1. Background
Blastocystis sp. is one of the most important inhabitant protozoans in the large intestine of humans (patients with gastrointestinal symptoms, and healthy individuals). It is a polymorphic parasite whose size varies from 5 µ to 150 µ. In 1912, it was introduced as an inoffensive parasite; afterwards, studies showed that it was a commensal protozoan of the intestine, but according to the last categorization, it was situated in the stramenopiles group and fecal-oralisits main route of transmission (1-4). Blastocystis sp. has a global spread-out and it has been one of the most common parasites in parasitological assessments. The prevalence of this parasite in different areas of the world varies from 0.5% to 23% and possibly more in developing countries. The prevalence of this parasite has been reported, in Khorramabad 6.5%, in Tabriz as 17.26%, and in Tehran cities as 6.5% and 12.8% (5-8). The pathogenicity of this parasite is extremely important, especially in people with immunodeficiency. Some of the pathological and immunological studies demonstrate some pathogenicity; however, no intestinal symptoms were found. The role of Blastocystis as a pathogen is more significant. Healthy carriers play an important role in the transmission of disease.
The prevalence of Blastocystis is closely associated to the epidemiological and hygienic situation of the district. Deployed troops and other crowded populations due to the low quality of sanitary conditions are at risk. According to a Thai study, prevalence of Blastocystis sp. carriage in Thai army personnel was reported 44% based on smear test and formalin/ethyl acetate concentration techniques (9).
In recent years, military conflicts in tropical and subtropical areas could be related with risk for gastrointestinal protozoan infections, especially Blastocystis. In another study, prevalence of Blastocystis sp. was 15% in military personnel who participate in the Iraq and Afghanistan war (10). Moreover Diarrhea caused by intestinal parasites, including B. hominis, leads to the inability of army personnel and, consequently, reduced combat power of military forces in operations and maneuvers (11).
Most infections are asymptomatic; however, in some cases, maybe demonstrate signs such as: anorexia, fever, vomiting, abdominal pain, and diarrhea (4, 12-14).
2. Objectives
Considering the slightly high prevalence of Blastocystis sp. in examined cases at parasitology laboratories and attributing many pathological signs to the above-mentioned protozoan in the recent years, and since no study has been conducted in Alborz province, the aim of the present study was to assess the prevalence rate of this parasite in cases referred to central laboratories of Alborz province during 2014 - 2015.
3. Methods
The current descriptive cross-sectional study with random sampling was carried out on cases referred to central laboratories of Alborz province during 2014 - 2015. The patients were asked to fill a questionnaire on their demographic characteristics. From each case, three stool samples were collected and accumulated in a plastic dish.
Some information consists of age and gender; symptoms of the present illness and date were recorded by filling a survey questionnaire by patients. The informed consent for participation in the study was obtained from each participant. Then, the samples were microscopically evaluated using normal saline and iodine solution preparations and formalin-ether procedure. Formalin-ether method was performed by parasite test kits. A 3.5 mL parasite test solution (formalin 10% + normal saline + ethyl acetate) was added and the sample was placed inside the kit and centrifuged for 1 min at 100 g speed and finally, the remaining fluid at the bottom of the kit was decanted and the sediment was transferred to the slide for microscopic examinations. The numbers of Blastocystis sp. cells in fecal materials were counted with a 40 × field microscope (15, 16).
Sampling was done from all referred and patients who used anti-parasitic diseases, those who did not want to participate were excluded from this study.
The data were statistically analyzed using SPSS V. 24 and by chi-square, ANOVA and t-test. P values < 0.05 and 0.001 were considered statistically significant.
4. Results
The presence of five or more Blastocystis sp. in the microscopic field (40 ×) was evaluated as positive. From 2500 assessed cases, 1494 (59.7%) were male and 1006 (40.3%) were female. Among the men, 195 (56.5 %) were infected and among the women a total of 150 (43.5 %) were infected with Blastocystis sp. by at least one stool sample. However, there was no statistical correlation between gender and Blastocystis sp. infection (Table 1). Consequently, the rate of Blastocystis sp. infection in cases referred to the Karaj central laboratories in 2014 and 2015 was counted as 13.8%.
| Variables | Blastocystis sp. | Total | P Value | |
|---|---|---|---|---|
| Positive | Negative | |||
| Gender | 0.08a | |||
| Male | 195 (56.5) | 1299 (60) | 1494 (59.7) | |
| Female | 150 (43.5) | 856 (40) | 1006 (40.3) | |
| Age group, y | 0.13a | |||
| ≤ 10 (1 mo - 10 y) | 171 (50) | 988 (46) | 1159 (46) | |
| 11 - 30 | 90 (26) | 655 (30) | 745 (30) | |
| > 30 (31 - 83) | 84 (24) | 512 (24) | 596 (24) | |
| Clinical symptoms | 0.16a | |||
| Symptomatic | 115 (33.3) | 433 (20) | 548 (22) | |
| Asymptomatic | 230 (66.7) | 1722 (80) | 1952 (78) | |
aNo significant difference was seen between infection with Blastocyst sp. and variables (gender, age and clinical symptoms).
In the reported assessment of pathological signs of Blastocystis sp. in patients whose stool examination was positive (infected with Blastocystis sp.). Among 345 infected people, 115 (33.3%) patients showed clinical Symptoms (Table 1).
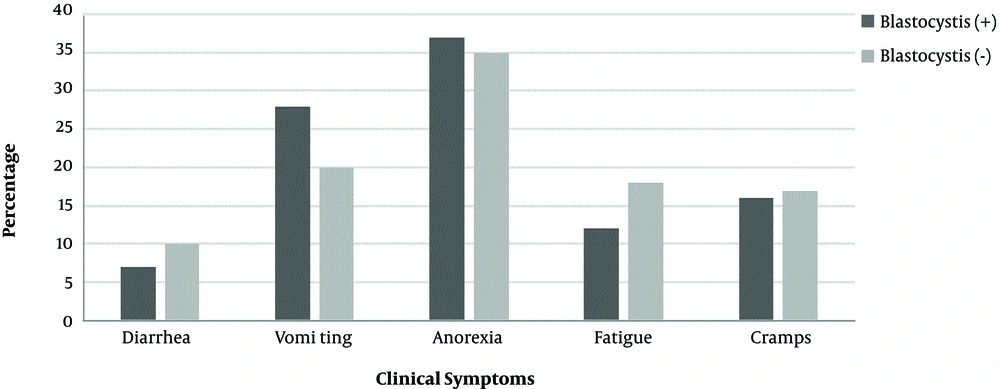
Among people with clinical symptoms; 37% had anorexia and were the highest and 7% had diarrhea, which was the lowest rate of clinical symptoms among those whose stool examination results were reported to be positive. Some of the people had simultaneously shown many signs, the most significant signs were diarrhea, vomiting/nausea, anorexia, flatulence and cramping as well as abdominal pain, respectively. There was no significant relationship between the symptoms of the disease in men and women (Figure 1).
Evaluation of Blastocystis sp. in sick people showed that the frequency of infection was mostly seen in people under the age of 10 (50%); no significant difference was seen between the infection with Blastocyst sp. and gender (P = 0.09).
5. Discussion
Blastocystis sp. is a commensal worldwide protozoan in the large intestine of both humans and wide range of other animals. The common clinical signs of this parasite include; fever, anorexia, abdominal pain, diarrhea, nausea, vomiting, constipation, weakening, and headache. The association of Blastocystis sp. with human disease is usually overlooked in clinical laboratories, and by practicing physicians and gastroenterologists. This infection was reported in different socioeconomic groups. Blastocystis sp. was found in Thailand (37.2%), Saudi Arabia (15%), as well as in primary school children in Malaysia (10.6%). In addition, more prevalence rates were observed in European countries, such as Italy (13.6%) and Turkey (0.96% - 56.3%) (17-20). In different regions of the world, the prevalence rate of this parasite was reported differently, for example in 2009 in France, the prevalence rate of this parasite was reported as 16.7%, which is close to the present study. However, in 2004 in Japan, the prevalence rate of this parasite was reported as 1% (21, 22). A study conducted in Nigeria showed that the prevalence of this parasite is related to hygiene, the rate of health care, and economic poverty. The prevalence of this parasite is reported differently in various regions of the world, especially in tropical and subtropical countries, however, it has a high scale of prevalence in developing countries due to low level of health and population congestion, absence of healthy water supply and sewage system, and economic and social problems (21). Due to the high prevalence of this protozoan, the submitted stool samples to the laboratories sometimes demonstrate relevant pathological signs (16, 23). The researchers have evaluated the prevalence rate of B. hominis in Tabriz (26.17%), Mashhad (36.8%), Mazandaran (6.8%) (3). In this study, we evaluated the prevalence rate of Blastocystis sp. in people referred to the central laboratories of Karaj city. The outcome of this study has shown that the prevalence of this parasite in the city of Karaj was 13.8%, however, the prevalence in Tehran, which has much similar weather and life conditions to Karaj city was estimated as 6.1% by Meamar et al. (7). This variation can be due to the difference between studied people, due to the fact that the researchers studied people with HIV. These patients used different drugs, which reduced the load of this parasite. However, in another study conducted by Akhlaghi et al., the prevalence of Blastocystis sp. parasite was estimated as 12.8%, which is more similar to the results of the present study (7, 8). In south western Iran, the prevalence of B. hominis was reported as 3.6% and 3.99% by Tork et al. (24), and Khoshnood et al. (25). The variation in the reported prevalence rate of this parasite can be attributed to the differences in weather and lifestyle of people living in that area. However, in a study conducted by Khoshnood et al., like the present study, the age range of children was under 10 - 15 years old. Moreover, in a study conducted by Mohtashamipour et al., in the Endocrine Glands and Metabolism Research Center of Isfahan city, the prevalence rates of B. hominis in control groups were sequentially reported as 9.3% and 2.5% (26). The outcomes of the present study have shown that the Blastocystis sp. Parasite, like Giardiasis, is one of the most common parasites in the city of Karaj.
Considering pathological signs noticed in patients infected with this parasite, it can cause many troubles to the society especially in kids due to the fact that its prevalence is much in underage children rather than elderly individuals; therefore, on time treatment of children is recommended. On the other hand, awareness of Blastocystis sp. and the use of concentrated solution of formalin-ether can increase the chance of noticing the parasite in a sample.
As this infection is related to hygiene, we can prevent the incidence of Blastocystis sp. by enhancing personal and public hygiene level. Due to the significant risk for zoonotic transmission, molecular techniques must be used to determine the route and source of infection (25-27).
Further research to evaluate the pathogenic potential of this organism is needed. To be protected from the disease, prevention, and control measures must be taken including education and personal hygiene and sanitation.
One of the limitations of the recent study was the lack of cooperation of many patients. Since each patient was sampled three times, many patients did not go for sampling.
5.1. Conclusions
The results of this study showed that Blastocystis hominis infection is one of the most common intestinal parasitic infections, and neglect of it can cause many problems for patients. Therefore, the use of appropriate diagnostic methods in the laboratories of hospitals and therapeutic centers can be effective in the correct and timely diagnosis; this will play an important role in promoting health and well-being in the community. In addition, due to the close relationship between the disease and environmental conditions, the disease can be a military threat to dormitory soldiers and needs to be continuously investigated in the densely populations.