1. Introduction
Airway management in trauma patients presents unique challenges extending beyond the mere placement of an endotracheal tube (ETT). Successful outcomes hinge on the healthcare provider's ability to anticipate difficulties and formulate a safe and actionable plan (1).
Anatomical markers, such as mouth opening, a small inter-incisor gap, prominent incisors, a large tongue, retrognathia, large neck circumference, and increased pre-tracheal soft tissue, generally serve as poor predictors of difficult airway management (2). Trauma pathophysiology introduces an additional layer of complexity and challenges for trauma patients. The term "physiologically difficult airway" encompasses non-anatomic patient variables, such as hypoxemia, hypocapnia, and hypotension, which can influence airway management outcomes (1, 3). Therefore, both anatomical and physiological factors should be taken into account in all trauma patients to mitigate the risk of devastating consequences during the peri-intubation period, ideally addressing them as part of the airway plan (2, 4).
Understanding the timing and reasons behind difficulties encountered by healthcare providers in airway management for trauma patients can inform the development of specific mitigation strategies and contingency plans. Calling for assistance should always be regarded as a patient-centered measure.
Maxillofacial fractures can impact airway management in various ways. Displacement of maxillofacial fracture segments may lead to soft tissue collapse and airway occlusion, further compounded by the presence of a cervical spine collar. Significant bleeding can pose a challenge during airway management, exacerbated by blood pooling in the oropharynx in the supine position, potentially triggering a gag reflex or vomiting, thereby exacerbating bleeding. Some maxillofacial fractures may also cause trismus, which can be alleviated using neuromuscular blocking agents. However, it is essential to differentiate it from mechanical obstruction before intubation (1, 2, 5).
Due to the increased mobility of the mandible and associated soft tissues, mandibular fractures occurring in two or more locations may render intubation easier; however, concomitant condylar fractures may cause mechanical obstruction, resulting in limited mouth opening, thereby complicating laryngoscopy and intubation (1, 2).
A thorough assessment of the patient's condition is the initial step in airway management. Healthcare providers should anticipate that pre-oxygenation in patients with craniofacial injuries will pose challenges, and that reoxygenation using bag-mask ventilation during rapid sequence induction (RSI) may be difficult or impossible if the initial attempt fails. Distortion of facial architecture may hinder proper sealing of the mask, and patients may tolerate positive pressure ventilation poorly due to tissue displacement, potentially exacerbating bleeding (1). Lower airway injuries can also lead to significant subcutaneous emphysema. During RSI, healthcare personnel must be mindful that structural airway collapse may occur, leading to difficulties in oxygenation and ventilation (2, 3).
The approach to airway management will hinge on the patient's ability to maintain a clear airway. If a patient's oxygenation remains satisfactory, physicians should conduct a targeted physical examination to ascertain the specific pattern of facial injury and plan accordingly. Given the anticipated difficult airway in maxillofacial trauma cases, challenges with intubation, mask ventilation, rescue with supraglottic airway devices, and maintaining spontaneous respiration during airway securing attempts should be anticipated (6).
The same general trauma management principles should be applied to pregnant patients, with certain necessary modifications. Perioperative anesthetic considerations encompass the safety of both the mother and fetus, accounting for physiological and anatomical changes during pregnancy, anticipating a difficult airway due to maxillofacial trauma compounded by pregnancy, the risk of utero-placental insufficiency, exposure of the fetus to anesthetic agents, and the risk of preterm delivery.
2. Case Presentation
A 20-year-old female patient was brought to the trauma center with an injury to the left side of her face and jaw pain following a history of a portion of the roof falling on her head. The patient's attendant reported loss of consciousness for 15 - 20 minutes following the trauma. On arrival, primary and secondary surveys were conducted according to Advanced Trauma Life Support guidelines. The cervical spine was stabilized, and there was no airway compromise or breathing disturbance. The patient had a Glasgow Coma Scale score of 15/15, and vital signs were within the normal range. Apart from the degloving injury over the forehead, left eyelid, and root of the nose (Figure 1), there were no other visible external injuries. Blood samples were collected, and the patient received intravenous fluids. A urinary catheter was inserted. Further history revealed that the patient was a primigravida with 5 months of amenorrhea. Chest and pelvic X-rays, performed with an abdominal shield, showed no abnormalities. Ultrasonography for fetal activity indicated a single, live intrauterine fetus with a fetal heart rate of 125 beats per minute.
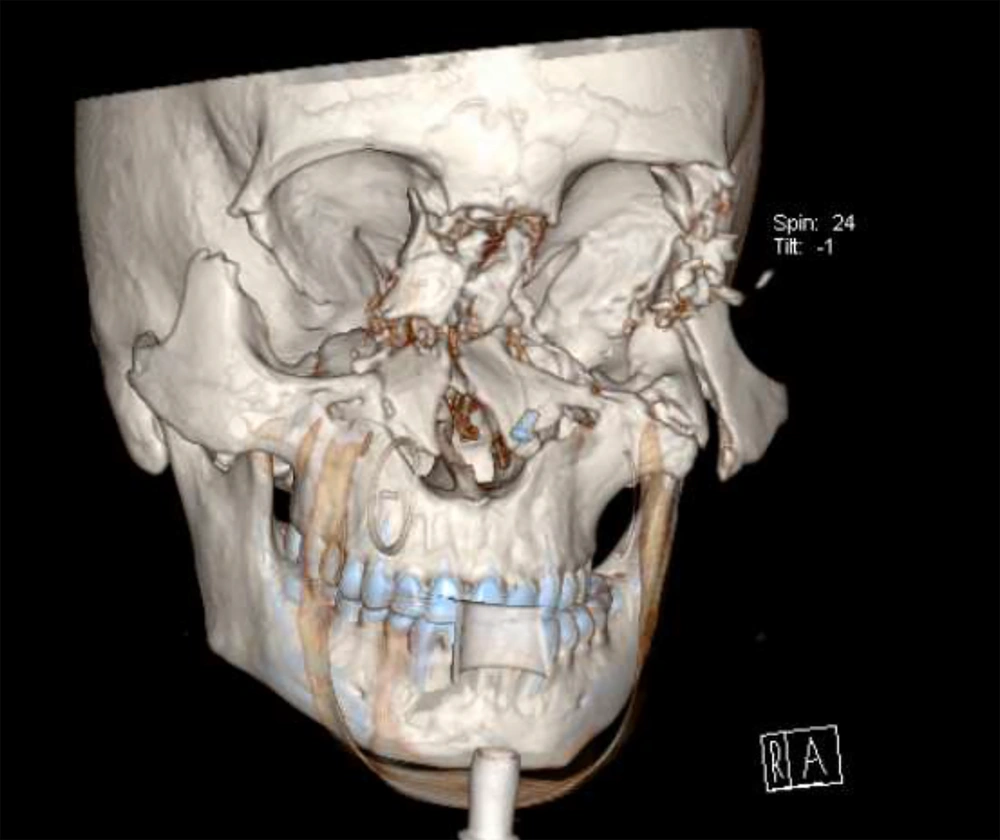
Further investigation revealed a left-sided sphenoid fracture, bilateral zygomatic bone and pterygoid plate fractures, Lefort 3 fracture, ethmoidal comminuted fracture, and a left orbital medial wall fracture, along with entrapment and rupture of the extraocular muscles (Figure 2). The patient was scheduled for open reduction and internal fixation of pan-facial fractures and primary repair of a lacerated wound under general anesthesia.
During the preoperative examination, a restricted mouth opening of approximately 1.5 cm was noted. Laboratory investigations revealed a hemoglobin level of 7.2 g/dL, for which 1 unit of packed red blood cells was transfused preoperatively. All routine investigations were within normal limits. Adequate fasting was confirmed, and high-risk consent for surgery and anesthesia was obtained due to the anticipated difficult airway, risk of aspiration, need for postoperative mechanical ventilation, preterm labor, and fetal loss.
A standby team for emergency tracheostomies was kept ready, and all essential monitoring requirements for the case were attached. The patient was preoxygenated with 100% oxygen for 3 - 5 minutes. Anesthesia was induced with sevoflurane and 100% oxygen while maintaining spontaneous respiration. After achieving adequate depth, direct laryngoscopy was performed using the C-MAC® videolaryngoscope (Karl Storz SE & Co. KG, Tuttlingen, Germany), during which the glottis was visualized. Subsequently, a fentanyl bolus of 100 micrograms was administered, followed by an injection of succinylcholine of 100 mg, and the patient was intubated with a 7.5 mm cuffed, flexo-metallic ETT under C-MAC guidance.
Following intubation, submental intubation was performed by the surgeon to provide better access to the surgical field (Figure 3). Throat packing was done by a maxillofacial surgeon to prevent aspiration of blood. Anesthesia was maintained with oxygen, air, and isoflurane, and bolus atracurium was used for muscle relaxation. After completion of the surgical procedure, the submental flexo-metallic ETT was exchanged with a conventional orotracheal tube under C-MAC guidance.
Due to airway surgery and vocal cord edema, the patient was not reversed and was shifted to intensive care with ETT in situ for further management. The patient was weaned and extubated on postoperative day 1, and her subsequent course was uneventful.
Effective trauma care requires a meticulous team approach, with resuscitation priorities clearly communicated and interventions guided by the physiological parameters that ensure adequate oxygen delivery. Although ensuring oxygenation and ventilation are important, they must not overshadow other resuscitative elements (3, 5, 7).
The management of a pregnant patient should maximally benefit the mother and cause minimal harm to the fetus. All life-saving interventions should be done regardless of pregnancy. All pregnant trauma patients should be managed according to Advanced Trauma Life Support (ATLS) guidelines for trauma, with additional mandatory modifications necessary to deal with physiological and anatomical alterations in pregnancy.
Factors leading to a difficult airway during pregnancy include increased tissue vascularity and edema, causing an increased incidence of airway bleeding during intubation; delayed gastric emptying and reduced lower esophageal tone, predisposing to aspiration; and increased breast size and neck adiposity, leading to difficulty in laryngoscopy. Pregnancy causes an increase in oxygen consumption and a decrease in functional residual capacity. All pregnant trauma patients should be given high-flow oxygen in the head-up position (unless contraindicated). Due to increased intravascular volume during pregnancy, the patient may lose 1 - 2 liters of blood before showing signs of hypovolemia. In fact, fetal distress may be the only early indicator of maternal hemorrhage leading to utero-placental insufficiency. After 20 weeks of pregnancy, all women should be placed in the left lateral position to avoid aorto-caval compression. Vasopressors should be avoided as they decrease placental perfusion. An obstetric examination is to be done once the patient is stabilized to assess fetal well-being, gestational age, and to rule out any complications of pregnancy. Once the patient is stabilized and obstetric complications have been ruled out, the patient may be taken up for emergency surgery, as conservative management of such a maxillofacial injury would lead to a risk of aspiration, airway edema, and infection and can affect the nutritional status of the mother and the fetus (8, 9).
Among maxillofacial traumas, nasal fractures are the most common, followed by mandibular fractures. Soft tissue injury, loss of facial bone framework, and malocclusion are all common complications of pan facial fractures, which further restrict mouth opening and increase airway edema. The first and foremost complication seen in maxillofacial trauma is a compromised airway. Additionally, an associated cervical spine injury may add further difficulties. It may be aggravated by diminished consciousness, alcohol, and/or drug intoxication. Airway management in such scenarios should be done following difficult airway society guidelines (3, 6).
The airway management of trauma patients is highly variable. It will depend on several factors, such as patient characteristics, medical and surgical history, airway examination, the patient’s current status and vital signs, and the clinical context in which airway management is required, like in any planned surgery. Appropriate training, experience, risk assessment, and clinical judgment are seen as essential to reliably predicting the difficulty of a patient’s airway. When there is an anticipated difficult airway, there are a number of options that need to be considered (10). Regional anesthesia is preferred over general anesthesia whenever possible. However, in patients who require general anesthesia with intubation, an awake intubation technique should be considered. If laryngeal structures are easily seen during check laryngoscopy after awake sedation, general anesthesia may be induced, and the patient can be intubated conventionally. This allows the patient to maintain their own airway (11).
3. Discussion
Patients with maxillofacial injuries require a thorough assessment of the injured airway anatomy as well as recognition of the particular airway problems associated with facial fractures. When such patients are pregnant, the situation becomes more challenging. Therefore, during managing the airway, an "awake" approach or a check laryngoscopy while maintaining spontaneous respiration, where feasible, should be considered.