1. Background
Insulin resistance is a state in which cells are unable to respond to the normal actions of the insulin. Therefore, the blood sugar increases. High levels of blood sugar cause high levels of insulin production and it leads to down regulation of the insulin receptors. It means that there is a relative resistance to insulin despite the high level of insulin in the hospital staff. Previous studies showed that insulin resistance results in the cluster of lipid disorders, hypertension and glucose intolerance (1-4). Therefore, insulin resistance is a risk factor for developing heart disease and type 2 diabetes (5).
Several factors increase the risk of insulin resistance. Stress is one of the important risk factors. Stress results in various emotional and physical disorders including depression, anxiety, heart diseases, hypertension and immune system disturbances that increase vulnerability to infections (6-8). A major source of stress is job stress. Job stress is mentioned as a significant health problem. Tehrani et al., reported a significant relationship between job stress and mental health in a study on the effect of stress on the nurses of emergency wards (9).
Stressful work situations such as: uncontrollable workloads, lack of job security, poor relationship with colleagues, lack of involvement in decision making, inadequate support from colleagues and superiors, dull and repetitive work, inadequate information about roles and responsibilities affecting both individual and organization lead to physiological responses that may finally contribute to sickness (10-12). Some reports show that medical staff faces high levels of stress at work because any medical errors or mistakes may threat patient’s life which is sometimes irreversible. In addition, medical staff always faces suffering and death (13-15).
2. Objectives
The current study aimed to: 1, identify the job stress level among medical staff of the Imam Reza hospital; 2, measure the insulin resistance among medical staff of Imam Reza hospital; 3, determine the relationship between job stress score and insulin resistance.
3. Methods
3.1. Participants
Participants included all the staff working in different departments of Imam Reza hospital, Tehran, Iran, from July to August 2013. Hospital departments included paraclinic, intensive care unit (ICU) and hospital wards.
Paraclinic department included odontology, pharmacy, pathology, radiology and central laboratory. Intensive care unit included ICU, coronary care unit (CCU) and emergency ward. Hospital wards included internal medicine, general surgery and operating rooms.
The Osipow questionnaire was used to assess the level of job stress among staff. The questionnaire consists of 60 statements based on a 5-point Likert scale; 5 for most of the times, 4 for usually, 3 for often, 2 for occasionally and 1 for never. Total score on this scale is considered in the assessment of occupational stress. Higher scores on this scale indicate more stress.
A copy of the occupational stress inventory (OSI) was given to the health care personnel. The completed questionnaires were analyzed by another person in the university.
Serum glucose level was measured by glucose oxidase-peroxidase (GOD-POD) method employing standard kits (Pars Azmoon, Karaj, Iran); fasting insulin level was also measured by enzyme linked immunosorbent assay (ELISA) using commercially available kits (Monobind, Inc. Lake Forest, CA, USA).
Insulin resistance was quantified using the homeostatic model assessment of insulin resistance (HOMA-IR) according to the formula: fasting insulin (microU/L) × fasting glucose (nM/L)/22.5 as previously reported by Matthews et al. body mass index (BMI) is body weight in kilograms divided by the square of height in meters (16). All participants in this study signed the informed consent form and the study was approved by the ethical committee of the AJA University of Medical Sciences, Tehran, Iran.
3.2. Statistical Analysis
All results were displayed as mean ± SEM (standard error of mean). Statistical analysis of data was carried out by SPSS ver. 16. One-way analysis of variance and Post-Hoc tests were used to analyze different variables among the staff of different departments. Correlation analysis was performed to analyze the relationships between insulin resistance and dependent variables (age, job stress level and BMI).
Data analysis was performed using SPSS software version 16. P values ≤ 0.05 were considered significant.
4. Results
In total, 97 subjects (36 male and 61 female) participated in the study. Some anthropometric and clinical measurements of subjects are summarized in Table 1.
| Groups | Age, Y | Weight, kg | Height, m | BMI | Glucose, mg/dL | Insulin, μIU/mL | Insulin Resistance | Stress Score |
|---|---|---|---|---|---|---|---|---|
| Paraclinic department staff (n = 40) | 32.0 ± 1.1 | 66.6 ± 1.9 | 1.64 ± 0.01 | 25.0 ± 0.7 | 93.1 ± 2 | 91.32 ± 10.9 | 2.08 ± 0.2 | 162.1 ± 5.6 |
| Intensive care unit staff (n = 21) | 34 ± 1.7 | 71.3 ± 2.7 | 1.69 ± 0.02 | 24.9 ± 1.01 | 91 ± 3.1 | 89.5 ± 23 | 1.95 ± 0.47 | 175 ± 7.2 |
| Hospital wards staff (n = 36) | 30 ± 1 | 68.5 ± 2.1 | 1.67 ± 0.01 | 24.2 ± 0.4 | 90.5 ± 2.8 | 116.4 ± 27.1 | 2.47 ± 0.56 | 155.7 ± 4.8 |
Abbreviation: BMI, body mass index.
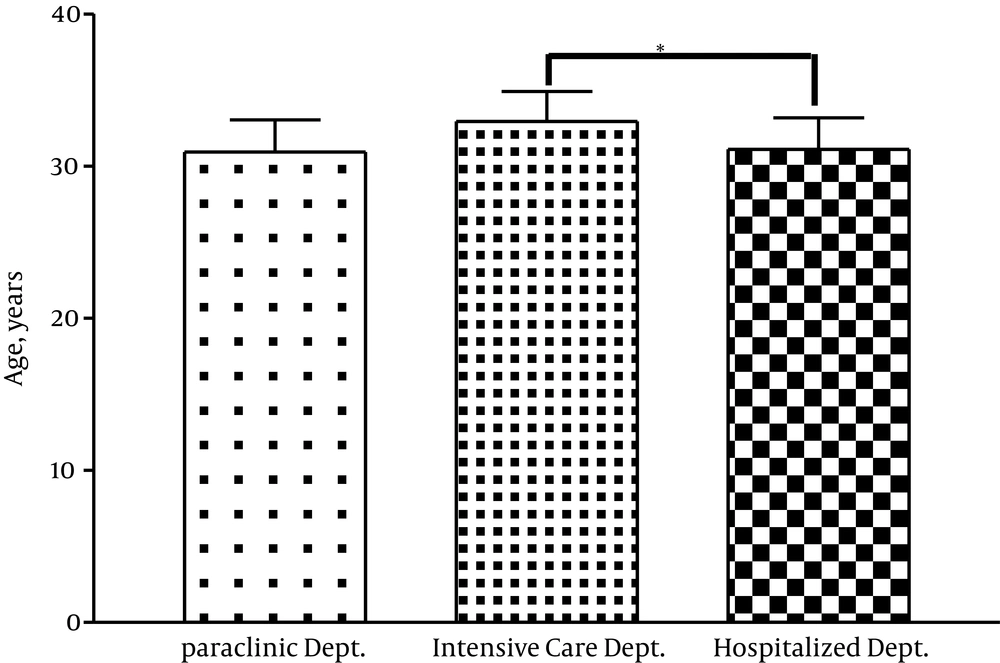
As indicated in Table 1, the staff of hospital wards was the youngest and those of ICU were the oldest ones. There was a significant difference between the staff of hospital wards and the ones in ICU regarding the age (P = 0.03) (Figure 1). There was no significant difference among the staff of different departments regarding BMI.
4.1. Serum Insulin and Glucose Concentration
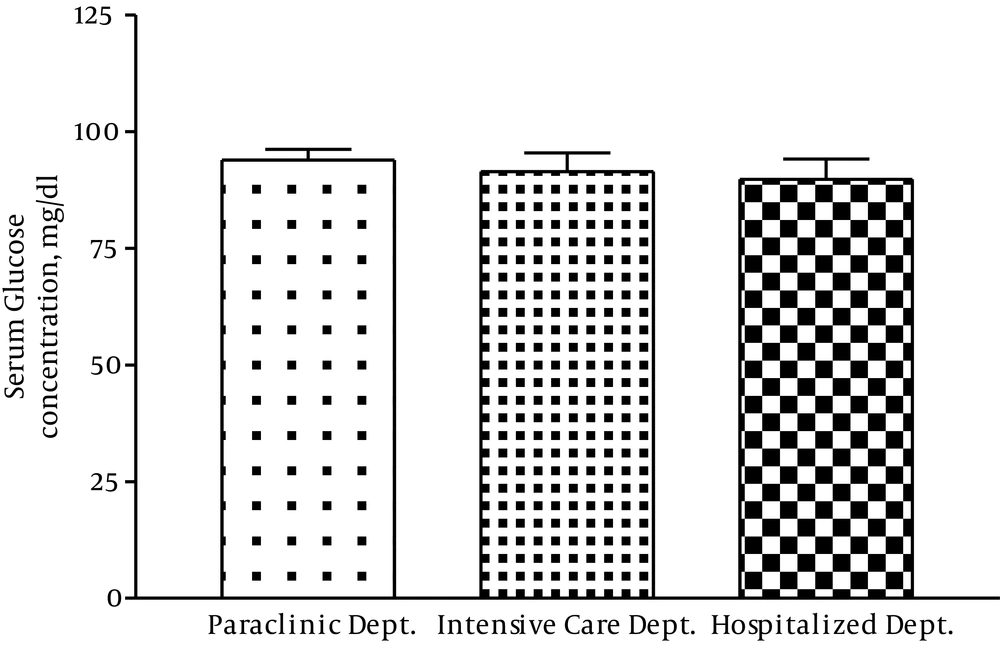
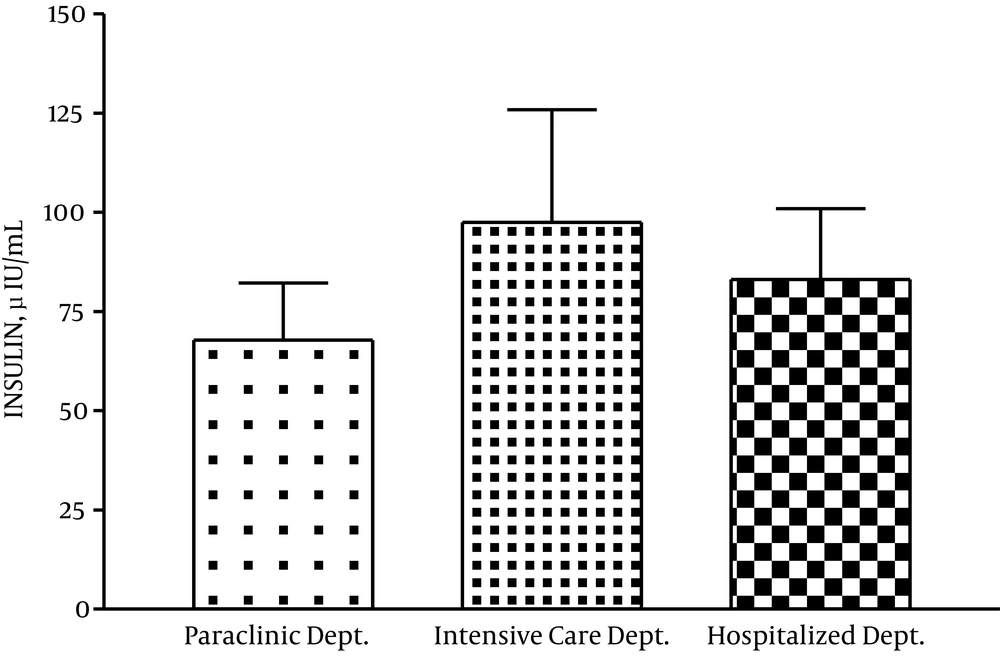
There was no significant difference regarding serum insulin and glucose concentration among the staff of different departments of the hospital (Figures 2 and 3).
4.2. Insulin Resistance
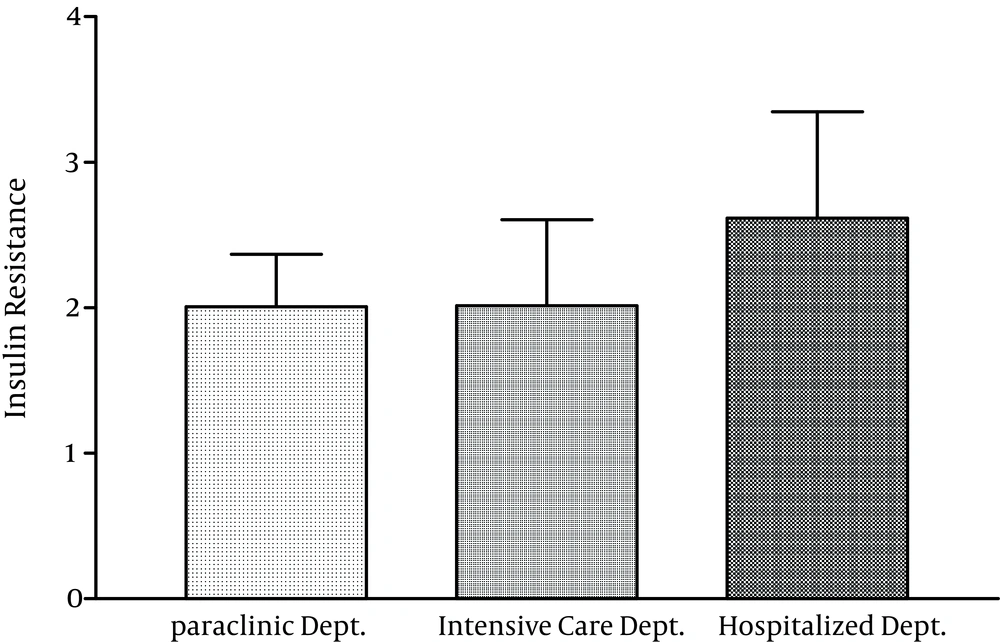
According to Figure 4, the staff of hospital wards and ICU showed the highest and lowest levels of insulin resistance respectively, but the difference between the rates was insignificant.
4.3. Occupational Stress Level
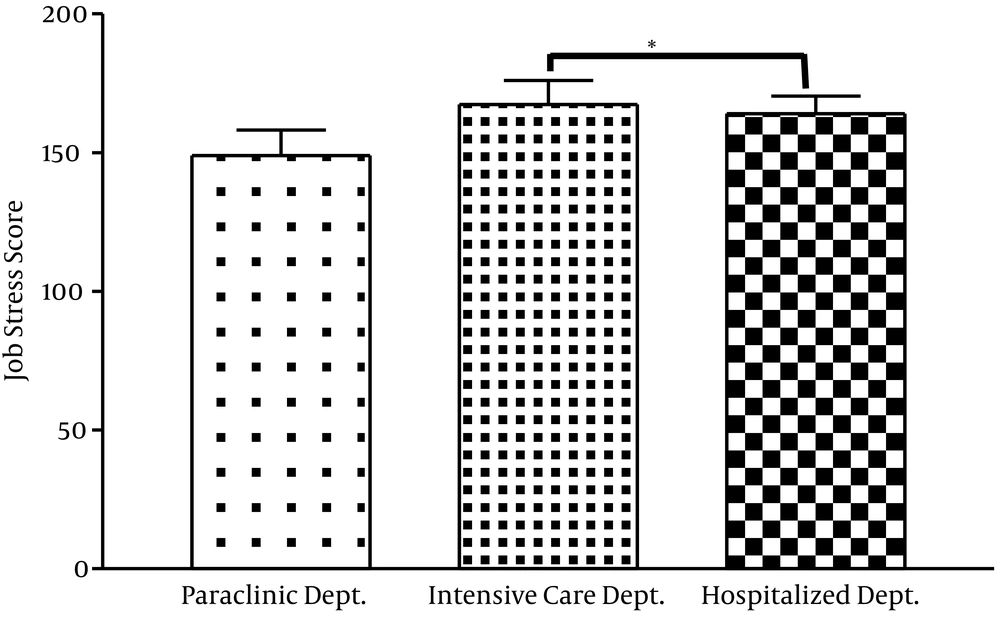
Comparing occupational stress scores among hospital staff showed that the level of job stress among the staff of ICU was significantly higher than those of the hospital wards (P = 0.035) (Figure 5).
4.4. Correlations
There was a significant positive correlation between the insulin resistance and age, but there was no significant correlation between insulin resistance with BMI and stress score.
| Insulin Resistance | ||
|---|---|---|
| r | P | |
| Age | 0.3 | 0.004 |
| BMI | 0.01 | 0.9 |
| Stress score | -0.09 | 0.3 |
Abbreviation: BMI, body mass index.
5. Discussion
Job stress adversely affects health at the individual level; it also negatively affects healthcare organizations and work output. At the individual level, stress is in association with metabolic syndrome and insulin resistance.
In the current study, there was no significant difference in insulin resistance among hospital departments, but there was a significant difference in age between the groups. Previous studies showed higher levels of insulin resistance in older people than younger ones and a positive relationship between age and insulin resistance (17, 18). Therefore, to study the effect of job stress on insulin resistance, age was considered as a confounding variable and ANCOVA was used to eliminate the effect of this factor. The results of ANCOVA as well as one-way ANOVA indicated no significant difference in insulin resistance between the three groups. Therefore, based on the results of the current study, insulin resistance does not depend on the working department, but it depends on the age.
However, in the current study, the relationship between age and insulin resistance was weak (r = 0. 3, P = 0.004). The study by Karakelides et al. on the older adults showed that age-related reductions in insulin sensitivity was due to an age-related increase in adiposity rather than a consequence of advanced chronological age (19).
In addition, another study showed that insulin sensitivity in males up to 60 - 70 years was more depends on body fat mass than age (20).
A few published studies evaluated the source and level of stress among healthcare staff (15, 21); according to the finding of these studies, the main source of stress was heavy workload and inadequate staff. However, to the authors’ best knowledge, the current study was the first study that compared insulin resistance and job stress level simultaneously among the staff of different hospital departments.
The results of the study showed that the staff of ICU, CCU and emergency ward experienced greater job stress than the other ones. This may not be surprising given that ICU and CCU staff usually faces high levels of stress at work, particularly due to the related clinical duties and death and that the ICU is especially stressful. Goodfellow et al. showed that ICU staff (physicians and nurses) exposed higher levels of stress than a normal working population (22).
In the current study, there was no correlation between insulin resistance and stress score. The study by Shiloah on 39 patients without diabetes and acute psychotic stress indicated an inverse correlation between β-cell function and insulin sensitivity with stress score (23). In another study, acute psychological stress (foot shock stress) in mice resulted in the elevation of blood glucose levels in both glucose tolerance and insulin tolerance tests (24). The difference may be due to the type of stress and the method used to estimate insulin resistance.
To assess insulin resistance in the subjects, hyperinsulinemic euglycemic clamp is the best technique, but it was costly, time-consuming and required more cooperation of hospital staff. Consequently, this method did not use, which was a limitation of the present study.
In spite of the current study, some previous studies reported a correlation between insulin resistance and BMI (25, 26). Trirogoff et al. reported that the primary determinant of insulin resistance in patients with chronic kidney disease (CKD) is BMI, specifically, fat mass. Another study on 132 patients with type 2 diabetes showed as BMI increased, the patients exhibited higher levels of insulin resistance and lower levels of insulin sensitivity. In this study glucose tolerance test was used to assess insulin resistance and insulin sensitivity indexes (25).
A longitudinal population-based cohort study showed that one standard deviation increase in rate of change in BMI corresponded to a decrease in insulin sensitivity by 19%; this study also quantified insulin sensitivity using a hyperinsulinemic euglycemic clamp (27).
The basis of this difference may be due to the study population and various methods used to estimate insulin resistance.
The current study had several limitations. First, there were small number of subjects in some departments and the cooperation of physicians was poor.
Low number of participants in the study results in low power of statistical analysis. The insulin resistance did not measure using the hyperinsulinemic euglycemic clamp. As previously mentioned, this is the best method to evaluate insulin resistance.
5.1. Conclusion
It seems that the staff of ICU is exposed to more job stress than other department staff, but there was no relationship between the job stress and insulin resistance among hospital staff. In addition, it is better to pay more attention to the age of the selected subjects working in CCU, ICU and emergency ward. However, further studies are needed to test job stress and insulin resistance in the other hospitals affiliated to AJA University to assess the correlation between job stress score and insulin resistance level.