1. Introduction
Immediately after the fall of Taliban in the winter of 2001, Indian Medical Mission (IMM), comprising of an anesthesiologist, a surgeon and a physician, were sent to the civil hospital in Mazar-e-Sharief to augment the depleted medical services. After Taliban were deposed by the U.S. invasion, health care delivery had been mainly through non-governmental organizations (NGOs), which were highly disorganized and interruptible. Afghanistan had some of the worst health indices in the world and ranked 173 out of 178 in the United Nations Human Development Index in 2004 (1). Many infectious diseases such as acute respiratory infections, diarrheal diseases, measles, and malaria contributed to the burden of disease. Malnutrition, physical trauma, psychological trauma, and human rights abuses are also significant problems in the country. There are many barriers to create an accessible, effective, and sustainable health care system in Afghanistan. Humanitarian assistance in surgery in rebuilding of a nation has a long history although no exclusive literature is available for anaesthesiology. The aim of this report was to describe the experience of a decade of practice of anaesthesiology in the rebuilding phase of post- war Afghanistan.
1.1. The Existing Anesthetic Practice at the Arrival of the Team
The 400- bed civil hospital of Mazar-e -Sharief is the tertiary care and teaching hospital to the Balk medical college, providing medical care to a population of 8 - 10 million. The hospital offers general surgery, obstetrics and gynecology, pediatrics, otolaryngology, ophthalmology, orthopedics, psychiatry and medicine as its major specialty care. Due to the long drawn civil war, the hospital lacked basic equipment and infrastructure when IMM was sent there; e.g., no casualty data, no operation theatre (OT), medical stores, and defibrillators. The entire hospital had only eight oxygen cylinders to begin with in 2001.
Practice of Anaesthesia in Northern Afghanistan was primitive as there were no qualified anesthesiologists in the country at that time. The technicians who had no knowledge of the subject administered anesthesia. There were no books in anesthesiology, and no curriculum for teaching anaesthesia as a subject. The concept of OT sterility, pre-anesthetic evaluation, intraoperative monitoring and postoperative care were primitive. The laboratory facility available was extremely unreliable. The commonest drug used was ketamine for all the patients irrespective of age, comorbid medical illness or surgical procedure. The on- table mortality in the operation theatre was said (not reported as no mortality data existed) to be quite high with one out of every four major surgery patient succumbing to death within 48 hours post-operation. The practice of regional anaesthesia was not present. Postoperative elective ventilation and intensive care facilities were almost non-existent. Moreover, there was an extreme degree of apathy towards anesthesia, and the doctors considered it below par. Furthermore, certain cultural and ethical constraints and misunderstandings had led to doctors not showing enthusiasm towards anaesthesia. In fact, most of the practicing anesthesiologists did not inspire confidence in fellow colleagues.
1.2. Equipment and Supplies
Problems related to equipment and supplies were multifaceted in procurement, distribution, inventory control and maintenance. There was complete lack of repair and maintenance facilities in Afghanistan. Most of the equipment were donated from various countries and had no facility for repair and services. Most of the anaesthesia ventilators had different pin index system since the machines were from Russia, and the oxygen cylinders were from the USA or European countries. Most of the sophisticated medical equipment was lying unused because of lack of knowledge of its function.
In view of almost nonexistent practice of anesthesia, certain general strategies were laid out to build up the practice of anesthesiology in Afghanistan, keeping the prevailing surgical practices, the socioeconomic conditions of the local doctors and the existing knowledge base.
1. Active effort was made to encourage and promote discussion and teaching of local medical personnel.
2. Attempt was made to inculcate the importance of resuscitation and fluid mgt, pre-op preparation and post- op care, regional anesthesia.
3. Change was initiated in OT set-up in areas of sterility, zonal concept and universal precautions.
4. An intensive care unit was set up in the long term after providing reasonable amount of training.
5. Inventories were established for equipment and drugs and for training the local staff on the maintenance of the equipments.
6. A teaching curriculum was developed at the civil hospital to provide formal training to the local Afghan doctors.
The prime advantage of the IMM was that it was perceived friendly in otherwise hostile country since cultural similarities paved the way for a cordial environment. There was also no great language barrier as most of the local doctors were well conversant with Urdu. The IMM doctors in due course learnt the local Dari language.
2. Methods
The initial data from December 2001 to May 2003 were not available in the Statistics Department of the Civil hospital of Mazar-e -Shrief. From May 2003 to May 2013, a total number of 22,856 patients were provided with anesthetic care in the operation room of the Indian medical mission, and more than 50,000 cases were provided with consultation. It was extremely difficult to go through the data, since the majority were written in Dari, which had to be translated into English, causing a delay in data analysis.
2.1. Equipment and supplies
The first team started its work in the winter of 2001 and initialized building the operation theatre, and three operation room assistants assisted them. Since being the only qualified anesthesiologist, he had to take over additional burden of running all the six OT’s apart from the Mission’s OT. This led to tremendous amount of frequent consultations in conducting surgeries in other operation theatres, which roughly went above 50,000 in the past ten years. However, it declined with time because the mission’s anesthesiologist extensively trained certain doctors selected by the hospital administration. At the end of the four years, 12 doctors were trained to conduct independent procedures in anaesthesia. By 2013, the mission had trained more than 60 doctors in anesthesia.
3. Results
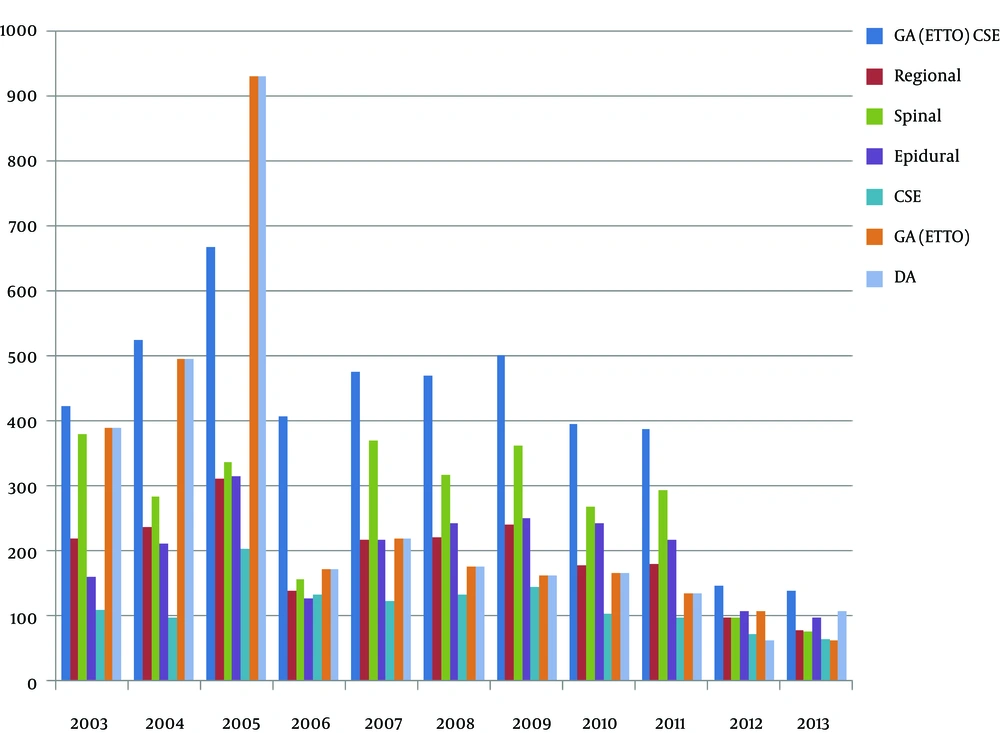
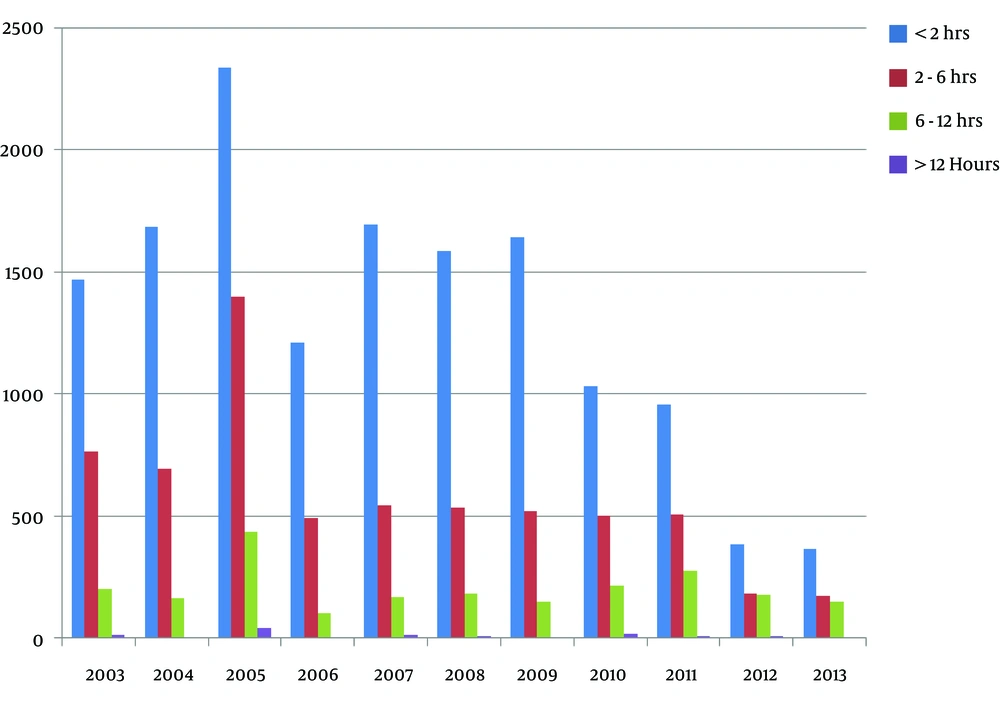
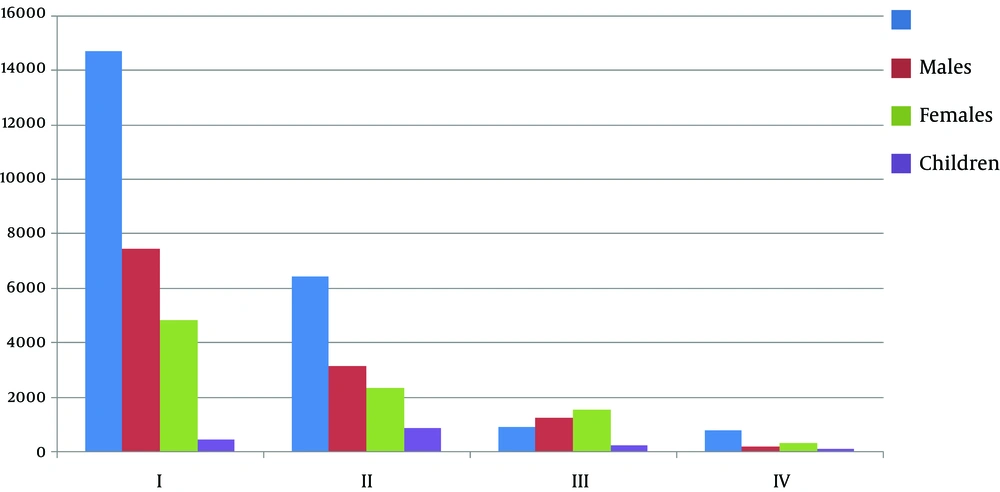
A total of 12,086 males (52.87%), 9,064 females (39.656%) and 1,706 children were administered anaesthesia. Among children, 1,104 were under the age of five (4.83%) while 602 were between 5 and 10 years of age (2.633%). Of all the techniques of anesthesia, general anesthesia (GA) with endotracheal intubation (ETTO) along with epidural analgesia (19.84%, n = 4535) was the most preferred, followed by GA with ETTO (13.19% n = 3025). Among the central neuraxial blocks, spinal analgesia was the commonest with 12.753% (n = 2915), and 9.54% (n = 2193) of the patients received epidural analgesia, which was the most common technique. Regional blocks were given to 9.28% (n = 2,123) of the patients (Figure 1). Predominantly, they were brachial plexus blocks. The cases done under local anesthesia have not been reflected here. The majority of the cases done were of a duration of less than two hours (62.4%, n = 14,356). Only 102 of 22,856 cases required more than 12 hours of anaesthesia. Of the cases, 39.1 % (n = 8,946) were administered anesthesia for emergency surgeries. Table 1 and Figure 2 display the demography and the anesthesia technique details. The majority of the anesthesia procedures done for the emergency cases were administered for polytrauma cases (65.5%, n = 5,864). Of the patients, 64% (n = 14,679) were classified as ASA I (American society of Anesthesiology Grading), 28% (n = 6,428) were ASA II, 4.1% (n = 946) were ASA III, and 3.5% (n = 803) were ASA grade IV patients (Figure 3). In the ASA I and II groups, 15.8% (n = 3,335) and in ASA III 42.8% (n = 405) had significant past history of one or more comorbidities. A total of 72,987 tests were ordered, of which 71,988 tests were carried out in the hospital or the private laboratory. An average of 3.15 tests per patient was ordered (range 1-8). Moreover, 15.67% (n = 3582) of the tests were abnormal. A greater number of test abnormality was found in ASA grade III (94%, n = 889) than ASA I and II (13.8%, n = 2913). A wide spectrum of surgeries was conducted in the Missions OT. The majority of the cases were trauma (37%, n = 8,342), followed closely by abdominal surgeries (32%, n = 7,299) Table 2 demonstrates the various surgeries conducted. There was no “on table death”, which was so common in Mazar hospital before the IMM was set up. A total of 3,868 complications were reported (errors might have been present in the reports of the first few years since the criteria were not well defined). Of the patients, 106 (02 children) died during the first 24 hours after surgery during the ten- year period, making it 0.87% mortality in first 24 hours. In fact, there was no reported death in first 24 hours after 2004. The 30- day mortality was 289 (17 children) at 2.3%, which is comparable to any tertiary care center results, considering the type of surgery, disease pathology and the preoperative nutrition status of the patients. Due to the frequent loss of follow-up of the patients, six- month survival rates were not calculated. The highly complicated cases were conducted in the OT of IMM in the past 10 years. A 10- bedded critical care unit, with two ICU ventilators and four multipara monitors were established in 2005, which unfortunately could not have still been expanded.
| Year | Male Patients | Female Patients | Children, y | Total | Regional Blocks | Spinal | Epidural | CSE | GA (ETTO) + CSE | GA (ETTO) | DA | Duration, h | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 - 4 | 5 - 10 | 2 | 2 - 6 | 6 - 12 | 12 | |||||||||||
| 2003 | 1162 | 1116 | 112 | 54 | 2444 | 220 | 380 | 160 | 110 | 422 | 390 | 390 | 1468 | 764 | 201 | 11 |
| 2004 | 1395 | 998 | 102 | 52 | 2547 | 236 | 284 | 212 | 98 | 524 | 496 | 496 | 1684 | 696 | 164 | 03 |
| 2005 | 1606 | 2171 | 144 | 88 | 4009 | 312 | 337 | 316 | 203 | 668 | 930 | 930 | 2334 | 1398 | 438 | 39 |
| 2006 | 1144 | 478 | 118 | 69 | 1809 | 138 | 157 | 128 | 133 | 408 | 172 | 172 | 1209 | 493 | 105 | 2 |
| 2007 | 1148 | 1112 | 96 | 56 | 2412 | 218 | 369 | 217 | 124 | 475 | 219 | 219 | 1691 | 542 | 169 | 10 |
| 2008 | 1060 | 1109 | 99 | 42 | 2310 | 222 | 318 | 243 | 134 | 469 | 176 | 176 | 1586 | 533 | 184 | 7 |
| 2009 | 1109 | 1108 | 103 | 61 | 2381 | 241 | 363 | 251 | 144 | 501 | 162 | 162 | 1642 | 522 | 149 | 2 |
| 2010 | 1351 | 268 | 96 | 48 | 1763 | 179 | 268 | 243 | 104 | 396 | 166 | 166 | 1032 | 503 | 214 | 14 |
| 2011 | 1196 | 394 | 92 | 44 | 1726 | 181 | 294 | 218 | 98 | 387 | 135 | 135 | 956 | 508 | 277 | 06 |
| 2012 | 476 | 166 | 68 | 46 | 756 | 98 | 76 | 108 | 72 | 147 | 107 | 62 | 386 | 184 | 178 | 06 |
| 2013 | 430 | 144 | 74 | 42 | 690 | 78 | 69 | 97 | 64 | 138 | 62 | 107 | 368 | 172 | 148 | 02 |
| Total | 12086 | 9064 | 1104 | 602 | 22856 | 2123 | 2915 | 2193 | 1284 | 4535 | 3015 | 3015 | 14356 | 6315 | 2227 | 102 |
| Year | Thoracic | Abdominal | OBG | ENT | EYE | Orthopedics | Reconstructive | Trauma |
|---|---|---|---|---|---|---|---|---|
| 2003 | 56 | 1063 | 312 | 51 | 18 | 116 | 64 | 684 |
| 2004 | 64 | 1094 | 366 | 56 | 21 | 112 | 108 | 1468 |
| 2005 | 108 | 1246 | 716 | 89 | 46 | 373 | 69 | 601 |
| 2006 | 66 | 753 | 412 | 37 | 17 | 91 | 46 | 772 |
| 2007 | 62 | 806 | 444 | 54 | 27 | 153 | 68 | 671 |
| 2008 | 53 | 621 | 296 | 42 | 28 | 147 | 64 | 673 |
| 2009 | 50 | 666 | 274 | 39 | 29 | 137 | 57 | 685 |
| 2010 | 54 | 784 | 253 | 38 | 25 | 123 | 56 | 666 |
| 2011 | 49 | 709 | 281 | 37 | 16 | 129 | 49 | 618 |
| 2012 | 32 | 204 | 193 | 27 | 12 | 72 | 32 | 237 |
| 2013 | 24 | 196 | 137 | 17 | 03 | 34 | 15 | 224 |
| Total | 618 | 8342 | 3684 | 487 | 212 | 1486 | 628 | 7299 |
4. Discussion
The contribution of anaesthesia services to reduce the burden of disease in an under-developed and developing countries is always under appreciated. It is always wrongly perceived that anesthesia services are only required in secondary and tertiary care centers. However, if available at the first referral center, anesthesia can significantly reduce death and disability because its role extends beyond the operation theatre in resuscitation, critical care facilities, pain relief as well as appropriate management of coexisting diseases.
Contini et al. (2), who used the WHO tool for situational analysis to assess emergency and essential surgical care, found severe deficiency in emergency surgical capacities and recommended comprehensive approach to strengthen it with certain urgency. They reported an abysmal low percentage of 27.2% certified anesthesiologists at peripheral health centers. The total number of anesthesiologists practicing in the Mazar civil hospital at the end of the mission was 18, and majority of them who received training went to private hospitals in Kabul or abroad. The ratio of anesthetists to surgeons at any given time was 1:7.5, which is much less compared to UK (1:1.25) and Canada (1:3) (3). What is further disturbing is that the basic package of health services released by Afghan Ministry of Public Health does not include the basic and essential surgical care among its seven major elements (4).
The number of surgical beds available was so small. Only 45 out of the 400 beds in the hospital were for surgical specialties. This was true for all the regions of Afghanistan (5). The scarcity of beds was further highlighted by the fact that Afghanistan, as a country, is always at war. Conditions for practice of anesthesiology, as per the laid down standards, were far from achievable. This made the task of conducting surgeries even more difficult.
Abnormal tests results for investigations were more frequent in the ASA III than in groups I and II, as expected, but past medical history did not influence the abnormality of the tests: 72% of the patients with past medical history in ASA II had normal laboratory findings. Although abnormalities were recorded in ASA I and II, which was 13.8% in our study, they have been reported to be much higher in few other studies (6).
Trauma remained the most common cause of morbidity in anesthesia facilities of IMM. Initially, it was war injuries and mine blast injuries, which used to dominate; however, the spectrum later shifted to road traffic accidents with certain peace returning. The blood bank facilities were primitive, with no availability of component therapy. As time passed and the knowledge of anaesthesia and surgical skills were passed on to the local doctors, the requirement of anesthesia services reduced. This was a good trend and only those cases, which had multiple comorbidities, were referred to the Indian anesthesiologist. We did not have the data of the anaesthesia provided by the local Afghan doctors in the operation theatre year- wise, as our request was not accepted. However, this decreasing trend indicated the reliability of anesthesia services provided by Afghan doctors, which was one of the prime aims of the Indian Medical Mission.
General anesthesia (with ETTO), combined with epidural analgesia, was the commonest technique used. This may be due to the fact the large number of cases were abdominal surgeries. In addition, many cases of trauma and reconstructive surgery received anaesthesia by this technique. We intend to publish the data of techniques of anaesthesia used in each specialty at a later date since presently it is out of the scope of this article. The commonest volatile used was Isoflurane. Halothane was the other volatile agent available and used extensively in the first two years. The availability of most of the narcotics, sedatives, muscle relaxants, inotropic drugs and other drugs used in anaesthesia and critical care were in adequate supply. There was no provision for nitrous oxide for the earlier team, but the supply of nitrous oxide improved from 2005 onwards. Oxygen was a great concern with the initial teams. However, slowly, the procurement and donations built up the 1246- liter cylinder stock to about 100. However, it was strongly recommended that a central oxygen pipeline system be installed for OT and the ICU. Most of the anaesthesia machines were donated by India, European countries, the United States and Japan. The autoclave facility was donated by Japanese government, which was very easy to operate and robust (Figures 4 - 6).
An interesting observation was that psychiatrists were treating head injuries prior to the arrival of the surgical team of IMM, despite the presence of the doctors from the Western countries, who had tirelessly tried to explain the importance of head injuries being treated by surgeons. It took many efforts to educate the doctors about the role of resuscitation and critical care support, especially in post-operative period.
The next nearest facility providing higher-grade medical care was in Kabul. Most of the superspecialist surgical facilities like cardio-thoracic surgery, neurosurgery, pediatrics surgery etc. were not available at Mazar, putting an immense pressure on the general surgeons to carry on the management, especially during the winter when the worlds’ highest highway “the Salang Pass” was blocked. This prompted for establishment of an effective evacuation system after stabilizing the patient. Since air was a costly mode of evacuation, seven hospital ambulances were modified by anesthesiologists in 2005 after equipping them sufficiently to carry out evacuation by road.
4.1. What is Further Required in Afghanistan?
4.1.1. Awareness of the Need
Recognition of the need for anaesthesia services at all levels of health care and its potential contribution to reducing mortality and morbidity is an important first step.
4.2. Policies and Legislation
In Afghanistan, the provision of anaesthesia services needs to be supported by policies and legislation that allow delivery of selective services by non-physician anaesthetists and mechanisms to achieve the United Nations Millennium Development Goals.
4.3. Education and Training
A multispectral approach for various levels of care is needed to address the inadequately trained and insufficient numbers of anaesthesia health providers. Short-term strategies should aim at improving the quality and quantity of mid-level providers for equitable access to primary health care in strengthening health systems. Task shifting or delegating anaesthesia services to non-physician anaesthesia providers will require the implementation of dedicated training programmes (7-9). Many developing countries have initiated task-shifting programmes to increase their capacity in providing anaesthesia and life-saving services, and this has resulted in an increase in the number of surgeries performed (Nepal), which is completely lacking in Afghanistan (7).
Long-term strategies should be targeted towards creating facilities for training physician anaesthetists for teaching and training, as well as providing specialized anaesthesia services for pediatrics, cardiac, neurosurgery, urology, plastic and transplantation surgery (8-10).
4.4. Policies for Retention
Appropriate environment should be provided in terms of well resourced, structured training, established posts in health facilities with adequate anaesthesia equipment, continuous professional development and financial remuneration that are consistent and comparable with other medical disciplines to reduce the brain drain of anesthesiologists from Afghanistan (9, 11).
4.5. Conclusions
The Indian Medical Mission was wrapped up in year 2014 after achieving some success in not only providing anaesthesia services to the population but also instilling a sense of pride and achievement in local anesthesiologists. The mission tried to revive the training and education part of its objectives.
There is not enough recognition of the need for anaesthesia services at all levels of the health system and their potential to reduce mortality and morbidity in Afghanistan. As a result, there is a serious lack of equitable services, especially in rural and remote areas. Creating awareness through better documentation of the burden of disease, appropriate policies, legislation, and the establishment of innovative and effective anaesthesia training programmes that address both the immediate need as well as the long-term needs of the health system (12) is the need of hour in Afghanistan. The Indian Medical Mission was able to make significant progress and contribution towards the growth of anaesthesia in Afghanistan.
4.6. Availability of Data and Material
Authors had no problem to readily reproduce materials described in the manuscript, including new software, databases and all relevant raw data, freely available to any scientist wishing to use them, without breaching participant confidentiality.