1. Background
Cancer is a leading cause of mortality worldwide and according to the 2015 world health statistics, more than 8.8 million global deaths in 2015 were attributed to cancer (1). The world health organization (WHO) estimates that 19% of all cancers are attributed to environmental factors, accounting for more than 1.5 million deaths annually (2, 3).
More than 900 agents have been categorized as potential cancer risk factors of which several factors relate to occupations (2). Particularly, military occupations yield several cancer risk factors including carcinogenic agents, nutritional factors, and psychological promoters that are theoretically avoidable and could be partially controlled. Possible deployment-related exposures have been documented by the US department of defense including industrial solvents, jet fuels, air pollution, and radiation. Moreover, Diluted Uranium, vaccination side effects, behavioral changes during deployment such as tobacco use have also been suggested as occupational cancer risk factors in military employees (4-7).
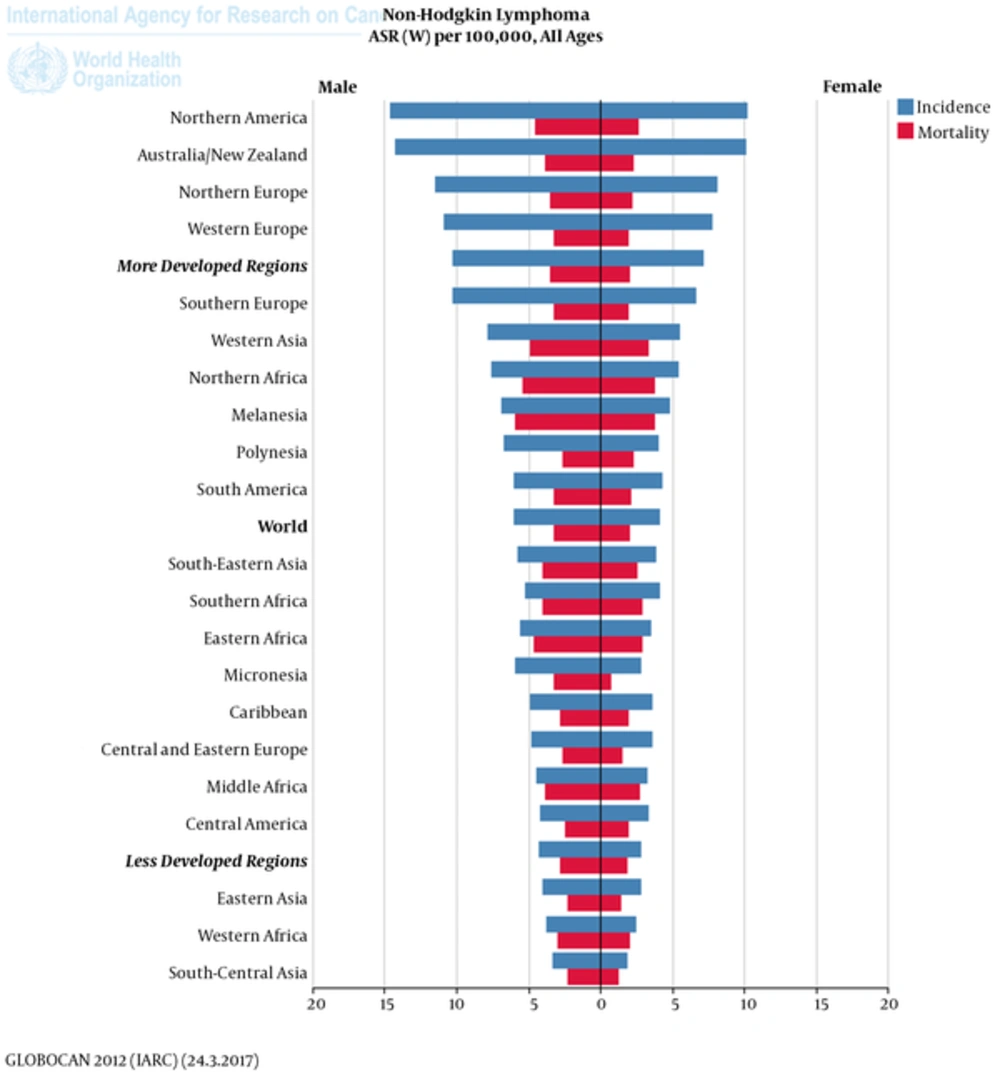
Malignant lymphocytic transformation would originate from B or T cells and is a major cause of painless lymphadenopathy. NHL is the most prevalent hematopoietic neoplasm representing approximately 4% of all cancer diagnoses and ranking seventh in frequency among all cancers. NHL is more than 5 times as common as Hodgkin disease. The median age at presentation for most subtypes of NHL is older than 50 years. The exceptions are high-grade lymphoblastic and small non-cleaved lymphomas which are the most common types of NHL observed in children and young adults (8). Based on a systematic review, 666,000 (95% UI, 584,000 – 710,000) incident cases of NHL and 231,000 (95%UI, 196,000 - 244,000) deaths have been reported in 2015. Non-Hodgkin lymphoma caused 6.3 million (95% UI, 5.4 - 6.6 million) DALYs in 2015, 95% coming from YLLs and 5% from YLDs (9). Although new diagnosed cases of NHL increased by 56% from 2005 to 2015 (9), no significant change in the rate of NHL has been detected in a systematic analysis of the cancer statistics from 1980 to 2015 (10).
At diagnosis, low-grade lymphomas account for 37% of NHLs in patients aged 35 to 64 years and account for 16% of cases in patients younger than 35 years (8, 11). As a result, determining the high risk groups and early diagnosis, in particular in military forces, would lead to a better prognosis of patients. While there are only a few scientific reports about the cancer rate in armed forces, NHL is among the main neoplastic diseases in military population (2, 4, 12). However, the information about the role of military jobs on the incidence of NHL is contradictory (2, 4-6, 13). This study aims to evaluate the potential role of military jobs on NHL in a case-control research.
2. Methods
In this case control study, the minimum required sample size for the case group was estimated as 150 with 300 controls. Therefore, respecting inclusion and exclusion criteria from various neoplastic patients from 2006 to 2008, all pathologically proven cases with NHL (n = 185) from three main referral oncology centers in Tehran (Imam Reza, Shariati and Imam Khomeini) were taken as cases and 315 age group-matched individuals without any oncologic disease were selected via a stratified systematic random sampling as controls from the same centers.
Inclusion criteria were: being pathologically proven of a type of NHL, age older than 20, having ICD-based standard record in the hospital health information system, being available for interview (in presence or by phone). The exclusion criteria were comorbidity with another cancer, congenital autoimmune diseases, and non-compliance.
Data gathering was performed based on a check list of potential risk factors both from the hospital records and complementary interview with the individuals. The study was approved by the University ethics committee and an informed consent was taken from each person during their interview.
3. Results
Descriptive statistics of 500 included subjects in the study demonstrated that male to female ratio was 1.47 in the patients and 1.84 in the control group (P = 0.24). There was no significant difference between the groups regarding their age.
In the whole study population, 171 individuals (34.2%) had a military occupation. However, there was no significant impact of military jobs on the incidence of NHL (P = 0.95). Family history, past medical history of hospital admission, smoking and addiction, and radiation history had a significant association with NHL incidence. In contrast, no significant relationship was observed between the history of inflammatory or autoimmune diseases and NHL. Viral or helicobacter infections were also associated with NHL (Table 1). No history was expressed for exposure to asbestos, Arsenic, wood dust, agricultural toxic agents or administration of digoxin and phenytoin or a history of congenital immune deficiency. The exposure to benzene could not be assessed properly (Figure 1).
| Variable | Case (n = 185) | Control (n = 315) | OR (95% CI) | P Value |
|---|---|---|---|---|
| Gender | 0.80 (0.55 - 1.16) | 0.24 | ||
| Male | 110 (59.5) | 204 (64.8) | ||
| Females | 75 (40.5) | 111 (35.2) | ||
| Occupation | 0.95 (0.65 - 1.40) | 0.80 | ||
| Military | 62 (33.5) | 109 (34.6) | ||
| Civil | 123 (66.5) | 206 (65.4) | ||
| Family history | 15 (8.1) | 7 (2.2) | 3.88 (1.55 - 9.71) | 0.002 |
| Past Hospital Admission | 106 (57.3) | 78 (24.8) | 4.07 (2.77 - 6.01) | 0.0001 |
| Viral infection or Helicobacter infection historya | 4 (2.2) | 0 | 15.64 (10.44 - 20.84) | 0.009 |
| Autoimmune disease historyb | 4 (2.2) | 5 (1.6) | 1.37 (0.36 - 5.17) | 0.64 |
| Smoking and addiction history | 30 (16.2) | 13 (4.1) | 4.49 (2.28 - 8.86) | 0.0001 |
Assessment of Potential Risk Factors for NHL
4. Discussion
In this study we did not find any evidence for a relationship between military occupations and NHL. Similarly, the odd of history of autoimmune diseases was not greater in the case group when compared to their controls. Instead, family history, past medical illness requiring hospital admissions, and risky behaviors such as smoking and addiction as well as viral infection or infection with Helicobacter pylori had significant associations with NHL.
Military population may differ from general population in various terms including exposure to particular risk factors, environmental contaminators, sunlight exposure, smoking and alcohol in one hand and better physical fitness, free access to medical care, and regular screening on the other hand (9). Military forces are also exposed to several hazards during deployment such as local industry pollutant, indigenous ambient particulate matter, exhaust from military vehicles, machinery and generators, open air burn pit emissions and fumes from fires, munitions and weapons, depleted uranium and radiation (2). Therefore, a different cancer incidence would be expected in military community.
The issue of the potential relationship between military jobs with cancer was mainly raised by self-reported cancer claims by the Vietnam War Veterans. The military health professions warned the public that the troops were exposed to several environmental contaminants in Vietnam of which the contaminated herbicidal named as “Agent Orange” with an extremely toxin dioxin was on the first line of the potential risk factors for post-deployment poor health (2). While the results of the studies about this relationship were contradictory, accumulating evidence was summarized by the Institute of Medicine in “Veterans and Agent Orange: Update 2012” report which demonstrated that there is sufficient evidence for an association between soft tissue sarcomas, NHL, chronic lymphocytic leukemia and limited evidence for an association with laryngeal, lung, bronchus, trachea and prostate cancer as well as multiple myeloma (2, 4, 14). It was concluded that the deployed troops who were exposed to the contaminated herbicide during 1965 to 1972 experienced a higher cancer incidence, whereas other deployed forces were not at a greater risk for cancer.
Following the 1991 Gulf War, an increased rate of post-deployment of some cancers (such as brain or testicular) was reported which was attributed to depleted uranium, petroleum products, hydrazine, pesticides, combustion products as well as chemical and biological warfare agents (2). Depleted uranium was firstly used on battlefields during the Gulf War in 1991 followed by the war in Bosnia and Herzegovina in 1995 during operation Balkan Strom in Kosovo in 1999 and then in Iraq in 2003 (6). It is possibly in use on the hybrid conflicts in Iraq, Syria, Yemen, Lebanon, Libya, Afghanistan and even some parts of Turkey and might be abused by the so called ISIS forces; though no formal document has been released in the regard. Meanwhile, several reports of post-deployment cancer have been reported including Italian troops involved in peace-keeping missions in Bosnia and Kosovo and American veterans who took part in the Gulf War (2, 4, 6). It was concluded that depleted uranium might contribute to the excess risk of cancer in the troops. However, real exposure to uranium was not confirmed. Furthermore, the comparison of 40,000 soldiers reveals rates lower than expected for cancer in males 20 to 59 years of age in Italy, except for Hodgkin lymphoma (6). However, there are still several unknown issues about depleted uranium including the soil and material remnants, contaminated dust distribution pattern, its pathologic effects, and the ways of decontamination and protection. Moreover, the psychological concerns about the threat of depleted uranium for military forces and local population is of greater importance that the previous exposure itself (13).
Given the use of chemical and radioactive weapons by Iraq against Iranian military forces during the war (1980 to 1988), the frequent dust storm in the war region and the proposed latent period, we investigated the potential association of military occupations with NHL about 20 years after the war. We did not find any evidence of the relationship between military jobs and NHL. Instead, general risk factors contributed to the NHL incidence. Our results contradict a study in US military veterans about NHL. In this study, analyses of 1,157 men with pathologically confirmed lymphomas and 1,776 control subjects showed that the risk of non-Hodgkin's lymphoma was approximately 50% higher among Vietnam veterans (odds ratio, 1.47; 95% confidence interval, 1.1 to 2.0) compared with men who did not serve in Vietnam (15). However, our findings are in parallel to the previous studies on multiple cancer incidences in military personnel. A comparison of the cancer incidence in US military population consisting of 14-year data from automated central tumor registry (ACTUR) with a national civil registry (SEER) demonstrated a lower cancer rate in military population except for prostate cancer and breast cancer. The later was mainly attributed to better diagnosis as a result of free access to health care and screening program (4). Recent studies about the possible association of battlefield environmental exposure and cancer diagnosis include an investigation by the US Army public health command which studies several neoplastic outcomes among formerly deployed service members to Karshi-Khanabad, an air base in southeastern Uzbekistan used to support missions in Afghanistan from 2001 to 2005 (2). Exposure to asbestos and radioactive and fuel material, dust and particulate matter was determined in the air base. After a 10-year follow-up, only age-adjusted rate of malignant melanoma and neoplasm of lymphatic and hematopoietic tissue (excluding NHL and leukemia) were greater than the control group (deployed troops to Korea) (RR = 3.2 and 5.6 respectively) (2). Finally, while previous exposure of some US Army Veterans to Adenovirus vaccine which was contaminated with Simian Virus 40 was supposed to have a role in cancer, evaluation of 181 brain cancers, 220 NHL, 10 mesothelioma did not provide any evidence for this relationship (5).
NHL in particular is not very infrequent in military units. Non-Hodgkin's lymphomas are one of the most commonly occurring cancers in the age groups heavily represented in the U.S. Navy (16). Assessment of the first 5,000 histologically confirmed malignancies at the Riyadh Armed Forces demonstrated that lymphoma was the second most frequent malignancy at 13% (after gastrointestinal cancers with 18% frequency) with 2.5:1 ratio of non-Hodgkin lymphoma to Hodgkin disease. In both groups, poor prognostic histological varieties were more frequent than in the West (12). While the information about the NHL incidence in military forces is diminutive, it seems that NHL frequency is not greater than that in the general population when a better diagnosis and free access to medical facilities are taken into account. However, risky behaviors and psychological consequences after the deployment would enhance the risk.
4.1. Conclusions
We found no evidence of the association of military occupations with NHL. Instead, conventional risk factors accounted for the NHL diagnosis which could be avoided or controlled by early diagnosis in high risk individuals in military forces.
4.2. Limitations
Our study had some limitations and potential biases that were mainly originated in the case-control design of the research. Perhaps, long term prospective studies with precise recording of the risk factors would yield more valid results.