1. Background
Nowadays, oral health is a major element in general health state and shares several risk factors with other aspects of health (1, 2). Although adequate evidence is available for effective preventive measures for oral diseases, oral health achievement is still a main public health challenge.
Several oral and dental pathologies associate with chronic diseases including diabetes mellitus and cardiovascular diseases (3). Some studies demonstrate the relationship between poor oral hygiene and esophageal cancers (4, 5). In addition, oral and dental diseases stimulate substantial individual and public socio-economical influence. Of great importance, improvement in oral health and its impact on mental and physical health is among the major objectives of world health organization (WHO) for 2020 (2, 6, 7) and has substantial socio-economic impact on any given population.
The most recent studies estimated that the mean numbers of existing tooth in the Iranian group of 35 to 45 years olds were 21 to 21.7, while all tooth should be preserved in this age, according to the standard care (8). This aim has been attained in developed countries. However, the decayed, missing and filled teeth (DMFT) index is diverse in different countries. For instance, it is 16.3 in Lebanese 35 - 45 years old group (9), 22.8 in Brazil (10) and 16.61 in Australia (11) at the same age group. Another study showed that 7.7% of Danish population at 35 - 44 years old had healthy periodontium (12). Sanders et al. reported that dental missing increased with increasing age and associated with the people economic state (13). The DMFT index was related to healthy behavior, dental visits and income level in Australia (11) and France (14).
Available information about oral health in military forces is sparse but includes important messages. According to an American study, from 2711 recruitment nominees, 99.3% had oral health problems. In this study, 92.4% of 13050 active duty US military forces (in Army, Air Force and Navy) had oral health problems. Approximately a half of the employment nominees (49.1%) and 14.5% of the personnel needed emergency dental treatment (15). Another study in Spain on 387 Spanish Naval Force revealed only 7.2% healthy and inflammation-free periodontium (16). The DMFT index was 13.1 in 304 Croatian soldiers (17) and 8.96 (± 5.49) in Jordan Army. The later reported that 65.5% of the Jordanian Army did tooth brushing at least once a day (18).
There was no documented report about oral health in Iranian military forces except a local study on 341 air crew in the Iranian Air Force in 2008, which estimated the DMFT of 9.2 ± 5.1 (19). Unfortunately, no certified national document was available for military population in Iran. However, In Iranian civilian population, apart from divergent small studies with conflicting results and major sampling bias, there is only one national report by Hessari et al. (20).
2. Objectives
Lacking of valid data precludes appropriate planning and effective preventive strategies. Therefore, this study aimed to clarify the current situation of oral health in Iranian armed forces in order to find out potentials for oral health improvement for 2020.
3. Materials and Methods
This cross-sectional study was conducted based on a multistage (stratified random in clusters) sampling of 420 persons from 4 strata (Army, Air Force, Navy and Commander General headquarter) based on the total number of their staff. A WHO-certified standard questionnaire was used in this study, which was adjusted for military units and its validity and reliability were approved (21). All examiners were trained and evaluated for a standard examination and accurate data collection.
Beside DMFT and periodontal findings, the evaluated variables also included age, gender, education level, history of systemic diseases, knowledge and satisfaction of dental care, history of dental hygiene education, dental visits and oral health-related behaviors (such as brushing, smoking, using dental floss, alcohol use).
A community periodontal index (CPI) is described in 5 groups from CPI = 0 to CPI = 4 as follows:
CPI = 0, healthy and normal periodontium; CPI = 1, bleeding after probing; CPI = 2, calculus exist; CPI = 3, pocket depth between 3.5 and 5.5 mm; and CPI = 4, pocket depth more than 5.5 mm.
The frequencies were compared by chi-square and the mean values were evaluated by t-test and ANOVA. P < 0.05 was considered as the significance level.
4. Results
Four hundred and twenty male individuals were selected from 12 examination centers in Tehran, Iran, (6 in the GF, 3 in the AF, 1 in the NY and 2 in the CG) between 2011 and 2012. The samples consisted of 227 (54%) from Army, 90 (21.4%) from the Air Force, 47 (11.2%) from the Naval and submarine Force and 56 (13.3%) from the common general, in accordance to their proportion in our cluster.
The mean age of the participants was 34.76 (19 to 60) years old. There was a significant difference among the forces (GF = 33.13, AF = 35.72, NY = 39.66, CG = 35.71; P = 0.0001). Pairwise comparison between the forces showed a significant difference between NY with both GF (P = 0.001) and AF (P = 0.036). Since age was a determinant factor for the oral health indices, all findings were adjusted for age in this study.
Most of the individuals had no knowledge about the dental services covered by their insurance (60.5%) and only 3.8% of them had complete information about this issue. The level of knowledge about insurance-covered dental services was significantly higher in the CG personnel than the forces (P = 0.017).
Generally, 68.1% of the personnel were satisfied of the provided dental services. The commander general headquarters had significantly the highest and AF had the lowest satisfaction level (P = 0.041).
About 66% of the samples had never taken any oral hygiene education during their visits in dental services. Air Force had the lowest (27.8%) and CG had the highest rate (42.9%) of dental hygiene education; however, the difference between the strata was not significant.
Fortunately, 78.8% of the personnel did dental brushing at least once a day, but daily using dental floss was only reported in 31.4% of the individuals. There was no significant difference between the forces in this regard. According to self-reporting, 76% were nonsmokers, 1.9% ex-smokers and 22.1% smokers, with no particular diversity between the subgroups.
In the temporomandibular joint (TMJ) examination, 51 persons had TMJ problems including 15 (3.6%) deviation, 33 (7.9%) TMJ click, 2 (0.5%) trismus and 1 person (0.2%) opening limitation. The TMJ click were more frequent in the CG subgroup (P = 0.004).
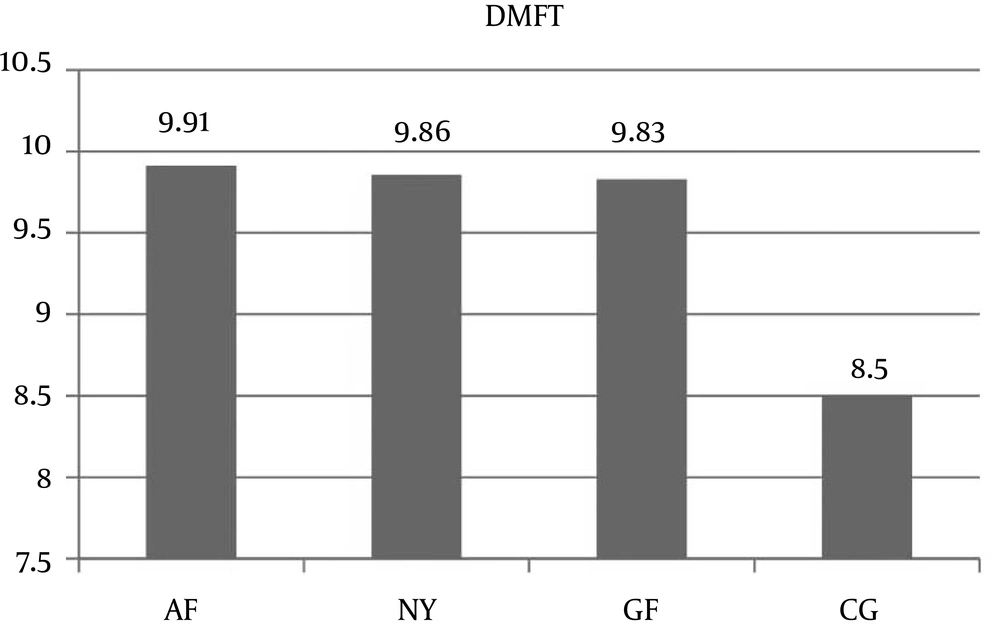
In this survey, DMFT was averagely 9.7±5.3 with no significant difference between the forces (GF = 9.8, AF = 9.9, NY = 9.8, CG = 8.5). From 420 examined personnel, 14 persons (3.3%) were caries-free, equally distributed in the subgroups. Furthermore, 92 individuals (21.9%) had root caries. The mean number of present teeth was 25.4 ± 3.265 (namely, GC = 25.7, AF = 25.4, NY = 23.7, CG = 25.7). The NY figure was significantly lower than other groups in this term (P=0.009). The minimum teeth number was 15 in GF, 9 in AF, 2 in NY and 15 in CG (Figure 1).
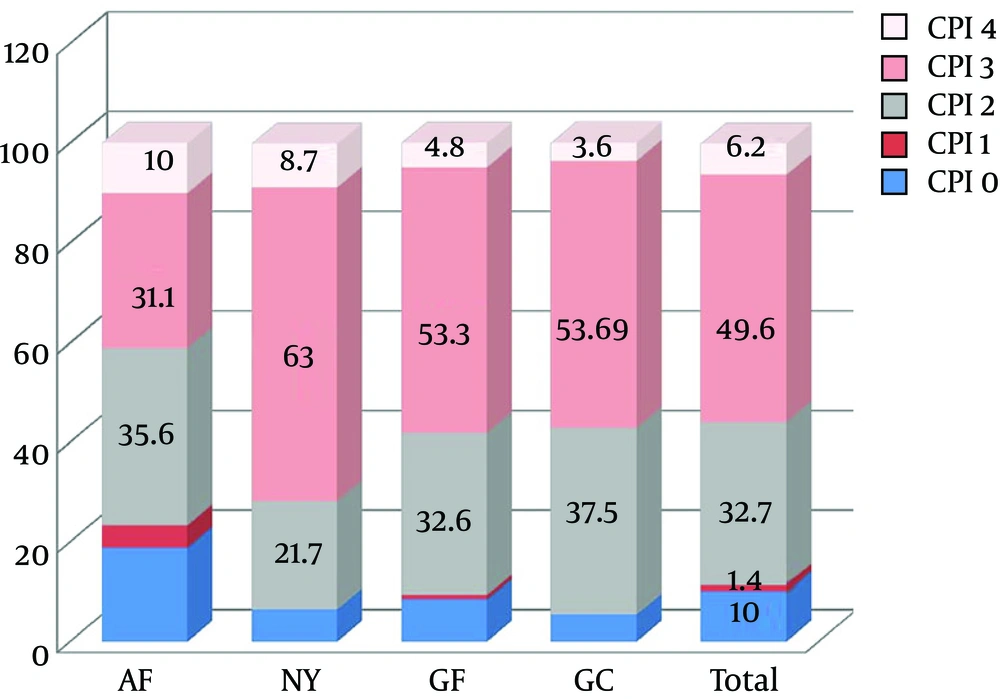
Totally 2520 sextants were examined, of which 1079 sextants (42.81%) had CPI=0, 71 sextants (2.18%) had CPI = 1, 741 sextants (29.40%) had CPI = 2, 495 sextants (19.64%) had CPI = 3, 39 sextants (1.54%) had CPI = 4 and 94 sextants (3.73%) could not be examined due to missing teeth.
A community periodontal Index was also recorded for individuals that illustrated CPI=0 (satisfactory periodontal state) in 10%, CPI = 1 in 1.4%, CPI = 2 in 32.7%, CPI = 3 in 49.6% and CPI = 4 in 6.2% of the cases. The frequency of pockets > 5.5 mm was greater in the AF and NY (Figure 2).
The AF subgroup had the greater rate of gingival bleeding in all sextants (P < 0.05). From individual perspective, the greatest bleeding rate after probing was seen in persons from the AF group (52.5%, P = 0.001).
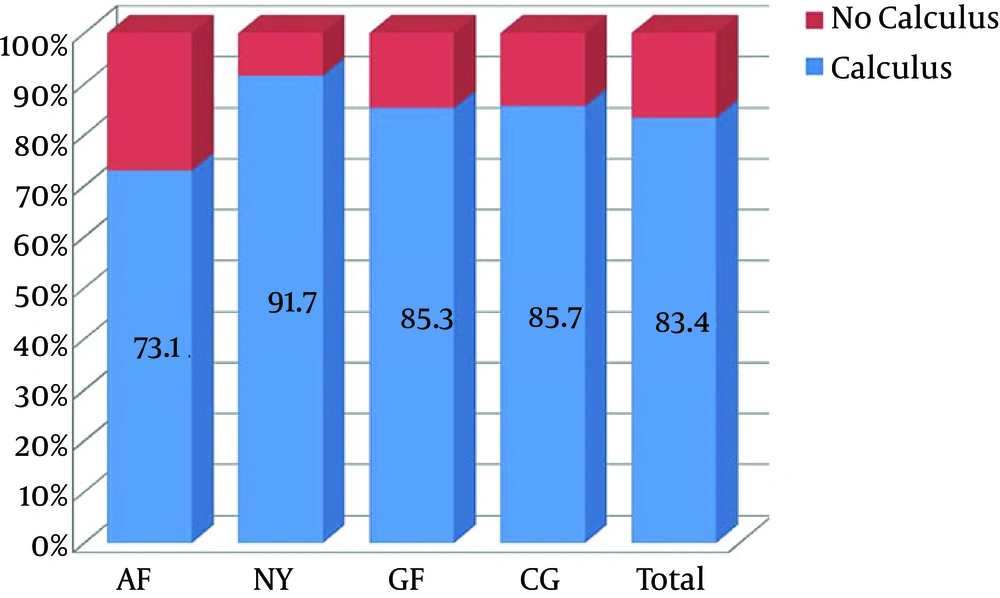
The frequency of calculus was significantly higher in the NY than other subgroups (P = 0.036). Within the NY subgroup, calculus was more frequent in the middle (upper and lower) sextants and the right lower sextants (P < 0.05) (Figure 3).
There was a statistically significant inverse relationship between the education level with DMFT (P = 0.049) and the frequency of root caries (P = 0.0001).
The worse DMFT (11.29) was recorded in smokers which was significantly different from nonsmokers (P = 0.004), independent of age. There was a significant correlation between frequency of sweet snack intake and DMFT (P = 0.06), with the highest DMFT in the person who took 4 or more times sweet snack.
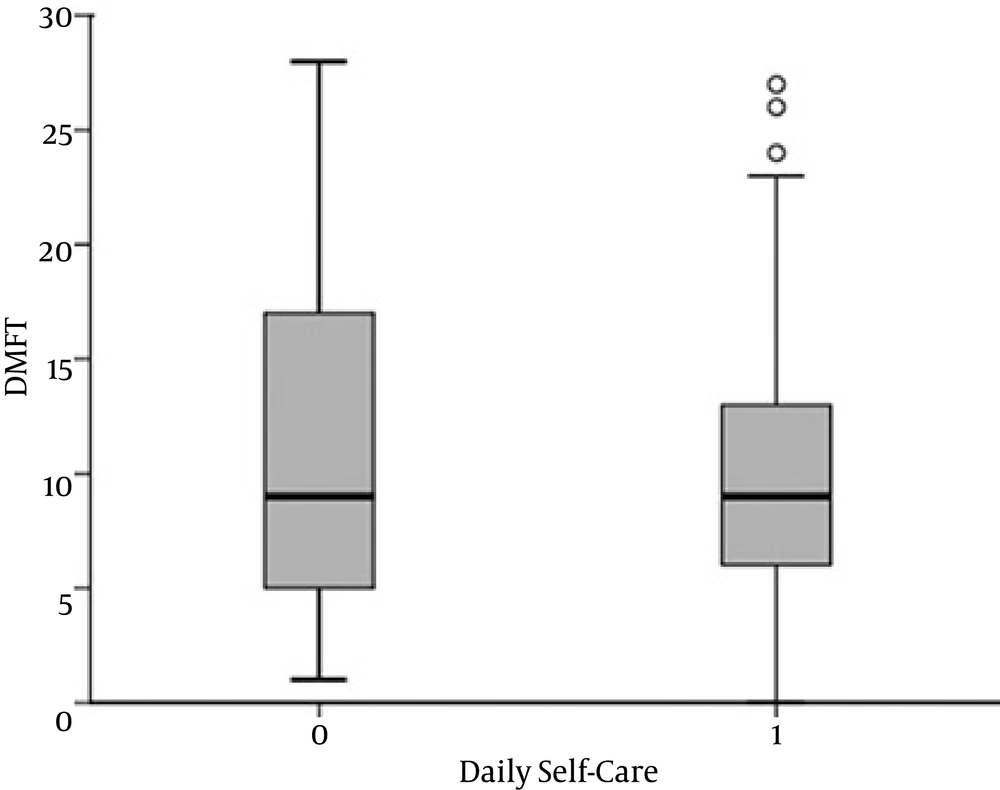
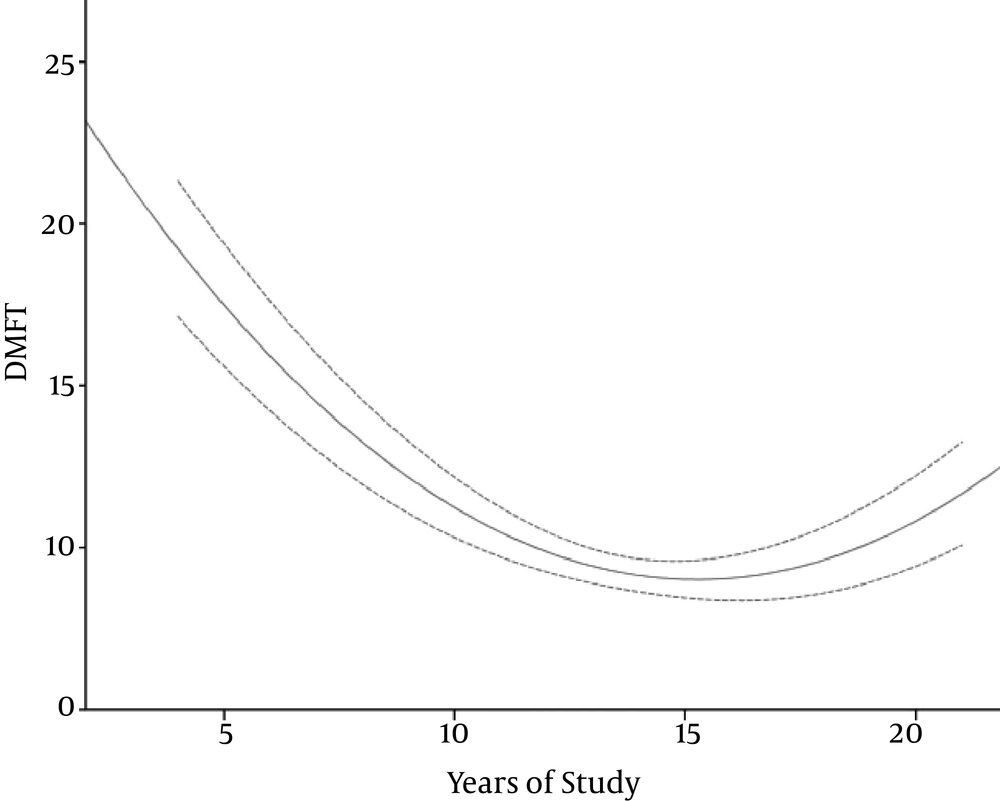
Although DMFT in the person who regularly did brushing or used floss was 2 unit better than the person who did not use brush or floss, the difference was not statically significant (P = 0.08) (Figure 4). Education had a nonlinear relationship with DMFT and permanent teeth, which indicates that the oral health literacy is not satisfactory even in the so-called educated group (Figure 5).
Of paramount importance, DMFT was 3.5 units greater in patients with a history of cardiovascular disease than other persons (P = 0.014). Using multivariate analysis with ANCOVA, it was revealed that this relationship was independent of age (P = 0.01). Although similar finding was observed as greater DMFT in diabetic patients than nondiabetics, it was not reached to the significance level (P = 0.07) (Table 1).
| Indices | Total | GF | AF | NY | CG | P Value |
|---|---|---|---|---|---|---|
| Mean age, y | 34.76 | 33.13 | 35.72 | 39.66a | 35.71 | 0.0001 |
| Education, y | 13.75 | 13.61 | 14.26 | 12.91 | 14.20 | 0.007 |
| Years in Services | 14.54 | 13.49 | 16.17 | 16.70b | 14.39 | 0.009 |
| Satisfaction of Last Dental Service | 68.1 | 70.2 | 57 | 66 | 78.6c | 0.041 |
| Never Trained about Oral hygiene | 34 | 33 | 27.8 | 40.4 | 42.9 | 0.215 |
| History of Head and Neck Trauma | 24 | 26 | 18.9 | 23.4 | 25 | 0.602 |
| No Knowledge about dental insurance | 60.5 | 64.3 | 62.2 | 66.0 | 37.5d | 0.017 |
| TMJ Click | 7.9 | 6.2 | 1.1 | 12.8 | 21.4d | 0.004 |
| Gingival bleeding | 38 | 38.9 | 52.6d | 25 | 20.4 | 0,001 |
| Dental calculus | 83.4 | 85.3 | 73.1 | 91.7d | 85.7 | 0.036 |
| Pocket depth ≥ 5.5 mm | 31.6 | 26.7 | 38.9 | 40.4d | 26.7 | 0.002 |
| DMFT | 9.67 | 9.82 | 9.91 | 9.84 | 8.50 | 0.33 |
| Caries free | 3.3 | 4.4 | 1.1 | 4.3 | 1.8 | 0.435 |
Abbreviations: AF, Air Force; CG, commander general headquarters; DMFT, decayed, missing and filled teeth; GF, Ground Force; NY, naval and submarine; TMJ, temporomandibular joint.
aNY vs. AF P = 0.036, NY vs GF P = 0.001.
bNY vs. GF P = 0.009.
cCG vs. AF P = 0.041.
dDifferent from all other groups, P < 0.05.
5. Discussion
In this study, the oral health profile (including DMFT and periodontal health state) of a randomly selected group of Iranian armed force was estimated. The estimated DMFT was 9.67 (from 9.42 to 9.92 with 95% CI) in this study, which was higher than estimated DMFT values in Malaysian (22) and Jordanian (18) armed forces (8.15 and 8.96, respectively).
In this study, about 10% of the examined persons had noninflamed healthy periodontal tissue which is a better figure than that of Spanish Armed Force (7.2%) (16), but the depth of pockets was more in our study compared to the mentioned study which refers to more need of oral health education in Iran. In a Croatian study (17), the mean normal sextant for each person was 2.1 while in our study it was 2.56.
Comparing Iranian Armed Force with civil population aged 35 - 45 in this country, as reported by Pakshir et al. in 2004, showed a better DMFT index (9.67) in the Armed Force compared to civilians (14.83) (8). Similarly, it was better than the findings by Torabi who reported a mean DMFT of 10.88 (23). The DMFT index was 11.0 ± 4.6 in another population-based study by Hessari in 2007 among 8301 civilians (20). In their study, the mean number of existing teeth was 21.6 which was markedly lower than the findings (25.6) of the present study. Hessari reported in their study 1%, 40%, 43%, and 10% for CPI from 0 to 4, respectively (20). All those indices were worse than those of the current study. The above-mentioned dominancy in oral health indices in the Armed Force compared to civilians may be due to the availability of insurance-covered dental services for military forces. However, most of the military personnel were unaware of the available dental services. It is assumable that this knowledge is even worse out of the capital city. Furthermore, 66% of the individuals had no oral health education in their visits at all. Then more effective educational program is required in this population which would lead to a model for oral health in our country. Perhaps, given the limited time for dentists, dental hygienists would have a major role in this regard.
The result of the current study showed that 78.8% of the personnel used dental brushing regularly and 31.4% regularly used dental floss, which is prominently better than 66.8% and 5.8%, respectively, for their civilian counterparts as reported by Torabi (23). This is in parallel to the better DMFT in the armed force compared to civilians. On the other hand, the DMFT index was associated with consumption of sweet snack and smoking. Therefore, health promotion would play a major role in controlling the risk factors.
Although DMFT was averagely worse in diabetic patients than nondiabetic individuals in this study, a significant level of difference was not proved due to the small number of diabetics (n = 13) which reduced the power of the statistical tests. Nevertheless, the relationship between cardiovascular diseases and DMFT was quite significant, which was independent of age. This interesting finding cannot show a cause and effect relationship. In other words, worse oral hygiene would stimulate cardiovascular diseases but it could also be considered that the medication which is used by patients with cardiovascular diseases can cause a worse oral health due to xerostomia. Similarly for diabetes, the more drive for sweet diet or drinks may result in dental caries. Therefore, longitudinal studies are required for more accurate investigation of these relationships.
5.1. Conclusions
In conclusion, although oral health profile was better in the Iranian Armed Force compared to their civilian counterparts, there are several potentials for improvement, as some international military forces attained. Of course, oral health education, preventive modalities, removing calculus, giving more information about dental services and health insurance, constructing a leveled shared network of dental services in the armed force, regular oral visits and taking the role of dental hygienist into account, play major roles in oral health improvement among armed forces.