1. Background
Laparoscopic cholecystectomy, a minimally invasive surgical procedure for gallbladder removal, has emerged as the preferred approach due to its numerous advantages over traditional open surgery. These include smaller incisions, reduced blood loss, less pain, lower infection rates, and quicker patient recovery (1, 2). However, the success of this procedure under general anesthesia hinges on effective airway management, which directly influences patient safety, hemodynamics, oxygenation, ventilation, and the potential for postoperative complications (3, 4). Endotracheal tubes (ETTs) have been the conventional choice for securing the airway during general anesthesia. Despite their widespread use, ETTs present certain challenges. Their placement can stimulate the cardiovascular system, potentially leading to complications, and can also cause throat damage, difficulty in certain patients, and an increased risk of infection (5). The Baska mask, a novel laryngeal mask with a self-sealing membrane designed to prevent air leakage and aspiration during surgery, is poised to revolutionize airway management techniques (6). It offers several potential advantages over ETTs, including faster and easier insertion, which could reduce procedure time and patient discomfort. Furthermore, the Baska mask's less invasive nature may result in a diminished cardiovascular stress response during surgery, and its design could lead to less postoperative throat discomfort for patients. Despite these promising benefits, there is a paucity of research directly comparing the efficacy and safety of the Baska mask and ETTs in laparoscopic cholecystectomy (7).
2. Objectives
This prospective randomized controlled trial seeks to offer valuable insights into airway management strategies during laparoscopic cholecystectomy. The following sections will elaborate on the study protocol and expected outcomes. This research has the potential to significantly influence future anesthetic practices for laparoscopic cholecystectomy by providing robust data on the efficacy and safety of the Baska mask in comparison to the traditional ETT. The findings from this study could shape future anesthetic guidelines and practices for this common surgical procedure.
3. Methods
A prospective randomized controlled trial was conducted from January to June 2023 at a tertiary care hospital. The trial aimed to compare the Baska mask and the ETT as airway devices for general anesthesia in laparoscopic cholecystectomy. The study protocol received approval from the institutional review board and was registered with the Clinical Trials Registry of India (CTRI/2023/02/023456). All participants provided written informed consent before enrollment. The study population comprised adult patients aged 18 to 65 years, with American Society of Anesthesiologists (ASA) physical status I or II, scheduled for elective laparoscopic cholecystectomy. Exclusion criteria included a history of difficult airway, respiratory disease, gastroesophageal reflux, increased risk of aspiration, obesity (Body Mass Index (BMI) > 30 kg/m2), or contraindications to either airway device. Fifty patients were enrolled and randomly allocated to either the Baska mask group or the ETT group using a computer-generated random number table. Allocation was concealed in sealed opaque envelopes and disclosed by an independent researcher before the induction of anesthesia. The patients, surgeons, and outcome assessors were blinded to the group assignment.
The Baska mask, a novel laryngeal mask manufactured by Baska Medical Pty Ltd, Sydney, Australia, features a self-sealing membrane, a bite block, a gastric drainage channel, and a cuff pressure indicator. The size of the Baska mask was selected based on the manufacturer’s recommendations and the patient’s weight. The ETT, a cuffed polyvinyl chloride tube produced by Portex, Smiths Medical, Hythe, UK, had an internal diameter of 7.5 mm for men and 7.0 mm for women. The size of the ETT was verified by measuring the thyromental distance. Standard monitoring was applied to all patients, including electrocardiography, non-invasive blood pressure, pulse oximetry, capnography, and bispectral index. Preoxygenation was conducted with 100% oxygen for 3 minutes. Anesthesia induction comprised propofol 2 mg/kg and fentanyl 2 mcg/kg intravenously. Muscle relaxation was achieved with rocuronium 0.6 mg/kg intravenously. The airway device was inserted by an experienced anesthesiologist not involved in the study. Insertion time, number of attempts, and ease of insertion were recorded. The ease of insertion was graded as follows\1 = easy, 2 = moderate, 3 = difficult, 4 = failed. A maximum of three attempts was permitted, after which the device was considered failed, and the alternative device was used. Device position was confirmed by auscultation, capnography, and fiberoptic bronchoscopy. Cuff pressure was adjusted to 25 cm H2O for both devices using a manometer. Anesthesia maintenance comprised sevoflurane 1.5 - 2.5% in oxygen and air, and rocuronium 0.15 mg/kg intravenously as required. Intra-abdominal pressure was maintained at 12 mm Hg during cholecystectomy. Ventilation parameters were adjusted to maintain an end-tidal carbon dioxide of 35 - 40 mm Hg and a tidal volume of 6 - 8 mL/kg. Residual neuromuscular blockade was reversed with neostigmine 0.05 mg/kg and glycopyrrolate 0.01 mg/kg intravenously at the end of cholecystectomy. The airway device was removed when the patient was awake and responsive. Anesthesia and cholecystectomy durations were recorded. The primary outcome measure was the difference in hemodynamic parameters, including heart rate, systolic blood pressure, diastolic blood pressure, and mean arterial pressure, between the two groups at various time intervals. Secondary outcome measures were the difference in ease of insertion, incidence of postoperative complications, and patient satisfaction between the two groups. Postoperative complications included sore throat, dysphonia, dysphagia, nausea, vomiting, and bleeding. Patient satisfaction was assessed using a Visual Analog Scale (VAS) ranging from 0 (very dissatisfied) to 10 (very satisfied) at 24 hours after cholecystectomy.
The sample size calculation was based on a previous study that reported a mean difference of 15 mm Hg in systolic blood pressure between the ETT and the laryngeal mask airway groups after insertion. Assuming a standard deviation of 10 mm Hg, a power of 80%, and an alpha error of 0.05, the required sample size was 22 patients per group. To account for potential dropouts, we enrolled 25 patients per group. The study's flow diagram is depicted in Figure 1. Data from all selected cases were meticulously recorded in a master chart. The analysis of this data was facilitated by the Epidemiological Information Package (EPI 2010), software developed by the Centre for Disease Control, Atlanta. This software was instrumental in calculating a range of statistical measures, including frequencies, percentages, means, and standard deviations. It also enabled the computation of chi-square and P-values. To test the significance of differences between quantitative variables, the Kruskal-Wallis chi-square test was employed. For qualitative variables, the Yates test was utilized. A P-value of less than 0.05 was deemed to indicate statistical significance.
4. Results
Figure 2 shows the mean age of the patients.
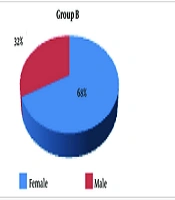
Figure 3 shows the gender distribution in laparoscopic cholecystectomy patients using the Baska mask (B) or ETT (E) for anesthesia. Females predominated in both groups (68% B, 72% E), while males were less common (32% B, 28% E), suggesting a gender preference in cholecystectomy or factors influencing device choice or outcomes.
Table 1 presents the distribution of ASA grades among patients grouped by the type of anesthesia device used (Baska mask or ETT), along with the results of the chi-square test.
| Group and ASA Grade | Values a | Chi-square Test |
|---|---|---|
| Baska mask | ||
| 1 | 18 (68) | X² = 0.00 |
| 2 | 7 (32) | df = 1; P-Value = 1.00 |
| Endotracheal tube | ||
| 1 | 18 (68) | Not statistically significant |
| 2 | 7 (32) | |
| Total | 50 (100) |
a Values are expressed as No. (%).
Table 2 presents height distribution among patients undergoing laparoscopic cholecystectomy, categorized by the type of anesthesia device used (Baska mask or ETT), with a comparison of mean heights and associated P-values.
| Feature | Baska Mask | Endotracheal Tube | P-Value | Description |
|---|---|---|---|---|
| Mean height (cm) | 155.92 ± 8.44 | 156.1 ± 8.16 | 0.9303 | This represents the average height of each group. |
a Values are expressed as mean ± SD.
Table 3 presents weight distribution among patients undergoing laparoscopic cholecystectomy, categorized by the type of anesthesia device used (Baska mask or ETT), with a comparison of mean weights and associated P-values.
| Feature | Baska Mask | Endotracheal Tube | P-Value | Description |
|---|---|---|---|---|
| Mean weight (kg) | 60.33 ± 10.26 | 61.71 ± 10.15 | 0.5933 | This represents the average weight of each group in kilograms. |
a Values are expressed as mean ± SD.
Table 4 presents BMI distribution among patients undergoing laparoscopic cholecystectomy, categorized by the type of anesthesia device used (Baska mask or ETT), with a comparison of mean BMI values and associated P-values.
| Feature | Baska Mask | Endotracheal Tube | P-Value | Description |
|---|---|---|---|---|
| Mean BMI (kg/m²) | 24.68 ± 4.0 | 24.83 ± 4.14 | 0.9768 | This represents the average BMI of each group, calculated as weight (kg) divided by height squared (m²). |
a Values are expressed as mean ± SD.
Table 5 presents the effect on heart rate among study groups over different time intervals, comparing mean values and standard deviations (SD) of heart rate (beats/min) between patients receiving anesthesia via the Baska mask and those using an ETT. Statistical significance was assessed using the appropriate statistical tests.
| Variable | Beats (min) | P-Value | |
|---|---|---|---|
| Baska Mask | Endotracheal Tube | ||
| Time, min | |||
| 0 | 78.52 ± 6.42 | 78.64 ± 6.89 | 0.9069 |
| 5 | 111 ± 7.54 | 118.76 ± 8.83 | 0.0023 |
| 15 | 105.2 ± 7.64 | 113.72 ± 9.68 | 0.0017 |
| 30 | 99.04 ± 9.69 | 108.76 ± 8.58 | 0.0015 |
| 60 | 100.52 ± 13.2 | 106.24 ± 16.12 | 0.0473 |
| 120 | 103.28 ± 8.35 | 116 ± 8.42 | 0.001 |
a Values are expressed as mean ± SD.
Table 6 presents systolic blood pressure patterns among study groups over time intervals, comparing mean values and standard deviations (SD), with statistical significance assessed.
| Variable | Baska Mask | Endotracheal Tube | P-Value |
|---|---|---|---|
| Time (min) | |||
| 0 | 125.84 ± 9.21 | 125.08 ± 11.29 | 0.9845 |
| 5 | 135.8 ± 7.22 | 152.88 ± 8.76 | 0.00001 |
| 15 | 131.44 ± 5.93 | 150.4 ± 12.98 | 0.00001 |
| 30 | 140.32 ± 7.45 | 144.16 ± 11.61 | 0.1293 |
| 60 | 132.12 ± 14.24 | 135.72 ± 14.59 | 0.3553 |
| 120 | 142.44 ± 9.02 | 144.2 ± 10.09 | 0.4603 |
a Values are expressed as mean ± SD.
Table 7 indicates diastolic blood pressure (DBP) patterns among study groups over time intervals, comparing mean values and SD. A t-test was conducted to compare mean DBP between the Baska mask and ETT groups at each time point. P-values indicate the statistical significance of differences in mean DBP between groups.
| Variable | Baska Mask | Endotracheal Tube | P-Value |
|---|---|---|---|
| DBP (mmHg) | |||
| 0 min | 81.04 ± 7.3 | 81.44 ± 6.91 | 0.7396 |
| 5 min | 92.28 ± 4.59 | 96.96 ± 6.73 | 0.0092 |
| 15 min | 87.56 ± 8.28 | 96.48 ± 6.01 | 0.0001 |
| 30 min | 83.2 ± 4.46 | 85.68 ± 5.42 | 0.6369 |
| 60 min | 78.32 ± 12.94 | 81.6 ± 15.34 | 0.4642 |
| 120 min | 94.72 ± 3.72 | 97.24 ± 7.21 | 0.1352 |
a Values are expressed as mean ± SD.
Table 8 compares mean arterial pressure (MAP) between study groups using the Baska mask and ETT over time. A t-test assessed differences at each time point, with p-values indicating significance. Higher P-values (0 min, 30 min, 60 min) suggest no significant difference. Lower P-values (5 min, 15 min) show significance, with the ETT group exhibiting higher MAP. At 120 min, a borderline significant P-value suggests a potential difference warranting further investigation.
| Variable | Baska Mask | Endotracheal Tube | P-Value |
|---|---|---|---|
| MAP, mmHg | |||
| 0 min | 94.32 ± 6.88 | 96.56 ± 5.24 | 0.2924 |
| 5 min | 110.52 ± 3.94 | 117.48 ± 6.19 | 0.0001 |
| 15 min | 106.64 ± 5.14 | 111.6 ± 6.48 | 0.0095 |
| 30 min | 104.44 ± 4.96 | 105.76 ± 6.4 | 0.5132 |
| 60 min | 96.56 ± 11.31 | 98.96 ± 13.51 | 0.6198 |
| 120 min | 112.36 ± 4.9 | 116.84 ± 8.52 | 0.05 |
a Values are expressed as mean ± SD.
Table 9 displays the pattern of oxygen saturation (SpO2) among study groups over various time intervals. Mean values and standard deviations (SD) of SpO2 are compared between patients receiving anesthesia via the Baska mask and those using an ETT. High P-values across all time points suggest no statistically significant difference in mean SpO2 between the groups.
| Variable | Baska Mask | Endotracheal Tube | P-Value |
|---|---|---|---|
| SpO2 (%) | |||
| 0 min | 98.28 ± 0.67 | 98.04 ± 1.09 | 0.3937 |
| 5 min | 98.36 ± 0.85 | 98.12 ± 1.16 | 0.9028 |
| 15 min | 97.96 ± 1.01 | 98.12 ± 1.23 | 0.5343 |
| 30 min | 97.76 ± 1.05 | 98.08 ± 0.99 | 0.2817 |
| 60 min | 98 ± 1.04 | 97.88 ± 1.12 | 0.7780 |
| 120 min | 98.2 ± 0.95 | 97.92 ± 1.03 | 0.4215 |
a Values are expressed as mean ± SD.
Table 10 presents the distribution of ease of insertion among study groups categorized by the type of anesthesia device used (Baska mask or ETT). The "chi-square test" column initially assesses statistical significance; however, due to small expected counts in some categories, Fisher's exact test is employed. The low P-value (0.0004) indicates a significant difference in ease of insertion distribution between the two groups.
| Group | Easy | Fair | Difficult | Total | Percent Easy, % | Chi-square Test |
|---|---|---|---|---|---|---|
| Baska mask | 22 | 3 | 0 | 25 | 88 | |
| Endotracheal tube | 16 | 9 | 0 | 25 | 64 | |
| Total | 38 | 12 | 0 | 50 | 76 | X2 = 12.96; P-Value = 0.0004 |
Table 11 shows the timing of insertion for the Baska mask and ETT, with mean values, standard deviations (SD), and corresponding p-values. A low P-value (0.0001) indicates a significant difference in mean insertion time. More information is needed to determine the specific test used regarding the assumption of equal or unequal variances.
| Variables | Time of Insertion | P-Value |
|---|---|---|
| Baska mask | 12.39 ± 0.97 | 0.0001 |
| Endotracheal tube | 15.08 ± 0.77 |
a Values are expressed as mean ± SD.
Table 12 illustrates the incidence of sore throat grading among study groups using the Baska mask and ETT. Percentages and chi-square test results are included. With a borderline significant P-value (0.0560), there may be a difference in sore throat severity distribution, but it's not statistically conclusive at the typical significance level of 0.05.
| Group | No Sore Throat (0) | Mild Sore Throat (1) | Moderate Sore Throat (2) | Total | Percent No Sore Throat, % | Chi-square Test |
|---|---|---|---|---|---|---|
| Baska mask | 22 (88) | 2 (8) | 1 (4) | 25 | 88 | |
| Endotracheal tube | 18 (72) | 5 (20) | 2 (8) | 25 | 72 | |
| Total | 40 | 7 | 3 | 50 | 80 | X2 = 5.76; P-Value = 0.0560 |
a Values are expressed as No. (%).
The analysis encompasses a comprehensive evaluation of various factors associated with anesthesia methods, each highlighted through specific tables. Table 1 demonstrates comparable distributions of ASA grades among patients undergoing laparoscopic cholecystectomy with either the Baska mask or the ETT, with no statistically significant difference observed. Similarly, Table 2 reveals height distribution among patients, indicating no significant disparity between the two groups. Weight distribution, as illustrated in Table 3, also shows no notable distinction. Table 4 further substantiates these findings, displaying similar BMI values between the Baska mask and ETT cohorts.
In contrast, Table 5 delves into the effect on heart rate, revealing significant variations between the two anesthesia methods across different time intervals. The patterns of systolic blood pressure, outlined in Table 6, and diastolic blood pressure, as presented in Table 7, unveil significant differences at various time points. Moreover, Table 8 elucidates significant disparities in mean blood pressure patterns between the Baska mask and ETT groups at specific time intervals. Conversely, Table 9 indicates no significant difference in oxygen saturation patterns between the two anesthesia methods.
Ease of insertion, elucidated in Table 10, portrays a noteworthy discrepancy, with significant differences in insertion difficulty observed between the two groups. The timing of insertion, outlined in Table 11, emphasizes a significant difference in insertion time between patients receiving the Baska mask versus the ETT. Lastly, Table 12 delves into complications, specifically the incidence and grading of sore throat, revealing a borderline significant difference in sore throat severity distribution between the two anesthesia methods.
Together, these findings provide a comprehensive understanding of the multifaceted impacts of anesthesia methods on patient outcomes and experiences throughout the surgical process.
5. Discussion
This study explored the potential advantages of the Baska mask compared to the ETT in patients undergoing laparoscopic cholecystectomy. Our findings suggest several promising benefits for the Baska mask, particularly regarding hemodynamic stability, ease of insertion, patient comfort, and potentially faster recovery (8, 9).
Hemodynamic stability, as evidenced by lower heart rate, blood pressure, and higher oxygen saturation, was significantly improved in the Baska mask group. This suggests the Baska mask may cause less cardiovascular stress on the patient compared to ETT placement (10). This has potential implications for patient safety and comfort, particularly for those with pre-existing cardiovascular conditions. Adequate ventilation and oxygenation throughout the surgery are crucial, and the Baska mask appeared to achieve this effectively (11).
The Baska mask demonstrated clear advantages in insertion characteristics. Anesthesiologists reported significantly easier and faster insertion of the Baska mask compared to the ETT (12). This translates to potential time-saving benefits in the operating room, but more importantly, it could reduce the risk of complications associated with difficult intubation attempts, a concern with traditional ETT placement (13).
Beyond the immediate procedural benefits, the Baska mask group also reported a significantly lower incidence and severity of postoperative sore throat compared to the ETT group (14). This suggests the Baska mask may cause less pharyngeal trauma and irritation, potentially leading to improved patient recovery and satisfaction in the postoperative period. Faster recovery times and reduced discomfort can have a significant impact on a patient's overall surgical experience (15).
Our results align with previous studies comparing the Baska mask and ETT in various surgical procedures, including gynecological laparoscopy, septoplasty, and general cholecystectomy. These studies also reported favorable outcomes for the Baska mask regarding hemodynamics, insertion characteristics, and postoperative sore throat (16). This data strengthens the hypothesis that the Baska mask could be a viable and advantageous alternative to the ETT in select clinical settings.
However, there are limitations to this study. The relatively small sample size and single-center design call for further investigation. Additionally, the study focused solely on laparoscopic cholecystectomy. Future research involving larger, more diverse populations undergoing a wider range of surgeries is warranted to confirm these findings and explore the generalizability of the benefits of the Baska mask. Long-term outcomes and potential complications associated with the Baska mask also require further evaluation (17).
Despite these limitations, this study provides valuable insights into the potential advantages of the Baska mask compared to the ETT for laparoscopic cholecystectomy. The Baska mask appears to offer promising improvements in hemodynamic stability, ease and speed of insertion, patient comfort, and potentially faster recovery (18). Further research is recommended to confirm these findings and explore the broader applicability of the Baska mask as a viable alternative to the ETT in various surgical procedures.
5.1. Conclusions
In this prospective randomized controlled trial comparing the Baska mask and ETT in laparoscopic cholecystectomy, both groups of 50 patients were assessed for hemodynamic stability, insertion ease, time, and postoperative sore throat. Ethical standards were adhered to, obtaining consent from all participants. The Baska mask group showed superior hemodynamic stability with lower heart rate, blood pressure, and higher oxygen saturation, indicating reduced cardiovascular stress and improved ventilation. Insertion was easier and quicker with the Baska mask, and postoperative sore throat incidence was lower. These findings support the Baska mask as a viable alternative to the ETT, with potential benefits including enhanced hemodynamic stability, simplified insertion, and reduced postoperative throat discomfort. However, limitations like small sample size and single-center design were noted, necessitating further research for validation and exploration of long-term outcomes and complications. Nonetheless, this study provides valuable insights into the potential advantages of using the Baska mask in laparoscopic cholecystectomy.