dental attrition of grade 2 or higher (wear completely destroyed the enamel and reached the dentin) (22). In the present study, 14.3% of the participants in the marine group had severe dental attrition, but no cases of severe dental attrition were observed in the submarine group. In general, the two groups were significantly different in terms of the presence and severity of dental attrition. Farzaneh et al. carried out a study on the Army personnel and civilians in Iran and concluded that the dental attrition rate is higher among army personnel (27). Moreover, among the army personnel, the dental attrition rate was higher in those who participated in war. In their study, attrition was defined as tooth wear higher than 1 mm. They reported the prevalence of dental attrition by as much as 9.9% among the army personnel. Based on the above definition, in the present study, 6.8% of subjects in the submarine group had dental attrition.
In two studies, Seligman et al. (28) and Yadav (22) reported the prevalence of TMJ click by as much as 17% and 22%, respectively, of their study populations. In the present study, 2.7 % of subjects in the submarine group had TMJ click. The difference between this study and previous studies could be due to the method of assessment used by observers.
Submarine missions are among the most stressful military missions. Factors such as being away from one’s family, disruption of the circadian cycle, working in a confined space, isolation from the outside world, and potential dangers of the missions could increase the stress level in submarine crews (29). Stress could lead to development or aggravation of some oral lesions, including lichen planus (7, 9), aphthous stomatitis (30, 31), and herpes lesions (30, 32). Recurrent aphthous stomatitis is a common and painful mucosal lesion; its possible etiologic factors include genetic factors, vitamin deficiency, immune dysfunction, stress, etc. (33, 34). In some studies, a direct relationship has been reported between stress and the occurrence of aphthous stomatitis (8, 9, 33-37). Such a relationship could not be found in some other studies (38, 39). Huling et al. demonstrated that stressful conditions can increase the occurrence frequency of aphthous stomatitis, but does not affect the duration of the lesions (35). According to the results obtained in the current study, the frequency of aphthous lesions in the submarine group was significantly higher than that in the marine group (P < 0.05). This could be explained by the stressful working conditions of the submarine crew.
In a 2008 study conducted by Deutsch et al. on the US submarine force, the incidence rate of dental problems was reported to be 5 per 100000 days of submarine missions (5). In another study performed by Ludwick et al. in 1974, the number of dental problems among the navy personnel serving in Vietnam was 42.9 for every 100000 days of missions (40). In a study on the land-based marine corps in 1996, this index was reported to be 40.6 per 100000 days of missions (41). According to the results obtained in the present study, the index was 27 and 35.7 for the submarine and marine groups, respectively. The difference observed between various studies could be attributed to the different health programs and health care in the various study communities. Moreover, the higher rate of dental problems among the marine group could be explained by providing better health care to the submarine group because of the occupational issues (job sensitivity) in the submarine group and their lack of access to dental care services on missions.
In a 1970 study on a submarine crew, Belmont et al. reported that 59% of the study population brushed their teeth twice or more per day (42). In the current study, the corresponding rates were 36.5% and 42.9% for the submarine and marine groups, respectively. In Deutsch’s study of an American submarine crew, the average rates of tooth brushing and dental flossing were 1.79 and 0.63 times a day, respectively (5). In the present study, the values were 1.35 and 0.473, respectively, for the submarine group and 1.36 and 0.42, also respectively, for the marine group. This perhaps indicates that the necessity of attention to oral care should be emphasized more in the population of the current study. It should be noted, however, that use of the appropriate method of tooth brushing and dental flossing is more important than the frequency of these practices. This indicates a need to provide the necessary training.
The advantages of the current study include a lack of similar studies in Iran and the use of a paraclinical diagnostic method (radiographic imaging) in addition to the clinical examination. Moreover, this survey considered many problems related to the mouth and jaw, including some oral lesions, in addition to dental problems.
Based on the results of this study, the following suggestions are provided: training in the appropriate measures of oral and dental health, including tooth brushing and use of dental floss, carrying out preventive measures, providing high quality dental care, and reducing stress levels in submarine crews to prevent the incidence or aggravation of some oral lesions.
5.1. Conclusions
In general, the oral and dental health status of the submarine crew was better than that of the Marine group. The prevalence of aphthous stomatitis, however, was significantly higher in the submarine group; one of the etiologies considered for this condition is stress.