1. Background
Since the global epidemiological transition from communicable diseases, which mostly had high mortality rates, to non-communicable diseases, which still have relatively high mortality rates but also impose high morbidity rates, the old epidemiological indices were not sufficient. This resulted in the announcement of a new index, namely, the burden of disease in 1990. In this index, health losses are calculated in disability-adjusted life years (DALY), a concise measure of population health that aggregates information about premature mortality, expressed as years of life lost (YLL), with data about non-fatal health losses attributable to time lived in states worse than complete health, expressed as years lived with disability (YLD) (1).
This index was used to calculate the projections of mortality and burden of disease by cause forward to 2000, 2010, and 2020 under three different scenarios (2). These estimations have been extensively used and continue to be quoted by World Health Organization (WHO) programs to provide a viewpoint on probable trends in global health (3). It has been reported that in all scenarios, there is a dramatic shift from communicable, maternal, perinatal, and nutritional causes to non-communicable disease causes, and from younger ages to older ones (2). Besides, it is estimated that the proportion of deaths due to non-communicable diseases will rise from 59 percent in 2002 to 69 percent in 2030 (2). On the other hand, the three leading causes of the burden of disease in 2030 are projected to include HIV/AIDS, unipolar depressive disorders, and ischemic heart disease (2).
Non-communicable diseases (NCDs) annually kill over 35 million people worldwide. They are responsible for nearly two-thirds of the world's deaths. Moreover, for the first time in human history, more than 80% of NCD-related deaths are in low- and middle-income countries (4).
Cardiovascular diseases are the main cause of mortality around the world. More than 75% of cardiovascular deaths occur in low- and middle-income countries. Considering that the prevalence is much higher in the 35 - 64 age group (i.e., the productive individuals), the costs will dramatically increase (5). In 2015, more than 46% of deaths were caused by cardiovascular diseases in Iran (6). With the increasing prevalence of risk factors for cardiovascular diseases, more emphasis should be placed on health policy, priority setting, and preventing cardiovascular disease deaths (5, 7, 8).
Recent reports show that, based on DALYs per 100,000 population, the rank of cardiovascular diseases in Iran has risen from 4th in 1990 to 1st in 2017, and the rank of mental disorders has risen from 7th in 1990 to 2nd in 2017 (9).
World Health Organization encourages countries continually to calculate the burden of diseases at the national level as the best guideline for taking policy in the health system. However, very few reports are now available for estimating the national burden of diseases in Iran (10-13). Besides, some other aspects have been well highlighted, such as the Adjustment of baccalaureate nursing curriculum with the burden of diseases in Iran (14), the effectiveness of adolescents' immunization against hepatitis B on the burden of the disease in Iran (15), and even in the scientometrics domain, such as the relation between Iranian Medical Science Research in the Scopus Database and the burden of disease in Iran (16) and comparisons with other countries (17). We did not find any study that focused on a specific population covered by a special institution. It seems that the importance of evaluating the burden of disease for health decision-makers in these institutions is neglected.
2. Objectives
To provide accurate information, this study aimed to estimate the burden of disease for cardiovascular and psychiatric disorders covered by an insurance fund.
3. Methods
This cross-sectional study was performed at Aja University of Medical Sciences in 2018 - 2019. The information for calculating YLL, YLD, and DALY was obtained from an insurance fund of the Islamic Republic of Iran. All the populations (i.e., census method) covered by this organization were included during 2012 - 2017, comprising 605,302 individuals across the country. The inclusion criteria were individuals who were under the coverage of that insurance fund during the study period and were hospitalized due to cardiovascular diseases or mental disorders.
Two diseases were investigated due to their highest disease burden in national and global estimates: (1) Cardiovascular diseases; and (2) mental disorders. These were extracted based on the international classification of diseases, 10th revision (ICD-10th revision).
To compute years lived with disability for a particular health outcome in a given population, the number of people living with that outcome is multiplied by a disability weight that represents the magnitude of health loss associated with the outcome. Disability weights are measured on a scale from 0 to 1, with 0 implying a state that is equivalent to full health and 1 a state equivalent to death. In this study, based on previous reports, the disability weight was considered as 0.323 and 0.600 for cardiovascular diseases and mental disorders, respectively.
We used the standardized template of WHO in Excel Software (version 2017) for calculations, which considers a standard discount rate of 0.03 and standard age weights of 0.04 (13, 18-20). It is highly recommended not to change these standards so that the results can be compared among various countries (21). The findings were represented as YLD, YLL, and DALY separately for cardiovascular diseases and mental disorders. These indices were also stratified and reported based on each study year (i.e., 2012 to 2017), age groups (i.e., 0 - 4, 5 - 14, 15 - 29, 30 - 44, 45 - 59, 60 - 69, 70 & higher), and gender (i.e., male, female). Additionally, the direct costs of these two diseases were obtained and reported.
4. Results
Overall, 605,302 individuals were covered by this specific insurance fund of the Islamic Republic of Iran. A total of 6,775 DALYs (3,953 in females and 2,823 in males) were lost due to cardiovascular diseases, which consisted of 5,691 YLLs (84%) and 1,084 YLDs (16%). On the other hand, 1,368 DALYs (571 years in females and 798 in males) were lost due to mental disorders, which consisted of 1,208 YLLs (88%) and 161 YLDs (12%).
As Table 1 shows, the highest YLLs were observed in the 60 - 69 age group for cardiovascular diseases and the 5 - 14 age group for mental disorders. As Table 2 shows, the highest YLDs were observed in the 60 - 69 age group for cardiovascular diseases and the > 70 age group for mental disorders. Finally, the highest YLDs were observed in the 60-69 age group for cardiovascular diseases and the 5 - 14 age group for mental disorders (Table 3).
| Age Groups | Cardiovascular Diseases | Mental Disorders | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
| 0 - 4 | - | - | - | 60.200 | 90.535 | - | - | - | - | - | - | - |
| 5 - 14 | - | - | - | - | - | 59.763 | 117.152 | 263.234 | 117.837 | 29.614 | 57.859 | - |
| 15 - 29 | - | - | - | - | - | - | 85.839 | 28.613 | - | 84.725 | 85.019 | 56.406 |
| 30 - 44 | 49.853 | 49.853 | 49.853 | 117.923 | 522.110 | 99.705 | - | - | - | - | - | - |
| 45 - 59 | 133.146 | 92.301 | 57.343 | 55.381 | 133.146 | 129.802 | - | - | - | - | - | - |
| 60 - 69 | 376.680 | 525.197 | 415.697 | 401.187 | 504.693 | 609.919 | - | - | - | - | 12.331 | 12.331 |
| 70 and higher | 339.304 | 153.874 | 63.359 | 175.028 | 298.855 | 126.947 | 87.917 | 56.877 | 58.155 | 15.520 | 31.040 | 7.760 |
| Age Groups | Cardiovascular Diseases | Mental Disorders | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
| 0 - 4 | - | - | - | - | - | - | - | - | - | - | - | - |
| 5 - 14 | - | - | - | - | - | - | - | - | - | - | - | - |
| 15 - 29 | - | - | - | - | 0.001 | - | 0.006 | 0.010 | 0.014 | 0.010 | 0.008 | 0.018 |
| 30 - 44 | 0.019 | 0.008 | 0.003 | 0.002 | 0.017 | 0.023 | 0.006 | 0.006 | 0.012 | 0.006 | 0.008 | 0.004 |
| 45 - 59 | 0.001 | 0.001 | 0.007 | 0.006 | 0.013 | 0.003 | 0.006 | 0.002 | - | - | - | 0.004 |
| 60 - 69 | 80.925 | 103.249 | 122.783 | 97.668 | 122.783 | 133.945 | - | 5.184 | 31.102 | 5.184 | - | 10.367 |
| 70 and higher | 43.492 | 55.489 | 64.488 | 121.477 | 67.487 | 70.486 | 8.358 | 25.073 | 11.143 | 22.287 | 22.287 | 19.501 |
| Age Groups | Cardiovascular Diseases | Mental Disorders | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | |
| 0 - 4 | - | - | - | 60.200 | 90.535 | - | - | - | - | - | - | - |
| 5 - 14 | - | - | - | - | - | 59.763 | 117.152 | 263.234 | 117.837 | 29.614 | 57.859 | - |
| 15 - 29 | - | - | - | - | 0.001 | - | 85.845 | 28.623 | 0.014 | 84.736 | 85.027 | 56.424 |
| 30 - 44 | 49.871 | 49.860 | 49.856 | 117.925 | 522.127 | 99.728 | 0.006 | 0.006 | 0.012 | 0.006 | 0.008 | 0.004 |
| 45 - 59 | 133.147 | 92.303 | 57.349 | 55.386 | 133.159 | 129.806 | 0.006 | 0.002 | - | - | - | 0.004 |
| 60 - 69 | 457.605 | 28.446 | 538.480 | 498.855 | 627.476 | 743.865 | - | 5.184 | 31.102 | 5.184 | 12.331 | 22.698 |
| 70 and higher | 382.795 | 209.364 | 127.846 | 96.504 | 366.342 | 197.433 | 96.275 | 81.949 | 69.298 | 37.807 | 53.327 | 27.261 |
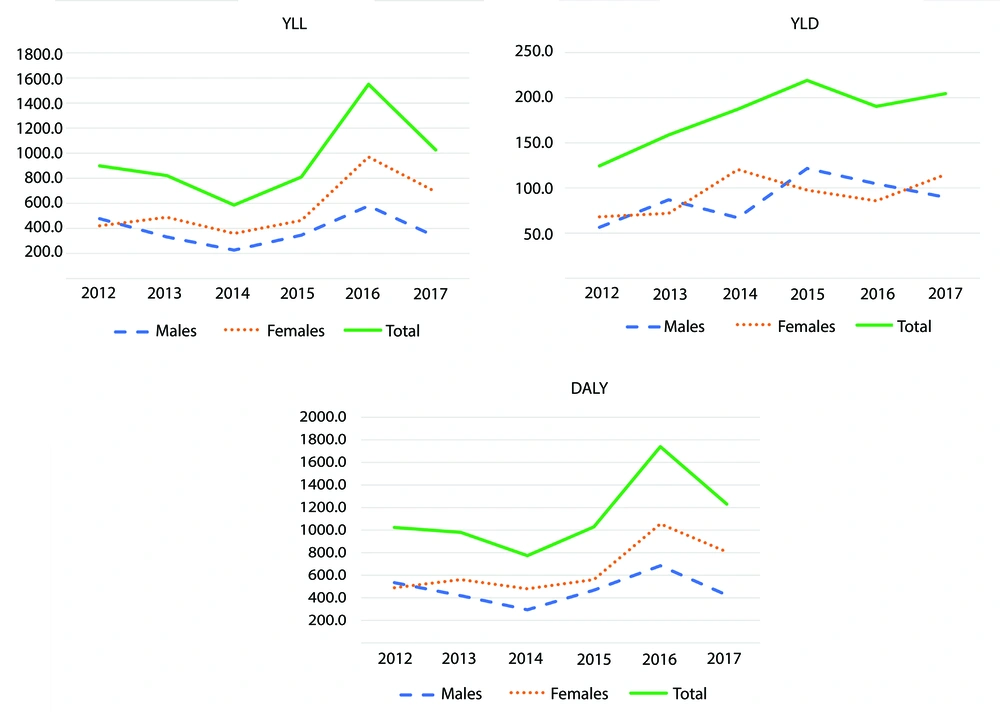
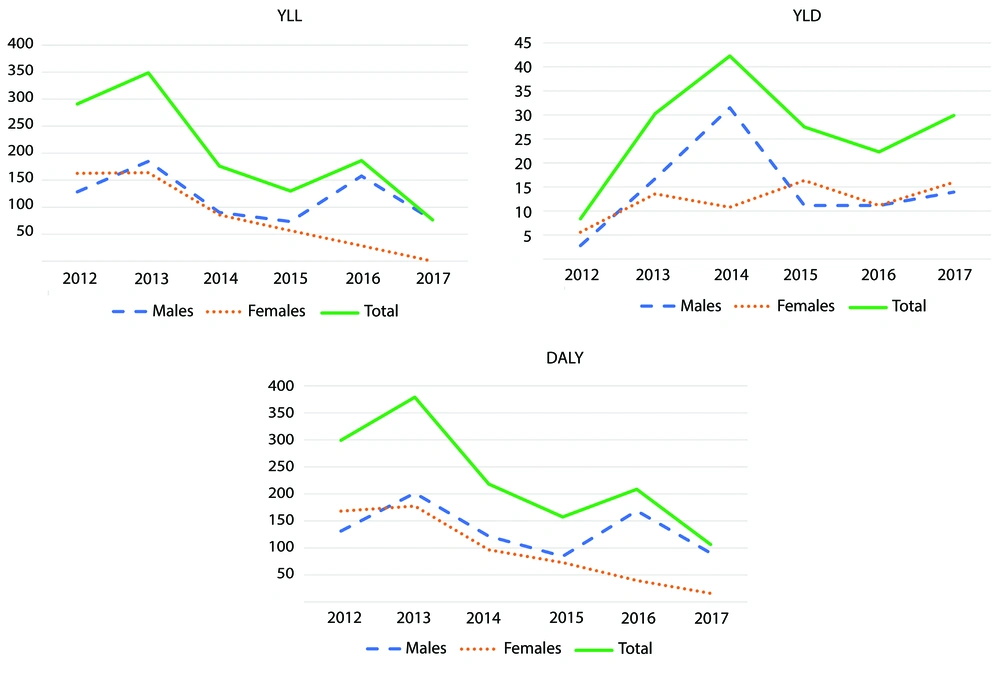
The trend of the three indices based on gender is demonstrated in Figures 1 and 2. The trends of YLL and YLD are both increasing for cardiovascular diseases, while YLL is decreasing for mental disorders and YLD shows an increasing-decreasing pattern. Overall, DALY exhibits a slightly increasing slope for cardiovascular diseases and a slightly decreasing slope for mental disorders.
The direct cost of cardiovascular diseases and mental disorders was also calculated. As Table 4 shows, more than 28.1 billion Rials were spent on cardiovascular diseases and 14 billion Rials on mental disorders. The trend in costs was increasing for both diseases.
| Year | Mental Disorders | Cardiovascular Diseases |
|---|---|---|
| 2012 | 824,766,644 | 2,149,017,553 |
| 2013 | 778,780,449 | 2,272,305,371 |
| 2014 | 1,710,554,050 | 2,548,691,990 |
| 2015 | 2,657,387,977 | 5,358,952,915 |
| 2016 | 3,354,103,836 | 7,962,309,165 |
| 2017 | 4,696,239,336 | 7,821,240,306 |
| Total | 14,021,832,292 | 28,112,517,300 |
5. Discussion
This study showed that in the two studied diseases, YLL was much higher than YLD (i.e., 7 times higher in cardiovascular diseases and 10 times higher in mental disorders). Over the 6-year study period, more than 6,775 years were lost due to cardiovascular diseases (3,953 in females and 2,823 in males). Additionally, 1,368 years were lost due to mental disorders (571 years in females and 798 in males). The trend of DALY was increasing in cardiovascular diseases but decreasing in mental disorders. These two diseases imposed more than 42 billion Rials of direct costs on the organizational health system.
As previously stated, there are very few studies about the burden of diseases in Iran. The first national study in Iran on the burden of disease was published in 2008. This study reported that 62% of DALYs were due to YLLs and 38% were due to YLDs (10). However, in our study, more than 84% and 88% of DALYs were due to YLLs in cardiovascular and mental disorders, respectively. Naghavi et al. (10) reported that in 2008, the top-ranked burden of disease was unintentional injuries in males, with nearly 2.8 million years of DALY, while mental disorders ranked highest in females, with nearly 1.2 million years of DALY. Although the authors stated that there was considerable variation in the burden of diseases among provinces, the top three causes of DALY (unintentional injuries, mental disorders, and cardiovascular diseases) were consistent across all six studied provinces.
The estimated DALY due to all diseases and injuries in Iranian children aged 0 - 14 years was 2,981,919 years (1,330,175 years in females and 1,651,744 years in males) in 2003 (12). Of these reported values, 56% were due to premature death (YLL), 44% to disability (YLD), 37% to perinatal diseases and delivery complications, 30% to external causes (injuries), and 7% to congenital diseases. In our study, we could not focus on children due to the very low incidence of the two studied diseases in this age group. However, similar to the previous report by Motlagh et al. (12), even though we did not restrict the age group, YLL dominated YLD in our study and had a greater impact on DALY. This finding explains that DALY closely follows the pattern of YLL more prominently than YLD.
As mentioned before, there is a very scarce body of evidence investigating the burden of disease in Iran. One such study is a report by Abolhasani et al., who estimated the DALY of osteoporosis to be 36,026 years in 2002 in Iran (11). To the best of our knowledge, this is the first study to evaluate the burden of two major diseases in a specific population covered by an insurance fund in Iran and even in the Middle East.
The burden of disease has also been utilized in educational and research contexts. In educational aspects, Aeen et al. reported that the proportion of credit hours in the nursing curriculum assigned to psychiatric, cardiovascular, respiratory, gastrointestinal, and sensory disorders, as well as intentional and unintentional accidents, nutritional deficiencies, and congenital anomalies, was less than the proportion of the burden of diseases as DALYs related to these diseases. Conversely, this proportion exceeded the optimum level for infectious diseases, maternal and antenatal problems, endocrine, genitourinary, and dermatologic diseases, and was at an optimum level only for musculoskeletal disorders and malignant neoplasms. The authors recommended a more precise revision of the baccalaureate nursing curriculum considering the above-mentioned diseases (14).
In research aspects, the relation between Iranian medical science research in the Scopus database and the burden of disease has been studied in Iran (16). It was shown that among 2,824 articles published in Scopus-indexed journals from 2010 - 2014, depression disorders and addiction had the highest (1,530 records) and lowest (62 records) numbers of publications, respectively. Additionally, major depressive disorders were found to have the greatest h-index, while the highest percentage of scientific productions with at least one citation was associated with addiction. Interestingly, a positive direct correlation was found between YLL (r = 0.8, P = 0.2), YLD (r = 0.2, P = 0.8), and mortality rate (r = 0.9, P = 0.205) with scientific productions. This could be promising in national aspects; however, the validity of institutional judgments about these results cannot be guaranteed. We believe the scientific production of each institution or even province should be aligned with the health issues (measurable by the burden of disease) in that location. Researchers should be guided and empowered to follow institutional research priorities. A more recent study on publication outputs showed that Iran's rank has improved from 16th (in 1996) to 11th (in 2017) in cardiology and from 15th (in 1996) to 12th (in 2017) in psychiatry (17).
Similar to our study, a trend analysis showed a decreasing level of psychiatric hospitalization during 2010 - 2016 in the northeast of Iran (22). It is suggested that focusing on mood disorders (as the most common cause of admission) and designing targeted interventions for high-risk groups (e.g., married unemployed men) can increase the effectiveness of interventions (22), especially for patients with suicide ideation, which has been found to be a more important predictor of suicide attempts compared to suicide planning (23). In this context, one of the main contributing factors is coping style. A considerable body of evidence shows that suicide attempters (24) and self-immolation patients (25) mostly use emotive coping strategies, while patients with intentional poisoning predominantly use avoidance and dreamlike coping mechanisms (26). This highlights the importance of targeted interventions to educate individuals on proper coping styles, particularly in high-risk groups.
In monetary aspects, Raghfar et al. evaluated the economic costs of coronary heart disease in Iran in 2014. They found that coronary heart diseases imposed an economic burden of 4,715 to 4,908 billion dollars (210,037,860,000,000 - 201,778,425,000,000 Rials). Additionally, the medical costs and the costs of lost productivity due to premature death were calculated as 3.572 billion USD (152,863,740,000,000 Rials) and 933 million USD (39,927,735,000,000 Rials), respectively. The major part of medical costs was related to angioplasty costs (47%) (27).
In our study, we only calculated the “direct cost” of cardiovascular diseases, which amounted to more than 28 billion Rials. It should be noted that we focused solely on individuals covered by this insurance fund, which explains the vast differences in costs. However, it was revealed that the direct cost due to cardiovascular diseases is more than twice that of mental disorders.
The overall estimation is that the more advanced a country is with a higher income, the more non-communicable diseases constitute a major part of the causes of mortality and morbidity (28). For instance, by 2030, diabetes is projected to be the fourth leading cause of death in developed countries, the sixth in middle-income countries, and the ninth in developing countries. Although diabetes ranks as the fifth leading cause of DALY in developed countries, it holds the tenth rank in middle-income countries and is not among the top ten causes in developing countries. However, the economic conditions of countries within each group can influence this concept.
There is a broad consensus that burden of disease indices are among the most solid and reliable pieces of evidence for health policymakers, health program management, health system research, and resource allocation (29-31).
5.1. Limitations
This study was not without limitations. The information required to conduct this study was extracted from data provided by a specific insurance fund. As a result, the analysis was based solely on data from hospitalized patients. Considering the necessity of hospitalization for the treatment of cardiovascular diseases and mental disorders, a reasonable estimate of the incidence of these diseases in the population under study can help ensure access to hospital services for all patients. Furthermore, all hospitals serving the specific population under the insurance fund were included in the study. The limitations of this study largely stem from the constraints of the data sources. Despite these limitations, the effort to estimate the burden of disease is justifiable, as even a less-than-perfect image is better than having no image at all. Relying on existing available data sources allows for an approximation of the burden of disease and highlights deficiencies and resource constraints. It is worth noting that, based on online searches, no similar study was found either in our country or our region that evaluates cardiovascular disease and mental disorders in such a specific population. This underscores the importance of this effort in filling a critical gap in the evidence base.
We suggest that preventive measures be implemented within this organization to address and mitigate major risk factors, at least for the two studied diseases. Additionally, we recommend that further studies evaluate other prevalent disorders within their population to provide a more comprehensive understanding of the disease burden.