1. Background
Hip surgeries are among the most common orthopedic procedures, and managing postoperative pain in these cases can be a significant challenge. Effective postoperative pain management and early recovery are crucial for achieving optimal functional outcomes in hip joint surgeries (1).
Lumbar epidurals, fascia iliaca compartment blocks (FICB), and femoral blocks have been used for postoperative analgesia (2). However, these techniques have proven insufficient for complete pain relief and are often associated with lower limb weakness, which can impair the basic mobility of patients (3). Recently, the pericapsular nerve group block (PENG) has emerged as a promising alternative for managing postoperative pain following hip fracture surgery. The PENG block targets the obturator nerve, lateral obturator nerve, and femoral nerve, which innervate the anterior hip capsule (4).
Previous studies comparing the effectiveness of PENG to FICB have yielded contradictory results, highlighting the need for further research (5-10).
2. Objectives
This study aims to investigate and compare the effects of PENG and FICB on reducing postoperative pain in intertrochanteric hip surgery.
3. Methods
This double-blind clinical trial was conducted in the operating room of Hazrat-e-Rasoul Educational-Therapeutic Center of Iran University of Medical Sciences. The study population included patients aged 40 to 80 years who were candidates for intertrochanteric fracture surgery and were classified as ASA I to III according to the American Society of Anesthesiologists (ASA) classification. Exclusion criteria comprised candidates for emergency surgery, individuals with a history of sensitivity to ropivacaine, liver or lung disease, a Body Mass Index over 40, blood coagulation disorders (platelet count below 100,000, PT more than 3 seconds above the normal limit, or PTT more than 1.5 times the normal limit), and drug addiction. Written consent was obtained from all patients after reducing analgesia and immobility levels. The study was approved by the ethics committee of Iran University of Medical Sciences (IR.IUMS.FMD.REC.1400.067) and registered with the Iranian Registry of Clinical Trials (IRCT20141127020112N11).
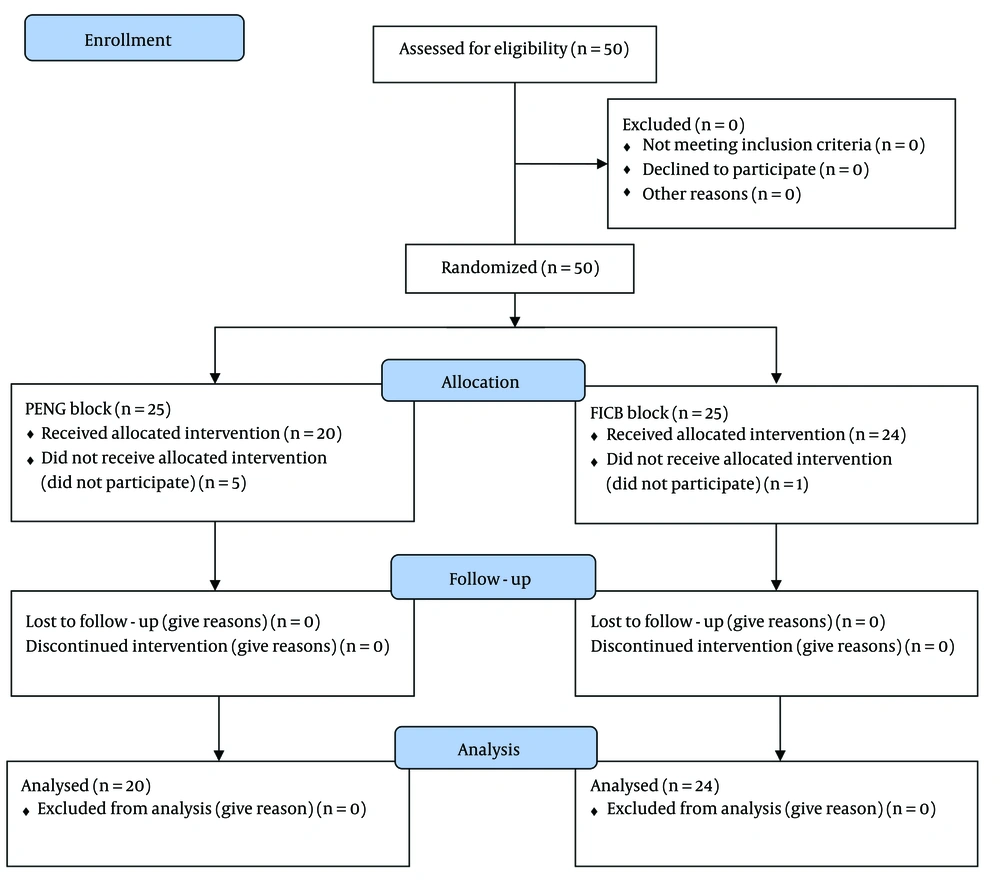
The sample size was estimated based on previous studies, which reported mean pain reductions of 4 units for PENG and 3.1 units for FICB. Using these findings, a sample size of 20 was calculated for each group. To account for a 10% dropout rate, the final sample size was set at 25 per group.
Patients were randomly assigned to the PENG and ultrasound-guided FICB groups using block randomization. In the operating room, patients were monitored using pulse oximetry (POM), ECG, and non-invasive blood pressure (NIBP). After administering 5 mL/kg of Ringer's lactate, spinal analgesia was performed with 2.5 mL of 0.5% Bupivacaine plus 25 micrograms of fentanyl, given in the lateral position. Surgery commenced once the anesthesia level reached T10, as confirmed by a pinprick test. If the systolic blood pressure dropped more than 20% from the initial value or fell below 80 mmHg, 10 milligrams of ephedrine were injected. If the heart rate dropped below 50 beats per minute, 0.5 mg of atropine was administered. Fluid therapy and blood transfusion volumes were calculated according to standard methods.
After surgery, the patient was moved to the recovery room. The sensory block from the spinal anesthesia was then confirmed using the pinprick method, with sensory levels detected below L1. Patients were grouped once the motor block level decreased enough to allow ankle dorsiflexion, and the targeted nerve block was administered using the specified methods.
For the pericapsular block group, the ultrasound probe (MHZ 15_6) was initially placed parallel to the inguinal ligament at the anterior superior iliac spine, then moved caudally toward the anterior inferior iliac spine. After reaching the anterior inferior iliac spine, the probe was rotated medially to visualize the hyperechoic shadow of the upper ramus pubis. The probe was fixed in this position, and the injection space between the anterior inferior iliac spine and the upper ramus pubis was targeted. Here, 20 mL of 0.25% Ropivacaine was injected using a 22 G needle.
For the ultrasound-guided FICB group, the linear probe was placed transversely above the inguinal ligament. The needle was inserted medially to inject 20 mL of 0.25% Ropivacaine into the space between the fascia iliaca and iliacus muscle. An intravenous pain control pump containing 1 mcg/kg/hr fentanyl was set up for both groups to administer 6 mL/h or 1 mL bolus with a lock period of 15 minutes.
Blinding was achieved by ensuring patients were unaware of the syringe contents during the injection, and the anesthesia resident evaluating and measuring pain was also unaware of the block type. When the VAS score was greater than 3, 0.1 mg/kg of morphine was administered intravenously and recorded.
The main outcome was the VAS score, measured immediately after blocks (30 minutes), and at 2, 6, 18, and 24-hours post-surgery. Additional variables included the time of the first morphine request, the amount of excessive morphine consumption 24 hours after surgery, and any complications during the block (bleeding, vascular damage, nerve damage), as well as nausea and vomiting within 24 hours of the block.
Quantitative findings were reported as mean and standard deviation, while qualitative findings were reported as frequency and percentage. The independent t-test was used to assess differences between the two groups at various intervals. Repeated measures tests were used to analyze intragroup variations. A multiple linear regression model was employed to examine pain changes and the effect of removing confounding variables. All tests were conducted at a significance level of 0.05. Statistical analyses were performed using Stata 14.1.
4. Results
This study involved 50 patients undergoing surgery for intertrochanteric fractures. None of the patients were excluded based on the exclusion criteria. The patients were randomized into two groups: The Pericapsular Nerve Block (PENG) group and the Fascia Iliaca Compartment Block group, each consisting of 25 subjects. In the PENG group, a block was performed for 20 patients, while 5 patients were excluded from the study due to the need for general anesthesia during the operation. In the FICB group, a block was performed for 24 patients, and one patient was excluded due to the need for general anesthesia during the operation (Figure 1).
The mean age of patients in the PENG and FICB groups was 65.9 ± 10.8 years and 61.5 ± 14.3 years, respectively. No significant difference was found between the two groups regarding mean age.
In terms of gender distribution, 50% of patients in the PENG group were female, and 50% were male. In the FICB group, 54.1% of patients were female, and 45.9% were male. The Chi-square test showed no significant difference between the two groups in terms of gender (P-value = 0.783).
Regarding physical status, 35% of patients in the PENG group were categorized as ASA index I, 40% as ASA index II, and 35% as ASA index III. In the FICB group, 41.6% of patients were ASA index I, 45.8% were ASA index II, and 12.5% were ASA index III. There was no significant statistical difference between the two groups regarding ASA index status (P-value = 0.562).
No significant difference was found between the PENG and FICB groups regarding pain scores at 2, 6, 18, and 24 hours after surgery. However, the results of the repeated measures test showed a significant reduction in the mean pain score in both groups compared to the start of the study (P-value < 0.001) (Table 1).
| Pain, Interval | PENG | FICB | P-Value |
|---|---|---|---|
| After surgery | 6.2 ± 1.5 | 6.0 ± 1.3 | 0.785 |
| Immediately after the block | 2.3 ± 1.4 | 2.2 ± 1.4 | 0.917 |
| 2 hours after surgery | 2.2 ± 1.4 | 2.1 ± 1.4 | 0.939 |
| 6 hours after surgery | 2.6 ± 1.5 | 2.8 ± 1.5 | 0.627 |
| 18 hours after surgery | 1.8 ± 1.1 | 2.3 ± 1.4 | 0.222 |
| 24 hours after surgery | 1.4 ± 0.6 | 1.8 ± 0.8 | 0.103 |
| Repeated measure P-value | 0.001 | 0.001 |
a Values are expressed as mean ± SD.
The performance of PENG and FICB and the factors affecting them were evaluated using multiple linear regression. This analysis revealed no significant difference between PENG and FICB in terms of pre- and post-block pain (P-value = 0.571).
The only complications observed in this study were nausea and vomiting; no other complications were noted. The incidence rate of vomiting in the PENG and FICB groups was 15% and 8.5%, respectively. The chi-square test showed no significant difference between the two groups regarding vomiting cases (P-value = 0.488).
The mean time for the first request for morphine in the PENG and FICB groups was 9.7 hours and 10.4 hours after surgery, respectively. The difference between the two groups was not statistically significant (P-value = 0.234). No significant difference was found between the PENG and FICB groups regarding mean total morphine consumption.
In the PENG group, 65% of patients requested excessive morphine, compared to 62.5% in the FICB group. No significant difference was found between the two groups (Table 2).
| Variables | PENG | FICB | P-Value |
|---|---|---|---|
| The mean time of the first morphine request by hours | 9.7 ± 1.6 | 10.4 ± 1.8 | 0.234 |
| Mean total morphine consumption (mg) | 9.2 ± 4.3 | 8.3 ± 4.0 | 0.538 |
| Patients required excessive morphine (%) | 65 | 62.5 | 0.875 |
a Values are expressed as mean ± SD.
5. Discussion
The results showed that both PENG and FICB significantly reduced postoperative pain from intertrochanteric fracture surgery. The mean pain score reduction with both blocks was 4 units. Comparison of these methods at 24 hours after surgery showed no significant difference. No statistically significant difference was observed at any interval, including immediately after the block and at 2, 6, 18, and 24 hours.
No significant difference was found between the PENG and FICB groups regarding morphine consumption. Both blocks were safe in terms of complications. The only complications, observed in 11% of patients, were nausea and vomiting, with no significant difference between the PENG and FICB groups in this regard.
The results indicated a significant reduction in the pain score for patients in the PENG group. Pain decreased from a score of 6.2 before the block to 2.3 immediately after, which is consistent with previous studies. Giron-Arango et al. found similar results, showing significant pain reduction 30 minutes after PENG insertion, observed in five patients. Unlike our study, Giron-Arango et al. investigated various types of hip fractures, while our study focused exclusively on intertrochanteric fractures. Additionally, patients in our study received a combination of bupivacaine 0.5% and 25 micrograms of fentanyl, whereas Giron-Arango et al. used bupivacaine with epinephrine (11). Despite these differences, both studies found that PENG significantly reduced postoperative pain.
Kukreja et al. also studied the effectiveness of PENG in reducing postoperative pain and found it to be effective in hip fracture patients. The primary difference between our study and Kukreja et al.'s study was the use of PENG. Our study employed only the PENG block, whereas Kukreja et al. used both PENG and QL (Quadratus Lumborum) blocks simultaneously. Furthermore, Kukreja et al. studied patients undergoing total hip arthroplasty, unlike our study, which focused on intertrochanteric fractures (12). Nevertheless, both studies found that the PENG block effectively reduced postoperative pain in various types of hip fractures.
Our results also showed that using FICB significantly reduced postoperative pain. The pain reduction in patients after the block was from a score of 6 before the block to 2.2 immediately afterward, which aligns with previous studies. In a review of clinical trials, Wan et al. confirmed that FICB is an effective and safe method for reducing pain after hip surgeries. This review of 27 clinical trials found that FICB consistently reduced postoperative pain in patients undergoing hip surgery (13).
Our study compared the effectiveness of PENG and FICB blocks in reducing postoperative pain within the first 24 hours after surgery. Comparing these two methods at various intervals after surgery showed no significant difference. This finding contrasts with those of Krishnamurty et al., who observed a significant difference between the PENG and FICB groups in pain reduction. Their study found that the VAS score 30 minutes after the block was significantly lower in the PENG group compared to the FICB group. They reported that VAS scores for both resting and dynamic hip activity were lower in the PENG group, which differs from our results. The discrepancies in pain measurement indices, timing, drug doses, and procedures may explain the differing results between our study and Krishnamorti et al. (14).
However, Krishnamurty et al. also compared the PENG and FICB methods for postoperative pain management in hip surgery patients and found no significant difference between the two groups, which is consistent with our findings (14).
Current pain management strategies for hip surgeries focus on providing effective analgesia while minimizing mobility limitations. FICB is widely used as a conventional method due to its high effectiveness in pain reduction. The FICB method provides adequate analgesic coverage by targeting the articular branches of the femoral nerve (FN), lateral femoral cutaneous nerve (LTCN), and obturator nerve (ON) near the inferomedial acetabulum, in the space between the anterior inferior iliac spine and iliopubic ridge. Despite its effectiveness, existing evidence indicates that FICB can reduce quadriceps muscle strength, impair basic mobility, and increase the risk of falling after surgery (8, 15).
However, the analgesic approach of the PENG block primarily targets sensory nerves while preserving the strength of the quadriceps muscle. Consequently, this method not only provides excellent pain relief around the thigh but also maintains the patient's mobility with minimal deviation from baseline levels.
According to the literature, the incidence of quadriceps weakness following hip surgeries is significantly lower with the PENG method compared to FICB. This finding is supported by Desmet and Gasanova (3, 16). Despite the importance of this issue, the study did not assess patient mobility or dynamic pain indices, as surgeons did not permit patients to leave their beds or place weight on the operated limb.
Morphine consumption within the first 24 hours post-surgery was another outcome evaluated and compared. Our results indicated no significant difference between the two groups in terms of morphine consumption. However, Senthil et al. reported significantly lower morphine use with the PENG method. They attributed this to more effective analgesia and longer duration of pain relief in the PENG group, which reduced the need for excessive morphine compared to the FICB group (8). Differences in inclusion criteria, local analgesia, and block strategies, as well as the lower mean age of participants in Senthil's study, may account for variations between their findings and ours. Additionally, their study included various types of hip fractures and only ASA I and II patients, whereas our study included ASA III patients as well.
Nausea and vomiting post-surgery were also evaluated, with no significant difference between the two groups, which may be attributed to the similar morphine consumption in both groups within 24 hours after the block. Our results align with those of Natrajan et al., with vomiting rates of 15% in the PENG group and 8% in the FICB group, consistent with previous findings (17). Krishnamurty et al. also found no significant difference in complications between the PENG and FICB methods, corroborating our results (14).
The time of the first opioid request in both groups was not significantly different. Previous studies on this topic have produced conflicting results. Consistent with our findings, Senthil et al. reported no significant difference in analgesia duration between the PENG and FICB groups (8). Jadon et al. also found no significant difference in the time of the first painkiller request between the two groups (18). However, several studies have reported that the time to the first opioid request after surgery was significantly longer in the PENG group. It has been suggested that the PENG method provides longer analgesia, thereby delaying the need for additional painkillers and reducing postoperative opioid consumption. Nonetheless, our study did not find evidence to support this hypothesis, as there was no significant difference between the two groups in this regard.
5.1. Conclusions
Based on our findings, both PENG and FICB blocks significantly reduced postoperative pain in patients who underwent intertrochanteric fracture surgery. Both methods are well-tolerated and do not cause significant complications. However, there was no evidence to suggest that PENG is superior to FICB in terms of pain reduction, opioid consumption after surgery, surgery duration, or prevention of complications. The results of this study are specific to intertrochanteric fractures of the hip joint and may not be generalizable to other types of fractures. Additionally, dynamic pain scores and mobility were not assessed in this study. Further multicenter studies with larger sample sizes are recommended to compare the effects of these two techniques.