1. Background
Patients undergoing chest wall surgeries often experience intense postoperative pain, which is predominantly nociceptive and neuropathic (1). Analgesia for these surgeries can be administered through various methods, including immediate intravenous and intramuscular routes, regional nerve blocks, and, later in the postoperative period, orally or intramuscularly. Paravertebral blocks and thoracic epidural analgesia have been considered gold-standard techniques for many years but are associated with complications such as pneumothorax, total spinal block, intrathecal spread, epidural hematoma, and the risk of neurological damage (2, 3). This has led to an increased demand for and popularity of ultrasound-guided (USG) pectoral nerve blocks (PEC blocks) (4).
R. Blanco pioneered the USG-guided PEC blocks, a novel superficial plane block technique that has recently been implemented to provide analgesia in chest wall surgeries (2). The PEC1 block anesthetizes the lateral pectoral nerve (C5 to C7) and medial pectoral nerve (C8 to T1) (5). The PEC2 block targets the pectoral, intercostobrachial, third to sixth intercostal, long thoracic, and thoracodorsal nerves.
2. Objectives
Therefore, this study was conducted to evaluate the efficacy of USG-guided PEC blocks postoperatively in patients undergoing chest wall surgeries, using 0.2% ropivacaine and fentanyl. The primary objective is to assess the total duration of postoperative analgesia, while the secondary objectives include calculating the total consumption of opioids/non-opioids, the Numeric Rating Scale (NRS) score, and any complications.
3. Methods
Following the approval of the institutional ethical committee and CTRI Registration, we conducted this prospective randomized trial at a tertiary care hospital from August 2020 to December 2021. We included 60 ASA I, II, and III patients aged 18 to 65 years after obtaining written and informed consent. These patients were scheduled for elective chest wall surgeries.
The surgeries encompassed procedures such as fibroadenoma excision, mastectomy, modified radical mastectomy with axillary dissection, synthetic breast expander implantation, breast reconstruction, cardiac pacemaker insertion, anterior thoracotomy, and shoulder surgeries. Patients were excluded from the study if they refused to give consent, were on anticoagulant drugs, had deranged liver function tests (LFTs), had an allergy to local anesthetics, had bleeding diathesis, were pregnant or lactating or had skin ulceration or infiltration of the chest wall at the site of the block.
The PEC1 block involved administering the local anesthetic solution in the plane between the pectoralis major and minor muscles, while the PEC2 block involved administration between the pectoralis minor and serratus anterior muscles.
In the preoperative room, all patients were informed about the NRS for pain at rest and were instructed to rate their pain accordingly, from 0 to 10 (0 indicating no pain, 1 to 3 mild pain, 4 to 6 moderate pain, and 7 to 10 severe pain).
All patients were instructed to fast overnight before surgery and were prescribed a tablet of alprazolam 0.25 mg at bedtime. Baseline parameters such as heart rate (HR), non-invasive blood pressure (NIBP), oxygen saturation (SpO2), temperature, and end-tidal carbon dioxide (ETCO2) were recorded.
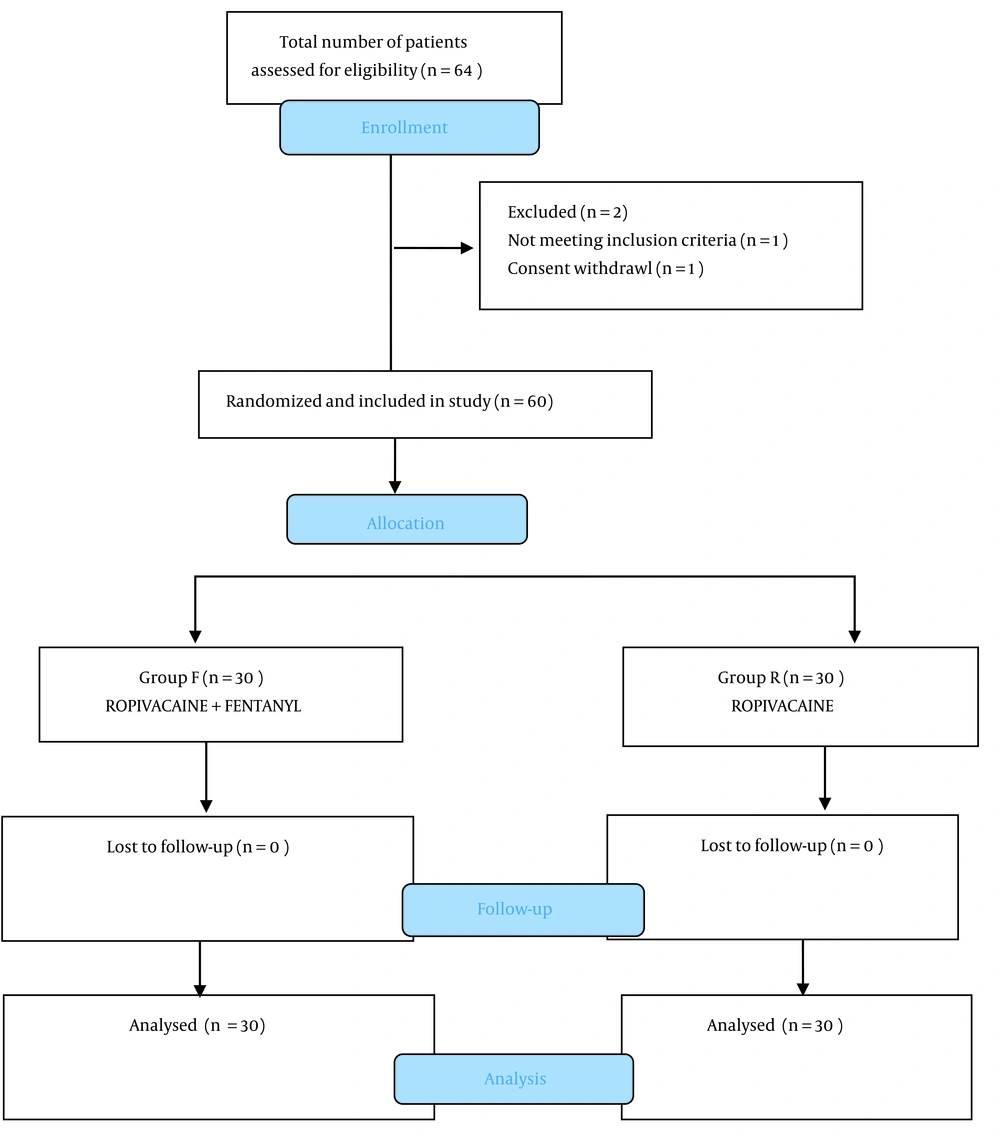
Patients were randomly divided into two equal groups according to the Consort statement (Figure 1) based on the drug administered in the PEC block:
- Group R received an injection of 0.2% ropivacaine 38 mL + 2 mL normal saline (total 40 mL).
- Group F received an injection of 0.2% ropivacaine 38 mL + 2 mL fentanyl (100 mcg) (total 40 mL).
To maintain the triple-blinded nature of the trial, the tasks of preparing the drug, administering the block, and observing the patient for postoperative analgesia for data collection were assigned to different individuals.
Patients were transferred to the operating theater, where ECG, NIBP, SpO2, temperature, and EtCO2 monitors were attached, and an IV line was secured. All patients were induced with general anesthesia, premedicated with inj. midazolam 0.02 mg/kg IV, inj. Glycopyrrolate 0.05 mg/kg IV, inj. ondansetron 4 mg IV, and inj. fentanyl 2 mcg/kg IV. Induction was achieved with inj. propofol 2 mg/kg IV and inj. succinylcholine chloride 2 mg/kg IV. The trachea was intubated with an appropriately sized endotracheal tube with a cuff, which was secured after verifying bilateral equal air entry by auscultation and confirmed with EtCO2.
Patients were maintained on a mixture of 50% oxygen and 50% air, and sevoflurane (MAC 2 - 3%) was used. Inj. atracurium 0.5 mg/kg IV was administered as a muscle relaxant loading dose, with 0.1 mg/kg IV given intermittently for maintenance. Adequate crystalloid Ringer's lactate was administered for maintenance, and blood loss and third space loss were replaced according to NBM hours and ideal body weight.
Upon completion of the surgery and prior to extubation, a USG-guided PEC1 and PEC2 block was administered to the patients according to the group they were allocated to (group R and group F). The PEC block was performed with the patient in a supine position and the ipsilateral upper limb abducted, using a linear USG probe (6 to 13 MHz). The probe was initially placed in the infraclavicular region, then advanced laterally to locate the axillary artery and vein directly above the first rib between the pectoralis major and pectoralis minor for the PEC1 block, where 10 mL of the drug was administered, followed by the PEC2 block, where 20 mL of the drug was administered between the pectoralis minor and serratus anterior.
Parasternal infiltration was performed with 10 mL from a prefilled syringe to provide analgesia for the medial part of the breast (innervated by the supramammary and inframammary nerves). The time of the block was recorded, and vital signs such as pulse, BP, and SpO2 were monitored.
After completing the procedure and once adequate reflexes were regained, patients were administered inj. glycopyrrolate 0.04 mg/kg IV and inj. neostigmine 0.05 mg/kg IV for reversal. Upon regaining consciousness, patients were extubated and then transferred to the recovery room for observation following our hospital’s routine postoperative protocols. Postoperative pain was assessed and managed according to the NRS score.
Vital signs and pain were assessed using the NRS at 0 hours, 30 min, 1, 2, 4, 6, and 12 hours (0 hour was defined as the time when the patient was shifted to the postoperative care unit). If the NRS was < 3, inj. paracetamol 1 gm IV was administered. If the NRS was > 3, inj. fentanyl 10 mcg IV was given every 10 minutes until the NRS was < 3. Therefore, inj. fentanyl was used for immediate pain relief and inj. paracetamol for long-duration pain relief as per our hospital protocol for rescue analgesia.
The primary outcome measures observed and studied were:
(1) Time of first rescue analgesia.
(2) Duration of analgesia (from the time of the block to the time when the first rescue analgesia was administered).
(3) Total cumulative dose of inj. fentanyl and paracetamol were given during the first 24 hours postoperatively.
The secondary outcomes were:
(1) Numeric Rating Scale score in both groups of patients at rest and during movement.
(2) Any adverse effects, such as local anesthesia toxicity, pneumothorax, nausea, vomiting, failure of the block’s effect, or respiratory depression, were noted.
3.1. Statistics
The data were collected and statistically analyzed using SPSS version 26. The data was explored using minimum, maximum, mean, and standard deviation for normally distributed data. Tests applied were the independent t-test or Mann-Whitney test, and the P-value was calculated for comparison and inference between both groups.
4. Results
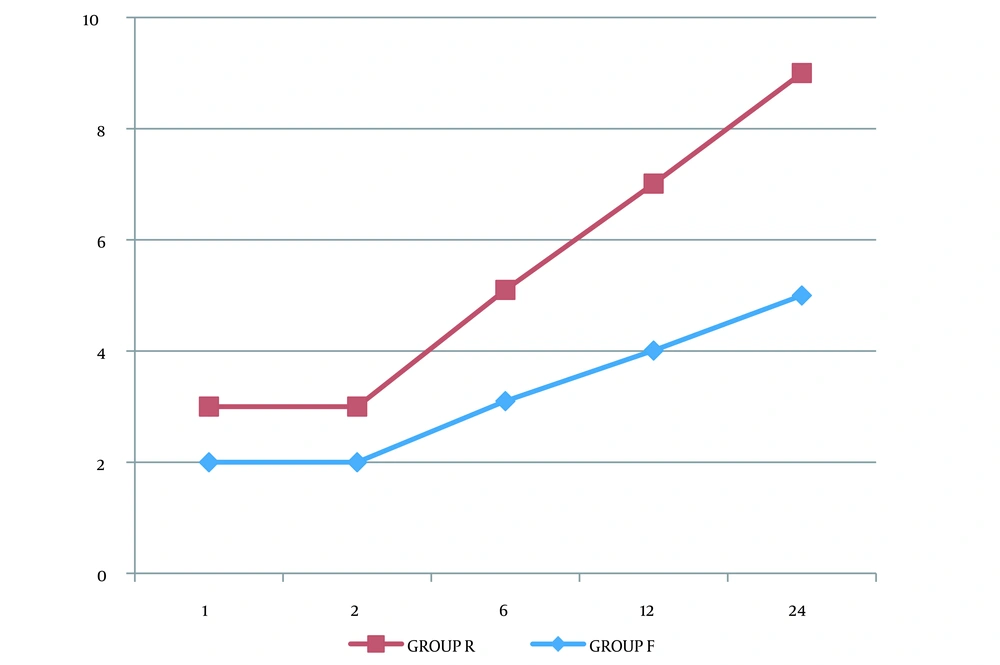
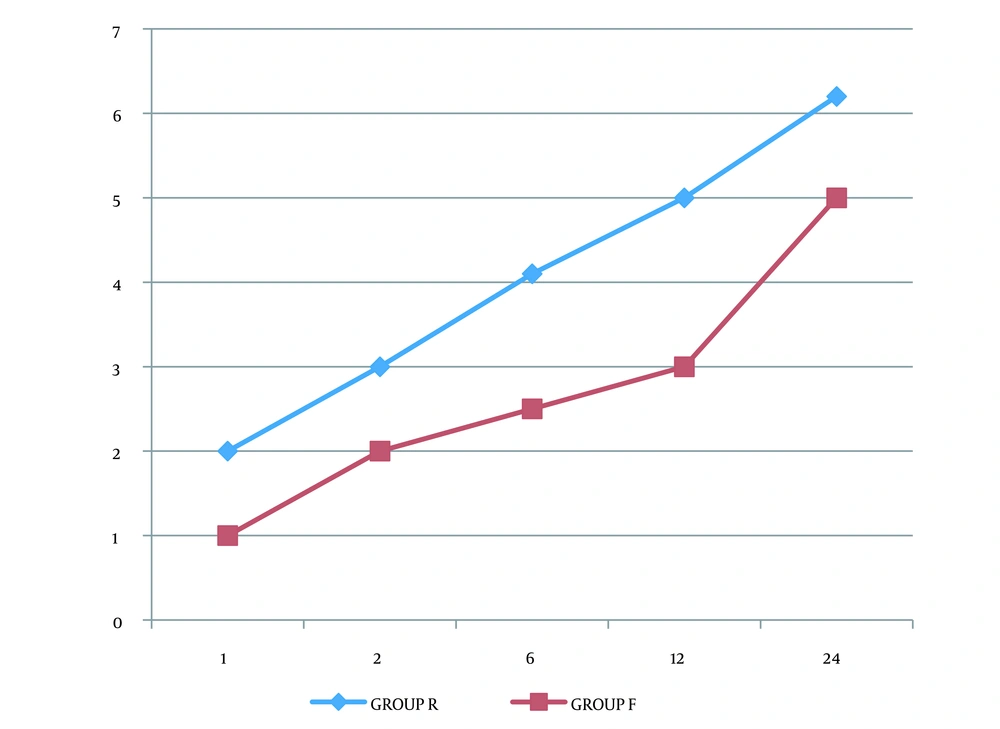
Demographic variables were comparable between the two groups, with no significant differences observed (Table 1). The time to the first rescue analgesia was longer in group F compared to group R. Total consumption of paracetamol and fentanyl was significantly lower in group F than in group R, with a P-value < 0.0001 (Table 2). The NRS score at rest in group F was lower than in group R (Figure 2), and the NRS score during movement in group F was also lower than in group R (Figure 3).
| Variables | Group R | Group F | P-Value |
|---|---|---|---|
| Age, y | 48 ± 15.3 | 46 ± 13.2 | 0.658 |
| M: F | 27: 3 | 26: 4 | - |
| Weight, kg | 61.50 ± 6.3 | 58.73 ± 5.6 | 0.48 |
| Height, cm | 144 ± 6.1 | 151 ± 3.42 | 0.19 |
| Duration of surgery, min | 119.2 ± 12.32 | 116.3 ± 13.46 | 0.3876 |
| ASA 1/2/3 | 10/8/12 | 9/11/10 | - |
a Values are expressed as mean ± SD.
| Parameter | Group R | Group F | P-Value |
|---|---|---|---|
| Time of 1st rescue analgesia, h | 8.28 ± 0.51 | 11.02 ± 2.01 | < 0.0001 |
| Total paracetamol consumption, g | 2.2 ± 0.8 | 1.5 ± 0.5 | < 0.0001 |
| Total fentanyl consumption, mcg | 35.1 ± 13.4 | 0 | < 0.0001 |
a Values are expressed as mean ± SD.
5. Discussion
The administration of peripheral nerve blocks has become increasingly recognized as a crucial component of the anesthesia care regimen.
In our study, we administered USG-guided PEC1 and PEC2 blocks along with parasternal local infiltration according to the group allocation. There were no differences between the two groups in terms of demographic data such as age, gender, weight, height, duration of surgery, and ASA grading (Table 1). The total duration of analgesia, or the time until the demand for the first rescue analgesia (measured from the time of block administration until the time when the first dose of rescue analgesia was needed), was observed and noted. In group R, it was 8.28 ± 0.51 hours, and in group F, it was 11.02 ± 2.01 hours (p-value < 0.0001), being statistically highly significant (Table 2).
Frenny et al. conducted a study titled "Intraoperative pectoral nerve block (PEC) for breast cancer surgery," dividing participants into two groups: One receiving 0.2% ropivacaine and the other normal saline as a placebo for the PEC block postoperatively. The time to the first rescue analgesia in their study was 353.93 ± 135.03 minutes for the ropivacaine group and 27.17 ± 18.08 minutes for the placebo group, demonstrating a significant difference that proved ropivacaine to be an efficient and effective analgesic agent (6).
Mahajan and Kaushal, in their study, compared a USG-guided PEC block given preoperatively with local anesthesia infiltration and observed that the duration of analgesia was 30.07 hours in the PEC block group versus 8.13 hours in the local infiltration group (7).
The results further reinforce our observations concerning the timing and duration of the first rescue analgesia. Contrary to our study, Assem Razek presented slightly different results with USG pectoral nerve blocks versus serratus intercostal plane blocks (SIPB) in breast surgeries, emphasizing that SIPB provided better analgesia compared to PEC blocks (8). This contrasted with our study's findings. The difference may be attributed to the timing of the block administration in Razek's study, which was preoperative. The preoperative administration of PEC blocks was shown to create fluid-filled tissue planes during dissection due to the spread of local anesthetic between two planes, resulting in tissue edema and reducing the efficacy of electrocautery.
To address this, in our study, we administered the PEC block postoperatively at the end of surgery prior to extubation, as the extra few minutes allowed for safe and quick administration of the block. Moreover, the structures dissected during surgery facilitated easy identification and helped avoid complications.
We also evaluated the total postoperative paracetamol consumption (group R 2.2 ± 0.8 g and group F 1.5 ± 0.5 g) as well as the total postoperative fentanyl consumption (group R 35.1 ± 13.4 mcg and group F 0) and found a significant reduction in the analgesic requirements in group F compared to group R (Table 2), with a P-value < 0.0001. This reduction in the postoperative analgesic requirement, as compared to other studies, can be explained by the fact that the block was administered at the end of the resection and after washing, which likely contributed to an increased duration of analgesia and a reduction in the dosage of other opioid analgesics. The injected drug solution is more likely to remain in the tissue plane where it is deposited, unlike when administered preoperatively, where it might leak during tissue dissection.
A similar study concluded that the total paracetamol dosage of 2.71 ± 0.46 g and total fentanyl of 0 mcg was significantly lower than in the placebo group, where the total paracetamol was 3.53 ± 1.074 g and fentanyl was 34.67 ± 13.58 mcg (6).
Shweta Mahajan and Kaushal, in their research, stated that the total dosage of rescue analgesia in the local infiltration group was significantly higher than in the PEC block patients (P < 0.05) (7). Similarly, in our study, the addition of fentanyl as an adjuvant to 0.2% ropivacaine significantly reduced postoperative analgesia due to synergistic effects compared to 0.2% ropivacaine alone.
Parenteral administration of opioids is an integral part of multimodal perioperative analgesia in major thoracic surgeries performed under general anesthesia. However, a reduction in opioid usage in oncological surgeries markedly improves outcomes as opioids have immunomodulatory effects, such as the promotion of cell migration and NET 1 gene migration (9).
We monitored the NRS score postoperatively at rest and during movement in all patients at various time intervals. The plotted graphs clearly show that the NRS score in group F is significantly lower compared to group R (Figures 2 and 3).
Razek et al. found that the Visual Analog Scale (VAS) pain scores were lower in the SIPB group compared to the PEC block group (8). Mahajan had similar observations, where VAS scores demonstrated the superiority of the PEC block over local infiltration (7).
We preferred 0.2% ropivacaine as the study drug solution over other local anesthetics because it has a reduced propensity for motor blockage and offers good postoperative pain control efficacy. It possesses reduced cardiotoxicity and CNS toxicity and leads to fewer side effects in the event of accidental intravascular penetration compared to other anesthetic agents (10).
Rajkhowa et al. conducted a study entitled "Fentanyl as an Adjuvant for Brachial Plexus Block: A Randomized Comparative Study" on 66 patients undergoing orthopedic surgeries of the forearm. They compared the analgesic efficacy of fentanyl used as an adjuvant to ropivacaine for the supraclavicular brachial plexus block and concluded that the addition of fentanyl to ropivacaine significantly prolonged the duration of analgesia compared to ropivacaine used alone (11).
Sinha et al. conducted a study comparing the erector spinae block with the PEC block in breast cancer surgeries involving 60 patients. They concluded that the PEC2 block was superior in terms of efficacy for postoperative analgesia and opioid consumption (12). Kumar et al. carried out a randomized controlled trial administering the PEC block to patients undergoing modified radical mastectomy and observed that the VAS pain score was lower in patients who received the PEC block, indicating that the PEC block provides excellent postoperative analgesia in the first 24 hours (13).
These studies, along with others (14, 15), demonstrate a synergistic effect of fentanyl as an adjuvant with ropivacaine in prolonging the duration of the block and reducing postoperative analgesic requirements. The USG approach is preferred over the blind block technique because real-time USG reduces known complications of the PEC block, such as pneumothorax and intravascular penetrations, and achieves a denser effect with a reduced volume of the drug compared to the larger volume required for the blind block approach.
The USG-guided PEC block is now considered a modern technique, surpassing the gold standard thoracic epidural because it is easier and quicker to perform, does not involve a sympathetic block, and thus leads to decreased hypotension. This makes it increasingly preferred for day-care procedures due to its segmental and safe effect.
5.1. Conclusions
In conclusion, the USG-guided PEC block, utilizing 0.2% ropivacaine with fentanyl as an adjuvant, is an excellent and ideal combination for pain-free chest wall surgeries. It improves patient satisfaction by serving as an excellent alternative to conventional approaches.