1. Background
Intraoperative hemorrhage is a potential complication in surgical procedures, posing significant challenges for surgeons and anesthesiologists (1). Attention to intraoperative and postoperative hemorrhage is crucial, and its source should be promptly controlled (2). Heavy bleeding typically occurs after more extensive operations (3). Spinal surgery, often characterized by a significant intraoperative hemorrhage, may be attributed partly to factors such as large surgical incisions, prolonged operation duration, and increased involvement of cancellous bone (4). Intraoperative and postoperative hemorrhage can lead to heightened coagulation, postoperative hematoma, anemia, and the need for allogeneic blood transfusion, which may result in complications like hemolytic and non-hemolytic reactions, acute lung injury, transmission of viral and bacterial infections, hypothermia, and coagulation disorders (5), incurring costs for both families and society. The economic burden of blood loss includes direct costs, such as blood products and intraoperative hemorrhage control technology, as well as indirect costs like long-term patient hospitalization and complication management (6, 7).
Numerous studies have aimed to reduce hemorrhage during spine fusion surgeries using various medications, including aprotinin, aminocaproic acid, tranexamic acid, and modified factor VII (8, 9). Standard anesthesia techniques and arterial blood pressure control play significant roles in preventing excessive intraoperative hemorrhage. The correlation between intraoperative hypotension and reduced intraoperative hemorrhage has been extensively documented, highlighting the importance of lowering blood pressure to minimize blood loss (10-12). Alpha-2 adrenergic agonists such as clonidine and dexmedetomidine, with distinct mechanisms of action compared to other anesthetics, have been studied for their effects on hemodynamic stability. Clonidine, an imidazole derivative, exerts agonistic effects on alpha-2 adrenergic receptors, is well absorbed orally, reaches peak effect in 60 - 90 minutes, and has an elimination half-life of 9 - 12 hours. Low-dose clonidine infusion intravenously reduces mean arterial pressure by activating central and peripheral alpha-2 receptors, while high doses through intravenous infusion or rapid intravenous bolus may elevate systemic blood pressure by activating peripheral alpha-1 adrenergic receptors post-binding (9).
Singh et al. (13) assessed the effects of clonidine versus atenolol on improving surgical visibility, reducing intraoperative blood loss, and maintaining hemodynamic stability in rhinoplasty under general anesthesia. Their study involved 60 ASA grade I and II patients undergoing rhinoplasty, randomly assigned to two groups of 30 people. Two hours before surgery, group A received 50 mg of oral atenolol, while group B received 100 μg of oral clonidine. Results showed that heart rate (HR) and blood pressure remained within normal ranges in both groups throughout the surgery. Patients who received clonidine experienced less blood loss, and surgeons reported better visibility during the operation. Bajaj et al. (14) investigated clonidine's efficacy and safety in reducing blood loss during pituitary adenoma surgery. The study included 50 patients with pituitary adenoma randomly divided into two groups. Group A (25 patients) received oral clonidine (200 μg), while group B (25 patients) received a placebo. Clonidine was found to be a safe and effective agent for reducing hemorrhage in microscopic transsphenoidal pituitary adenoma surgeries.
Ebneshahidi and Mohseni (9) examined the impact of oral clonidine on reducing intraoperative hemorrhage and maintaining hemodynamic stability during cesarean section under general anesthesia. They observed significantly lower blood loss and reduced narcotic requirements in the clonidine-treated group compared to the placebo group. Deepa and Shekhar (15) investigated the effects of pre-medication with intravenous clonidine on modulating hemodynamic responses during laparoscopic surgeries in 60 patients. Patients were divided into two groups: One group received 2 μg/kg of intravenous clonidine, while the second group received a placebo. Their findings indicated that patients pre-medicated with intravenous clonidine exhibited stable hemodynamics and improved analgesia and sedation compared to those who did not receive clonidine.
Overall, pre-medication with clonidine has been shown to significantly enhance patient stability during and after surgery across various procedures. Given its efficacy in reducing hemorrhage in multiple surgeries and its positive effects in thoracic spine trauma surgery, we aimed to evaluate its impact on bleeding volume in patients undergoing lumbar laminectomy with pedicle screw fixation for lumbar disc herniation. By mitigating side effects and reducing hospitalization duration and associated costs for families and society, widespread adoption of this approach can be justified based on the findings of this field study.
1.1. Fusion Surgery
Spinal fusion is performed to correct deformities or relieve back pain and is recommended for diseases such as degenerative scoliosis, spondylolisthesis, and vertebral fractures causing spinal instability. Additionally, fusion surgery is used in conditions such as tumors, spinal canal stenosis, disc herniation, and spinal weakness or instability caused by diseases like arthritis (spondylosis).
1.2. Clonidine
Clonidine is an imidazole derivative drug that has an agonistic effect on alpha-2 adrenergic receptors. Clonidine is well absorbed orally, with an onset of effect around 30 - 60 minutes, a peak effect at 60 - 90 minutes, and a half-life of 9 - 12 hours. In the central nervous system and in the presynaptic location of nerves, clonidine inhibits the secretion and release of the neurotransmitter norepinephrine, thereby having an inhibitory effect on the sympathetic system.
1.3. Dexmedetomidine
It is an alpha-2 adrenergic agonist with sedative, anxiolytic, hypnotic, analgesic, and sympatholytic effects. It is metabolized in the liver and excreted through urine and feces.
2. Methods
2.1. Study Population, Clinical Design, and Disposition
This study was conducted at the educational-therapeutic center of Imam Reza, Tabriz, between January 2020 and July 2020, involving patients referred to the hospital's operating room for laminectomy surgery with pedicle screw insertion (as a fusion procedure) due to lumbar intervertebral disc herniation. Written and informed consent was obtained from all patients, and their information remained confidential. The study received approval from the local ethics committee of Tabriz University of Medical Sciences (IR.TBZMED.REC.1398.936) and was registered at the Iranian Registry of Clinical Trials (IRCT20140107016117N4).
The sample size was estimated to be 100 patients aged 20 - 60 years, selected through a convenience consecutive method based on the order of patients visiting the operating room. Inclusion criteria were ASA class I - II patients aged 20 - 60 years, candidates for laminectomy with pedicle screw fixation. Exclusion criteria included patients with systemic diseases (cardiovascular, cerebral, renal, liver, and kidney), blood loss exceeding 10% in hypertensive patients, diabetic patients, and non-use of medications that interfere with clonidine, such as ibuprofen, losartan, beta-blockers, diazepam, and vitamin B12 (16, 17).
Patients were randomly assigned to two groups (intervention and control). The intervention group received a clonidine tablet (0.2 mg) one hour before entering the operating room with half a glass of water in the ward and then were transferred to the operating room. No pill was administered to the control group. Both patients and anesthesiologists were blinded to the drug (clonidine). All procedures were managed by a resident anesthesiologist. In the operating room, all patients received intravenous midazolam (2 mg) and fentanyl (100 μg), followed by induction of anesthesia using propofol (2 mg/kg), cis-atracurium (0.15 mg/kg), and lidocaine (1 mg/kg). Three minutes after anesthesia induction y monitoring HR, blood pressure, O2 sat, and electrocardiogram (ECG), patients were intubated with a cuffed spiral tube (inner diameter 8 mm in men and 7.5 mm in women). Anesthesia was maintained with nitrous oxide 3 L/min and O2 3 L/min, isoflurane 1%, and remifentanil infusion (0.05 μg/kg/min). Blood pressure and HR were recorded before anesthesia, after anesthesia induction, 1 minute and 3 minutes after intubation, 1 minute after surgical incision, and then every 15 minutes until recovery. If blood pressure exceeded 150/100 despite anesthesia, intravenous nitroglycerin (TNG) infusion was used to reduce blood pressure, and the amount used was recorded. The hemodynamic status of the patient and the amount of TNG used were compared between the two groups.
2.2. Statistical Analysis
The data were expressed using descriptive statistics (mean ± standard deviation and frequency percentage) and analyzed using paired-samples t-test, repeated-measures ANOVA, and independent t-test. Normal distribution of data was assessed using the Kolmogorov–Smirnov test. SPSS 22 software was used for data analysis, and a P-value < 0.05 was considered statistically significant.
3. Results
Patient demographics are displayed in Table 1, indicating no statistically significant difference between the two groups. Additionally, regarding sex distribution, sixty cases (60%) were male, and 40 cases (40%) were female, with males showing the highest frequency in both groups. Concerning physical condition and ASA class, 88% of the patients were classified as class I, and 12% as class II, with no significant difference between the two groups (P = 0.067).
| Variables | No. | Mean ± SD | P-Value |
|---|---|---|---|
| Height (cm) | |||
| Control | 50 | 164.7 ± 4.1 | 0.560 |
| Clonidine | 50 | 163.8 ± 4.1 | 0.560 |
| Weight (kg) | |||
| Control | 50 | 79.2 ± 5.82 | 0.245 |
| Clonidine | 50 | 81.4 ± 4.80 | 0.245 |
| BMI (kg/m2) | |||
| Control | 50 | 27.3 ± 2.05 | 0.468 |
| Clonidine | 50 | 27.5 ± 1.92 | 0.468 |
| Age (y) | |||
| Control | 50 | 43.6 ± 6.73 | 0.237 |
| Clonidine | 50 | 41.6 ± 3.39 | 0.237 |
Surveys indicated that the surgery duration in the clonidine group lasted 110 minutes, while the average for the control group was 170 minutes, and this difference was statistically significant. The total dose of remifentanil infusion in the clonidine and control groups was 50.7 ± 69 and 623 ± 13, respectively, and this difference was statistically significant (P = 0.01). TNG was not used in either of the two groups.
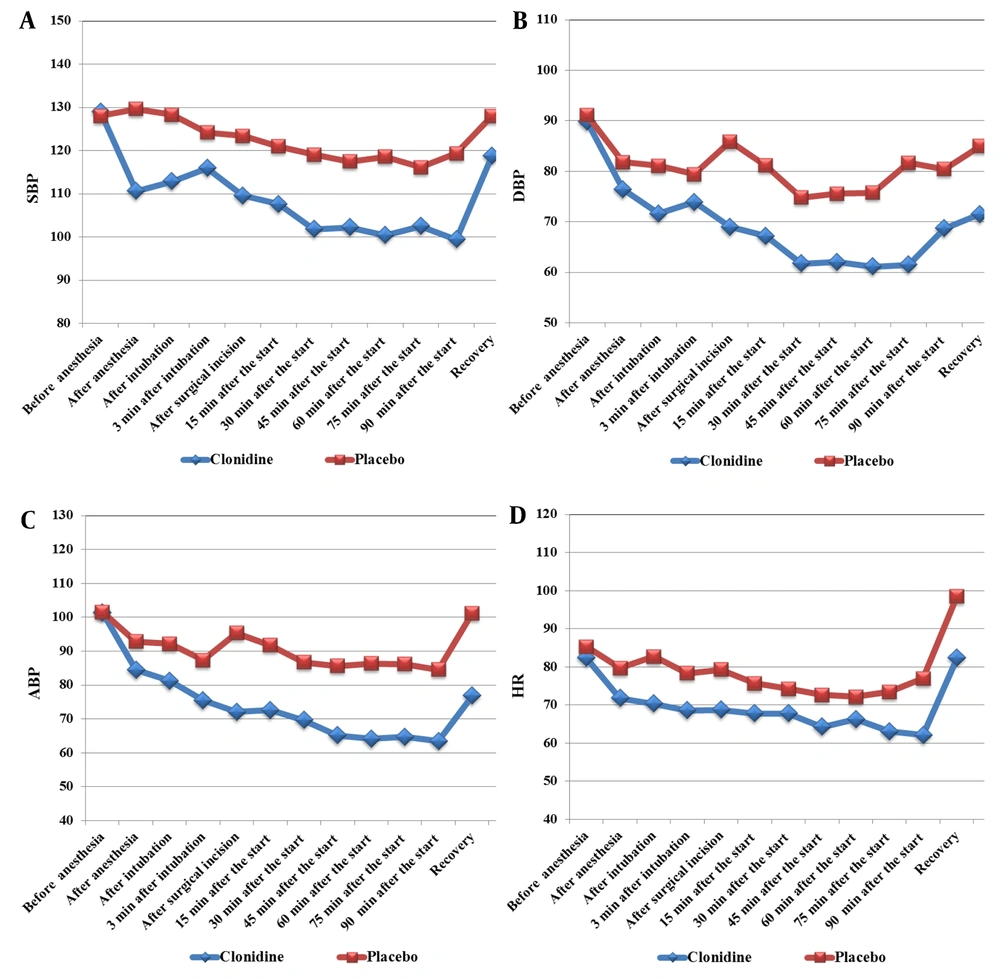
Figure 1A shows that mean systolic blood pressure (SBP) in the clonidine group decreased after induction of anesthesia, after intubation, and during surgery compared to the control group, and this decrease was significant. Figure 1B show that similar to SBP, in the clonidine group, the mean diastolic blood pressure (DBP) significantly reduced after induction of anesthesia, after intubation and during surgery. According to Figure 1C, in the clonidine group, the average blood pressure (ABP) values were significantly reduced compared to the control group. Figure 1D shows that the average HR in the clonidine group decreased significantly after intubation, during surgery and recovery compared to the control group. Also, Table 2 shows the average standard deviations for SBP, DBP, ABP and HR values.
| Result | Average Deviation Control Group | Average Deviation Clonidine Group | P-Value |
|---|---|---|---|
| SBP | ± 14.2 | ± 15.1 | 0.04 |
| DBP | ± 12.2 | ± 13.4 | 0.03 |
| ABP | ± 14.5 | ± 15.5 | 0.04 |
| HR | ± 12.3 | ± 13.8 | 0.03 |
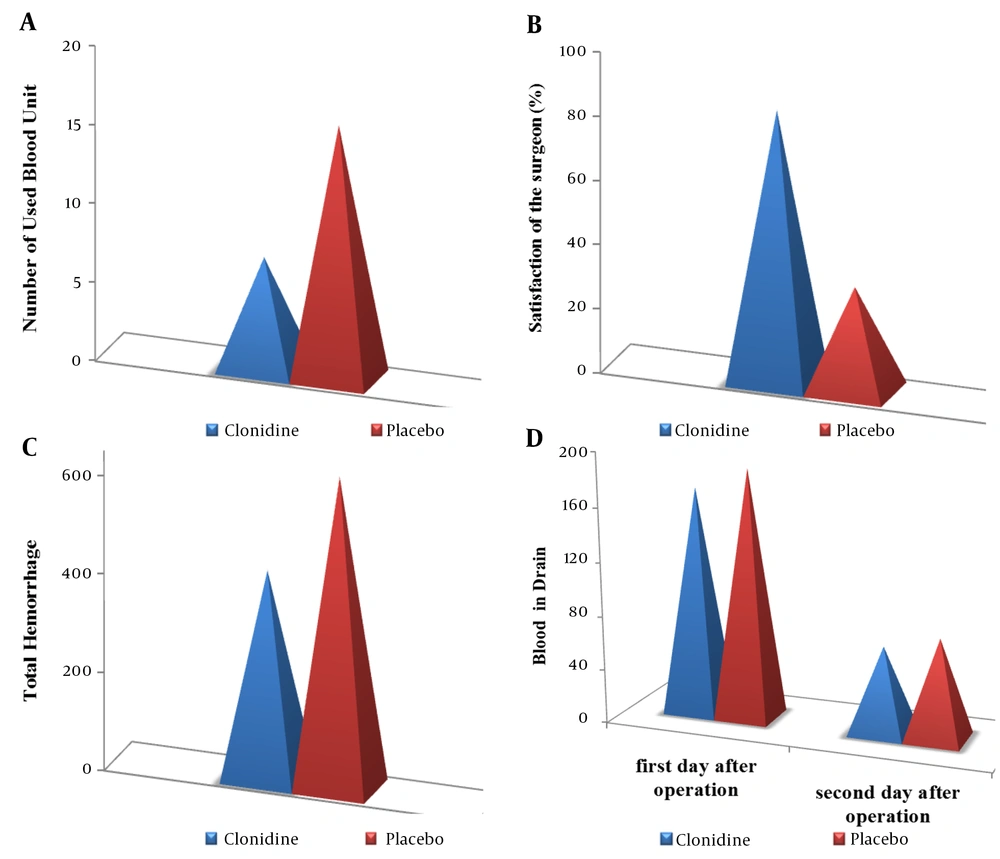
The average amount of blood transfusion in the clonidine and control groups was 7 and 16 units, respectively, and a significant difference was observed between the two groups (P = 0.02) (Figure 2A). Regarding surgeon satisfaction, 84% of surgeons in the clonidine group and 32% in the control group were satisfied, and there was a significant difference between the two groups (Figure 2B) (P = 0.04). Additionally, the results showed that hemorrhage in the clonidine group decreased by 34.5% (Figure 2C) (P = 0.05). According to Figure 2D, there was no significant difference between the groups in the amount of blood in the drains on the first and second days after the surgery (P = 0.80 and P = 0.73).
4. Discussion
Using alpha-2 agonist drugs, such as clonidine and dexmedetomidine, is one of the methods to prevent hemodynamic instability and reduce intraoperative hemorrhage. Alpha-2 agonist drugs are sympatholytic and affect central receptors to reduce peripheral norepinephrine release (5). Only a few studies have been conducted on the effect of alpha-2 agonist drugs, especially clonidine, on hemodynamic response and intraoperative hemorrhage.
In this study, we investigated the effect of oral clonidine on hemorrhage in patients undergoing fusion surgery using the data of 100 patients undergoing fusion surgery. The effectiveness of clonidine was evidenced by a significant reduction in operation time and the amount of hemorrhage. This reduction in hemorrhage can be explained by the pharmacological effect of the drug. Clonidine is a selective alpha-2 adrenergic receptor agonist and when consumed orally, it is rapidly absorbed and reaches its maximum level in 60 to 90 minutes, and its half-life is between 9 and 12 hours. This drug causes vasoconstriction by acting on alpha-2 receptors through its sympatholytic effect. It also has receptors in the brain stem, which causes a decrease in blood pressure and bradycardia (14).
The results showed that in the clonidine group, the mean SBP, DBP, mean arterial pressure (MAP), and HR significantly decreased after induction of anesthesia, after intubation, at seven different time points from 15 minutes after intubation to 90 min after the operation, and also in the recovery. Also, total blood loss was reduced in the clonidine group. The amount of blood and fluid collected from the drains was less in the patients who received clonidine, and as a result, the amount of blood transfusion in the patients in the clonidine group was lower than in the control group.
Regarding previous studies, clonidine reduced intraoperative hemodynamic stability more than dexmedetomidine (18). Pandazi et al. (19) studied low-dose clonidine premedication and hypotension after carotid artery surgery and concluded that intravenous premedication with low-dose clonidine (1 μg/kg) is effective in preventing hypertensive attacks during carotid endarterectomy under general anesthesia. However, clonidine seemed to increase the incidence of postoperative hypotension possibility. Similar results were also reported by other researchers (20). They declared that clonidine as a selective alpha-2 agonist, is a central sympatholytic, which can significantly cause hemodynamic stability and dose-dependently reduce HR and blood pressure.
The effectiveness of clonidine in reducing hemorrhage and blood transfusion reduced doubts and concerns about blood transfusion complications. No complications or adverse outcomes were observed in our study. In this study, SBP, DBP, ABP, and HR were lower in the clonidine group, so the amount of remifentanil given to control BP and HR was significantly lower in the clonidine group. This finding is consistent with that of Okuyama et al. (21), who observed that clonidine has a favorable effect on hemodynamic stability and analgesia. Also, the duration of surgery was significantly shorter in the clonidine group, which may be due to the favorable hemorrhage control leading to the improved field of vision. In addition to estimating the amount of blood loss, the satisfaction of the surgical team was also assessed (22, 23). The surgeon was satisfied with the bloodless operative field in 42 cases (84%) in the clonidine group compared to 16 cases (32%) in the control group, and this difference was statistically significant (P = 0.05).
4.1. Conclusions
In this study, the effect of using clonidine as a pre-anesthetic medicine on patients who underwent lumbar laminectomy with pedicular screws was studied, and the most remarkable findings are listed below:
- The preventive use of oral clonidine before surgery was effective in reducing blood loss during and after spine surgery.
- Clonidine reduced the amount of blood transfusion to patients and its related complications.
- Surgeon satisfaction was significantly higher in the intervention group compared to the control group.
- SBP, DBP, ABP, and mean HR were significantly reduced, indicating higher hemodynamic stability during surgery and recovery.