1. Background
Postoperative nausea and vomiting (PONV) are common side effects following laparoscopic procedures (1-3). In patients receiving postoperative opioids, PONV has an incidence of 20 - 40%. However, if antiemetic prophylaxis is insufficient, the incidence can rise to around 80% in those with multiple PONV risk factors (4-6). Several PONV risk factors, such as obesity, a history of postoperative nausea and vomiting (motion sickness), type of surgical procedure, anesthetic method, and preoperative eating pattern, have been reported (1, 7, 8).
Although these symptoms typically occur within the first 4 to 6 hours, they rarely persist beyond 24 hours (9, 10). While most patients experience mild symptoms, others may suffer from serious adverse effects, including electrolyte imbalance, dehydration, gastric content aspiration, and prolonged recovery (11, 12).
Despite the availability of several antiemetic medications, such as Metoclopramide, Ondansetron, Dexamethasone, Glycopyrrolate, Diphenhydramine, and Droperidol, some are limited by their adverse effects and varying effectiveness in treating patients (13, 14). Dexamethasone alone or in combination with other medications has been found effective in preventing PONV in several studies (15-18).
Herbal therapy, as a complementary and alternative medicine (CAM), is widely used worldwide. Ginger (Zingiber officinale) is one of the most commonly used herbal remedies, traditionally used to alleviate gastrointestinal problems, including nausea and vomiting (15, 16). Recent studies have suggested that Ginger's antiemetic properties may stem from its anti-serotonin-3 effects on either the central nervous system or gastrointestinal receptors, as well as 6-Gingerol, which is responsible for its aromatic, spasmolytic, carminative, and absorbent effects (16, 17).
2. Objectives
The present study aimed to compare the efficacy of Ginger capsules in preventing postoperative nausea and vomiting with that of Dexamethasone, a conventional treatment for PONV.
3. Methods
This is an observational prospective study conducted at Labbafinejad Hospital (Tehran, Iran) from December 2019 to November 2021. All patients were informed about the study's purpose, and written informed consent was obtained from each patient. The ethical committee approved the study design of the Iranian Urology and Nephrology Research Center at Shahid Beheshti University of Medical Sciences with the number unrc.911222.9.
Patients enrolled in this study were randomly divided into two groups: The Dexamethasone group (Group A) and the Ginger group (Group B).
3.1. Inclusion Criteria
The inclusion criteria were as follows: An age range of 18 to 65 years old, ASA (American Society of Anesthesiologists) classification groups I or II, patients who were candidates for laparoscopic non-function simple nephrectomy, live donor nephrectomy, and partial or radical nephrectomy.
3.2. Exclusion Criteria
Patients with a history of motion sickness, gastrointestinal surgery, drug addiction, cholecystolithiasis, hepatitis, coagulopathy, pregnancy, or a Ginger allergy were excluded from the study.
3.3. Study Design
A Ginger capsule (500 mg) was prepared in identical forms at a pharmacology laboratory. Eligible patients were randomly divided into two groups. Thirty minutes before anesthesia, Group A received 8 mg of intravenous Dexamethasone, and patients in Group B were given a Ginger capsule (500 mg).
According to the anesthesiologist's expertise, conditions of anesthesia, such as the type of medication and duration of anesthesia administration, were standardized. The medication for anesthesia induction included Midazolam 1 mg, Propofol 2 mg/kg, Fentanyl 2 µg/kg, Atracurium 0.5 mg/kg, and Lidocaine 1.5 mg/kg. Additionally, Isoflurane 1 - 1.5 MAC (minimum alveolar concentration) and fentanyl/Atracurium boluses were used to maintain anesthesia.
The intraperitoneal technique was employed in a lateral decubitus posture to perform laparoscopic nephrectomy. CO2 was used to insufflate the peritoneal cavity at a maximum pressure of 12 mmHg. Hemodynamic status was monitored throughout the operation and in the recovery room. After the procedure, all patients were monitored in the recovery room for three hours. Vomiting during the extubating procedure was not considered a sign of favorable postoperative vomiting.
Vomiting was defined as the forceful ejection of digestive tract contents through the mouth due to significant gastrointestinal stimulation. All episodes of vomiting in the recovery room and their medical treatment were recorded by nurses who were unaware of the research groups. The frequency of vomiting in the first 24 hours following surgery was recorded separately.
A Visual Analogue Scale (VAS) scores of 0 (no), 1 to 3 (mild), 4 to 6 (moderate), 7 to 9 (severe), and 10 (very severe) was used to measure the patients’ pain in the first 24 hours (20). Additionally, patients’ hemoglobin and hematocrit levels were measured 6 hours and 24 hours after surgery.
3.4. Data Analysis
The collected data were analyzed using SPSS software (IBM, Version 22). Independent sample t-test, one-way ANOVA, and Chi-square test were conducted to compare means and ratios in this study. A P-value less than 0.05 was considered statistically significant.
4. Results
A total of 131 patients aged 18 to 65 years were included in this study. Before the operation, Group A received Dexamethasone (8 mg) (N = 70), while Group B was given Ginger capsules (500 mg) (N = 61).
The demographic data are summarized in Table 1. The average age of patients in Groups A and B was 37.04 ± 13.89 and 38.44 ± 13.45 years, respectively, with no statistically significant differences between the two groups (P = 0.52). There was also no significant difference in the mean operation time between the two groups, which were 220 and 218 minutes in Groups A and B, respectively (P = 0.65) (Table 1).
| Variables | Ginger Group(B) (N = 61) | Dexamethasone Group(A) (N = 70) | P-Value b |
| Age (y) | 38.4 ± 13.45 | 37.04 ± 13.89 | 0.52 |
| Gender | 0.06 | ||
| Female | 24 (39.5) | 19 (27) | |
| Male | 37 (60.5) | 51 (73) | |
| Type of nephrectomy | 0.31 | ||
| Total | 53 (87) | 59 (84.3) | |
| Partial | 7 (11.5) | 8 (11.5) | |
| Radical | 1 (1.6) | 3 (4.2) | |
| Past medical history | |||
| HTN | 2 (3.2) | 3 (4.2) | 0.5 |
| DM | 3 (4.9) | 3 (4.2) | |
| HTN + DM | 2 (3.2) | 3 (4.2) | |
| Duration of surgery(H) | 3.64 ±0.41 | 3.67 ± 0.48 | 0.65 |
Patients' Data in Ginger and Dexamethasone Groups a
In the Dexamethasone group (Group A), 26 patients (37%) experienced at least one episode of vomiting in the recovery room (within 6 hours after surgery), while in Group B (Ginger capsule), seven patients (11%) suffered from vomiting (P = 0.001). Further analysis revealed that seven patients in the Ginger group experienced only one episode of vomiting after surgery in the recovery room. In contrast, in the Dexamethasone group, 21 patients had one episode, and 5 patients had two episodes of vomiting. Among the 26 patients in the Dexamethasone group, 5 and 14 patients received intravenous Ondansetron and Metoclopramide (Plasil), respectively. Among the seven patients suffering from vomiting in the Ginger group, 3 and 1 patients were given Ondansetron and Plasil in the recovery room, respectively. The ratio of drug administration to control vomiting in the recovery room was also significantly lower in the Ginger group (P = 0.003).
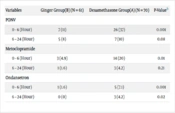
Data on the frequency of vomiting in the first 24 hours after surgery were also obtained. The frequency of vomiting was 47% (33 patients) and 19.7% (12 patients) in the Dexamethasone and Ginger groups, respectively (P = 0.001). Twenty-five patients (38%) in the Dexamethasone group and 5 (8.2%) in the Ginger group were treated with intravenous medications such as Ondansetron or Metoclopramide in the first 24 hours after surgery (P = 0.001). The severity of nausea was lower in the Ginger group than in the Dexamethasone group during the first 6 hours following surgery (Table 2).
| Variables | Ginger Group(B) (N = 61) | Dexamethasone Group(A) (N = 70) | P-Valueb |
| PONV | |||
| 0 - 6 (Hour) | 7 (11) | 26 (37) | 0.001 |
| 6 – 24 (Hour) | 5 (8) | 7 (10) | 0.08 |
| Metoclopramide | |||
| 0 - 6 (Hour) | 3 (4.9) | 14 (20) | 0.01 |
| 6 – 24 (Hour) | 1 (1.6) | 3 (4.2) | 0.21 |
| Ondansetron | |||
| 0 - 6 (Hour) | 1 (1.6) | 5 (7.1) | 0.001 |
| 6 – 24 (Hour) | 0 (0) | 3 (4.2) | 0.02 |
Postoperative Nausea and Vomiting in Ginger and Dexamethasone Groups and Supplement Treatment a
No significant side effects were observed in either the Dexamethasone or Ginger groups. The mean hemoglobin drop after 6 and 24 hours was not significantly different between the two groups; after 3 hours, it was 1.14 vs. 1.08 for Ginger vs. Dexamethasone, respectively (P = 0.34), and after 24 hours, it was 1.35 vs. 1.24, respectively (P = 0.215). Three patients in each group required blood transfusion, indicating no significant difference (P=0.185). All patients were asked about post-surgical pain and discomfort using the VAS, which indicated no significant difference between the two groups (P = 0.45).
5. Discussion
Postoperative nausea and vomiting are common and distressing side effects of various surgical procedures. Postoperative nausea and vomiting occurs in 20 - 40% of patients receiving postoperative opioids. In cases of inadequate antiemetic prophylaxis, the incidence of PONV may increase by about 80 percent (4-6).
Patients undergoing laparoscopic procedures more commonly experience severe types of PONV (19). This can be attributed to the increased probability of vagal stimulation (directly or secondary to gas irritation) or intra-peritoneal manipulation of the gastrointestinal system, leading to decreased alimentary tract motility (19, 20).
Although PONV might not result in severe medical complications (such as gastric herniation, electrolyte imbalance, dehydration, wound disruption, and esophageal tearing), it imposes extra stress on patients who have already undergone major surgery. Several medications, such as Metoclopramide, Ondansetron, and Dexamethasone, commonly used for the treatment of nausea and vomiting, have also been utilized in different studies as "premedication" to prevent PONV. Due to the prevalence of PONV, using a safe and inexpensive medicine before surgery may lead to a reduction in patients' distress after surgery (13, 14). Dexamethasone, primarily prescribed for the treatment of vomiting secondary to chemotherapy medications, may produce endogenous prostaglandins and opioids, resulting in reduced pain and nausea after surgery (21, 22). A meta-analysis has indicated that the rate and severity of PONV can be lowered by Dexamethasone within 24 hours of surgery and, therefore, can be used as routine premedication against PONV (23).
Ginger root, officially known as "zingiber officinale," has been traditionally used in China to treat motion sickness and hyperemesis gravidarum (24, 25). Studies have identified gingerols, particularly 6-Gingerol, as the significant active compound in ginger root (24). While several studies suggest that 6-Gingerol enhances active transport in the digestive system (26, 27), others, like the one conducted by Philips and colleagues, have concluded that ginger does not improve gastric emptying rate in humans (28). Nevertheless, 6-Gingerol and another active ingredient in ginger, galanolactone, act as competitive antagonists for 5-hydroxytryptamine (5-HT) receptors in the gastrointestinal system (26, 29), leading to the suppression of nausea and vomiting (30).
Some studies propose that ginger may act via receptors in the central nervous system (CNS) (29). For example, research by Yamahara et al. demonstrated that 6-Gingerol might suppress cyclophosphamide-induced vomiting in animal models (31). However, a study led by Holtmann and colleagues challenged the notion that ginger directly affects the vestibular and oculomotor systems (32).
Previous randomized clinical trials (RCT) comparing ginger to placebo have been conducted. In our study, we compared the effect of ginger on PONV to intravenous dexamethasone. The results showed that the frequency of vomiting in the first 24 hours after surgery was significantly lower in the ginger group than in the dexamethasone group (P = 0.001).
Arfeen et al. indicated that Ginger powder does not improve PONV after laparoscopic gynecological procedures (33). Another study by Kalava et al. revealed that Ginger is ineffective in reducing the incidence of nausea and vomiting during and after surgery (13). These studies do not support the findings of our research.
On the other hand, Nanthakomon et al. indicated that Ginger, compared to placebo, can reduce PONV (34). Another study carried out in Thailand revealed similar results (35). A meta-analysis study on Ginger as a premedication has concluded that 1 gram of Ginger powder effectively prevents PONV following gynecologic surgery (36).
Most of the studies that have used Ginger as a premedication have been in obstetrics and gynecology (34, 37). To the best of our knowledge, in the field of urologic laparoscopy, only a few studies have been conducted to evaluate the effect of Ginger. Since laparoscopic nephrectomy is usually performed via a transperitoneal approach, involving manipulation of the colon, small intestine, and high levels of vagal stimulation during surgery, there may be differences compared to laparoscopic gynecology, which is typically limited to the pelvic cavity. These variations could lead to different mechanisms and prevalence of PONV. Therefore, further research is recommended in the future to clarify this issue.
5.1. Limitation
Our research had a few limitations, such as a small sample size and a single-center design.
5.2. Conclusions
Ginger (500 mg oral capsule) can reduce the incidence of nausea and vomiting after laparoscopic nephrectomy compared to Dexamethasone, which is one of the standard treatments for PONV.