1. Context
As conditions evolve worldwide, there is a worrying increase in the number of people suffering from coronary artery disease (CAD) (1). This trend is exemplified in Iran, where chronic illnesses contribute to over 70% of mortality, with cardiovascular diseases, including CAD, accounting for 42% of these fatalities (2). Coronary artery bypass surgery stands as a well-established therapeutic modality for managing CAD patients (3). However, despite its efficacy, this surgical intervention is not devoid of risks and complications (4). One notable complication associated with coronary artery bypass surgery is postoperative delirium (POD), a cognitive impairment that ensues in the aftermath of surgery, particularly prevalent in cardiac procedures due to factors such as hypothermia and the use of cardiopulmonary bypass pumps (5). The incidence of delirium post-cardiac surgery exceeds 90%, significantly impacting patient outcomes. Unlike POD observed in other surgical contexts, cardiac surgery-related delirium presents distinctive features owing to the advanced age of the patient population and specific considerations related to the use of cardiopulmonary bypass pumps necessitating specialized anesthesia techniques (6).
Delirium manifests as a spectrum of cognitive symptoms encompassing alterations in consciousness, reduced attention span, and impaired cognition, with varying durations extending from hours to days post-surgery, leading to heightened morbidity, mortality, and prolonged care requirements. The mortality rate associated with delirium post-surgery ranges from 12% to 33%, substantially elevating the risk of death threefold (7). Perioperative pharmacotherapy plays a pivotal role in mitigating the incidence of POD, with ketamine emerging as a promising agent due to its N-methyl-D-aspartic acid (NMDA) antagonistic properties (6, 8).
Ketamine, recognized for its analgesic and sympathomimetic effects, alongside its anti-inflammatory attributes, exhibits the potential to reduce the inflammatory cascade associated with open-heart surgeries, thereby enhancing recovery and patient satisfaction (9). Preclinical and clinical investigations have underscored ketamine's efficacy in mitigating POD through its anti-inflammatory mechanisms (10). Recent research suggests that adjunctive use of ketamine during general anesthesia for cardiac surgeries may lower the incidence of POD by approximately 3% (11). However, conflicting findings exist, as evidenced by a large-scale trial where single-dose ketamine administration during induction failed to demonstrate significant differences in outcomes across both cardiac and non-cardiac surgical settings (12). Consequently, the precise impact of ketamine on reducing POD remains inconclusive.
Recognizing the evolving landscape of research on this subject, a scoping review methodology is proposed to comprehensively explore existing literature and delineate avenues for future investigations. Given the limited available data, employing a scoping review enables a broad examination of the topic, facilitating the identification of pertinent research questions and guiding subsequent inquiries toward providing nuanced and definitive insights into the challenges surrounding POD management in cardiac surgery contexts. This review framework serves as a blueprint to refine future research endeavors, ensuring a targeted approach toward addressing critical gaps and advancing knowledge in this domain.
2. Evidence Acquisition
2.1. Study Design
The scoping review presented herein was conducted during the latter part of 2023. Within contemporary academic discourse, the scoping review methodology represents a burgeoning paradigm in evidence synthesis, distinguished by its capacity to elucidate expansive research landscapes. Notably, the delineation between systematic reviews and scoping reviews remains a subject of ongoing scholarly deliberation, compounded by a paucity of established guidelines, particularly in scenarios characterized by inadequate literature support. Within the confines of the present inquiry, the absence of well-defined parameters or the presence of intricately nuanced circumstances renders the execution of a more granular systematic review unfeasible. This is primarily attributable to the complexity and uniqueness inherent in the subject matter under investigation. As such, the scoping review emerges as an apt methodology, offering a flexible and comprehensive framework to navigate the uncharted contours of the research landscape. Through its iterative and exploratory approach, the scoping review enables the identification and synthesis of diverse sources of evidence, thereby affording a holistic understanding of the research domain (13). It is pertinent to acknowledge that the nascent nature of this methodological approach necessitates a cautious and judicious application. In the absence of well-established criteria or precedence, scholarly endeavors such as the present scoping review serve not only to contribute to the expanding body of knowledge but also to shape the discourse surrounding evidence synthesis methodologies. Therefore, this study represents a pivotal contribution to the evolving methodology of evidence synthesis, paving the way for future advancements in research methodology and scholarly inquiry. In this scoping review, our intention is to scrutinize the most recent and current literature published in this domain. To achieve this objective, we conducted a search for articles specifically published within the past decade, encompassing the last 10 years.
2.2. Research Questions
For the scoping review entitled "Effect of ketamine administration on the incidence of delirium after coronary artery bypass surgery," the research questions are as follows:
1. Does ketamine administration have a significant effect on the frequency and severity of delirium after coronary artery bypass surgery?
2. Are the side effects associated with the administration of ketamine acceptable after coronary artery bypass surgery?
2.3. Search Strategy
In alignment with the formulated research inquiries, the investigators initiated the search process by employing Medical Subject Heading (MeSH) terminology to derive pertinent keywords. This approach facilitated a systematic exploration of the extant literature across multiple databases, including Scopus, Web of Science, PubMed, Cochrane, and Google Scholar. The search strategy encompassed keywords such as "Delirium," "Agitation," "Ketamine," "Coronary Artery Bypass Graft Surgery," "Open Heart Surgery," and "Cardiac Surgery." In addition to the aforementioned databases, internal repositories such as SID, Iran ISC, and Explore were scrutinized utilizing keywords specifically tailored to the research context, namely "delirium," "coronary artery bypass surgery," and "ketamine." Following the initial search phase, all retrieved publications underwent meticulous scrutiny based on their title and abstract, enabling the exclusion of irrelevant entries. Adherence to methodological rigor was ensured through consensus-building among the research team, comprising four investigators, to resolve any discrepancies in the inclusion criteria. Through a process of negotiation and scholarly discourse, unanimous agreement was attained regarding the selection of articles deemed suitable for inclusion in the study. Subsequently, data extraction was systematically conducted from all identified studies, encompassing key elements such as authorship, research objectives, participant demographics, interventions employed, outcomes assessed, and major findings elucidated. Notably, the scope of the search was delimited to encompass studies conducted within the temporal framework spanning from 2014 to 2024, thereby ensuring relevance and contemporaneity of the retrieved literature corpus. By adhering to rigorous search methodologies and employing stringent inclusion criteria, the research team endeavored to curate a robust evidence base conducive to addressing the delineated research inquiries effectively.
2.4. Study Selection
The process of study selection was meticulously guided by predefined inclusion and exclusion criteria aimed at ensuring the systematic identification and curation of relevant literature pertinent to the research inquiry. Included within the ambit of this study were:
1. Studies directly relevant to the formulated research question.
2. Randomized clinical trial studies and cohort studies.
3. Studies published in either Persian or English language within the past decade, spanning from 2014 to 2024.
4. Studies focusing on the realms of coronary artery bypass graft (CABG) surgery and open heart surgery, wherein ketamine was incorporated as a component of the anesthetic regimen.
5. Investigations encompassing the administration of ketamine in any form and at varying dosages.
6. Studies comparing the efficacy of ketamine against placebo or alternative anesthetic or anti-delirium agents in mitigating the incidence of delirium.
7. Studies specifically examining delirium occurrences within the aforementioned patient cohorts.
Conversely, excluded from consideration were studies pertaining to non-cardiac surgical interventions, pediatric cardiac surgeries, systematic review studies, abstracts, reports, articles with inaccessible full texts, animal studies, conference proceedings, book chapters, and correspondence articles.
Systematic organization and management of the identified literature corpus were facilitated through Endnote© version 9 software, wherein duplicate entries were meticulously eliminated to streamline the dataset. Subsequently, a three-tiered evaluation process was implemented to ascertain adherence to entry and exit criteria, with any discordance being adjudicated by a fourth member of the research team, ensuring unanimity in the final selection of articles for inclusion in the study. By adhering to stringent selection criteria and employing a robust evaluative framework, the study aimed to engender a comprehensive and methodologically sound evidence base poised to yield meaningful insights into the central research inquiries.
2.5. Extracting the Data
The process of data extraction was undertaken by a cohort of four researchers. Extracted data from each pertinent article encompassed a comprehensive array of parameters, including study particulars such as lead authorship and year of publication. Additionally, facets concerning study characteristics, including its primary aim, geographical context, and the respective patient cohort sizes within experimental groups, were meticulously documented. Moreover, patient-centric attributes, exemplified by mean age, were meticulously recorded. Pertaining to intervention, key elements such as the timing of ketamine administration, dosage regimens, and the modality of delivery were systematically collated. Assessment tools adopted within the study framework were identified alongside comparative analyses vis-à-vis placebo or alternative pharmacotherapeutic agents.
Subsequently, the amassed data underwent rigorous analysis and was meticulously prepared for subsequent presentation. Concurrently, an in-depth examination of lacunae within the studies was undertaken, facilitating critical insights into potential avenues for future investigative endeavors. Recommendations pertaining to the amelioration of these identified gaps were thoughtfully deliberated upon, thereby furnishing a comprehensive framework for future research initiatives.
3. Results
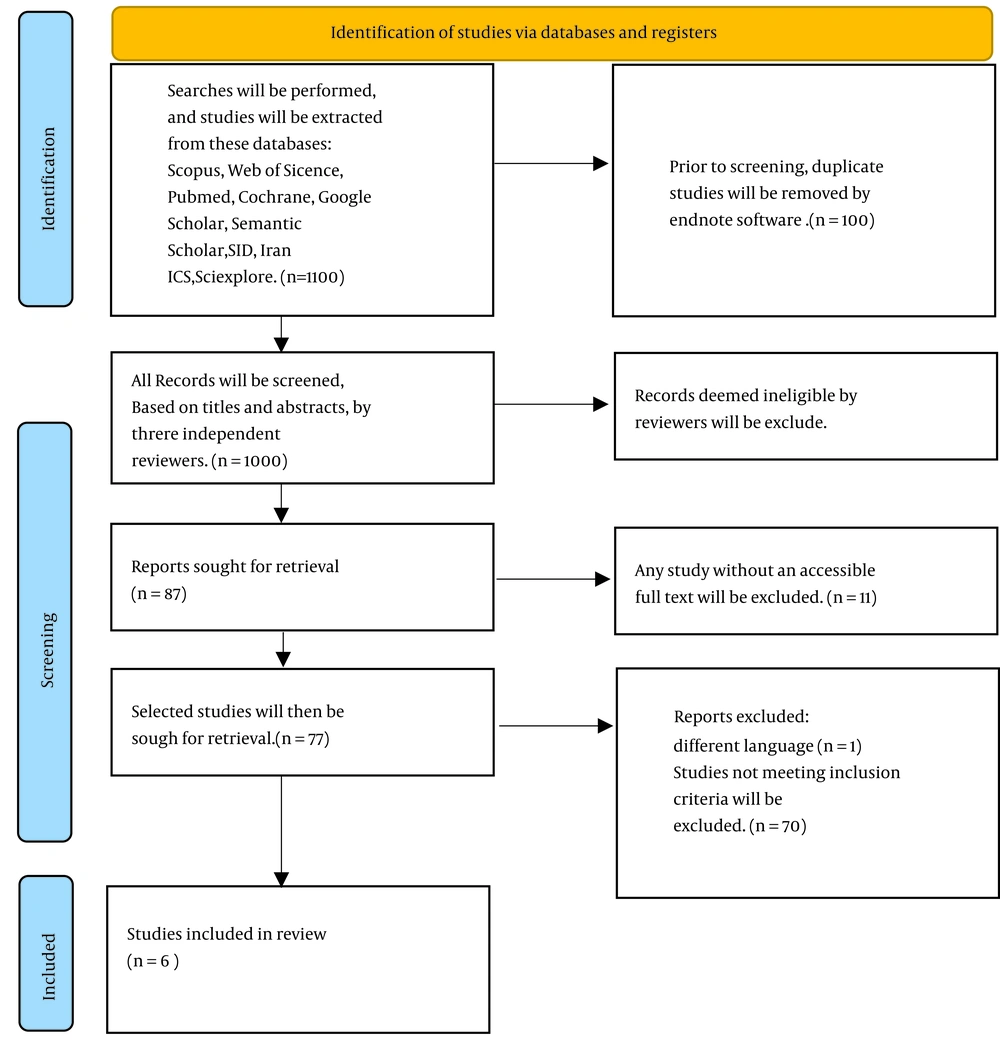
The selection process is summarized in the PRISMA flow diagram (Figure 1). The search strategy yielded an initial pool of 1100 articles. Subsequently, 100 articles were excluded from the review due to duplicate content. Thereafter, the titles and abstracts of the remaining 1000 articles underwent meticulous scrutiny. From this cohort, 6 articles were deemed unsuitable for inclusion on the grounds of being conference papers, while 42 articles were identified as systematic reviews, and 64 were excluded due to their focus on book chapters or animal studies. Following this initial screening phase, the full texts of 87 studies were subjected to thorough evaluation. Within this subset, 70 studies were deemed irrelevant to the research question, necessitating their exclusion. Additionally, one study was eliminated due to linguistic incongruence, and 11 studies were discarded due to the unavailability of complete textual documentation. Consequently, a total of 6 studies—comprising 5 English-language studies and 1 Persian-language study—were deemed eligible for inclusion in the review. The finalized review encompassed randomized controlled clinical trials conducted across diverse geographic locales, specifically Iran, Turkey, Canada, the United States, and Thailand. These trials were uniformly characterized by their focus on elderly patient cohorts, with an average age exceeding 60 years. The results are given in Table 1.
| Num | 1 | 2 | 3 | 4 | 5 | 6 |
|---|---|---|---|---|---|---|
| Year/Author | 2023- Kömürcü et al. (14) | 2023-Wittwer et al. (15) | 2021-Siripoonyothai and Sindhvananda (12) | 2020- Camern et al. (16) | 2017-Avidan et al. (17) | 2015-Soltanzadeh et al. (18) |
| Country | Turkey | USA | Thailand | Canada | USA | Iran |
| Title | Comparison of the hemodynamic effects of etomidate-midazolam and ketamine-midazolam combinations in anesthesia induction in coronary artery bypass surgery | Impact of ketamine versus propofol for anesthetic induction on Cognitive dysfunction, delirium, and acute kidney injury following cardiac surgery in elderly, high-risk patients | Comparison of postoperative delirium (POD) within 24 hours between ketamine and propofol infusion during cardiopulmonary bypass machine: A randomized controlled trial | Intraoperative ketamine for analgesia post-coronary artery bypass surgery: A randomized, controlled, double-blind clinical trial | Intraoperative ketamine for prevention of POD or pain after major surgery in older adults: An international, multicentre, double-blind, randomized clinical trial | The effect of intravenous ketamine during cardiopulmonary bypass on postoperative agitation |
| Sample size(n), population | N = 40 (n = 20 each group), 30 < age < 80+ CABG | N = 52 (n = 25 in the ketamine group and n = 24 in the propofol group)+ age > 70+ surgery involving more than one heart valve, redo sternotomy procedures, or combined valvular and CABG. | N = 82 (n = 32 in each group) + patients undergoing cardiac surgery with CPB, aged > 65 + CABG and valvular surgery | N = 80 (n = 48 in ketamine and n = 38 in the placebo group)+ Age > 18+ CABG surgery with left internal mammary artery harvesting and cardiopulmonary bypass | N = 672 (n = 222) in the placebo group, n = 227 in the 0.5 mg/kg ketamine group, and n = 223 in the 1.0 mg/kg ketamine group) + Age > 60+ undergoing major cardiac( coronary artery bypass graft (CABG) or valve replacement) and non-cardiac surgery under general anaesthesia | N = 40 (n = 20 each groups) Age > 55 +CABG on Pump |
| Prescribed time and dosage of Ketamine | Induction-1 mg/kg Ketamine intravenously + 0.025 mg/kg midazolam | Induction + 1 - 2 mg/kg ketamine intravenously | During CPB +1 mg/kg/h ketamine | 0.5 mg/kg ketamine intravenously as a bolus dose prior to skin incision, followed by an infusion of 0.5 mg/kg/h until the end of surgery | After induction of anesthesia and before surgical incision+ 0.5 or 1.0 mg/kg ketamine | 0.5 mg/kg ketamine iv before sternotomy and repeated the same dose on the pomp during warming |
| Comparison group | 0.3 mg/kg Etomidate + 0.025 mg/kg midazolam | 0.5 - 1 mg/ kg propofol | During CPB + 1.5 - 6 mg/kg/h propofol | Bolus and saline infusion in the same amount and volume as ketamine | Equivalent volume of normal saline | The same volume of normal saline |
| Research design and instrument | Prospective, randomized, and double-blinded study; CAM-ICU | Prospective randomized study; CAM | Randomized controlled trial; CAM-ICU | Single university academic center, randomized, controlled, double-blind clinical trial; CAM-ICU | Multicentre, international randomized trial; CAM/CAM-ICU | Double-blind clinical trial; SAS |
| Result | No hemodynamic difference between the two groups (P > 0.05). The use of the ketamine-midazolam combination is suitable in CABG patients without causing cardiovascular instability. No difference in the incidence of POD during one week after surgery (P-value was not reported). | A significant decrease was observed from preoperative to postoperative testing for many cognitive tests for both groups. The incidence of AKI is higher in the propofol group (P = 0.08). +The need for a lower dose of vasopressors in the ketamine group (P = 0.03). There was no difference in the incidence of POD between the two groups (P = 0.23). Ketamine has no advantage or disadvantage in the induction of anesthesia compared to propofol in the induction of delirium. | The mean intraoperative arterial pressure was higher in the ketamine group (P = 0.01). +Risk of POD was higher in the Propofol group. Demographic information and preoperative variables are non-significant risk factors (P = 0.30). No occurrence of nightmares and hallucinations up to 24 hours after the operation in both groups | There is no hemodynamic difference between the two groups. No notable variance in postoperative opioid use or pain levels within 48 hours post-CABG surgery (P = 0.53). The incidence of delirium was not different in the two groups (P = 0.28). Extubation time was not different between the two groups (P = 0.63). The patient's movement was greater in the ketamine group than in the placebo group (P = 0.03). | Time to delirium onset, duration of delirium, and delirium severity did not differ significantly between the three groups over postoperative days 1–3. There was no difference in the incidence of POD between the groups (P = 0.80). There were no apparent differences in pain between the three groups at any of the postoperative time points. With increasing ketamine dose, more patients reported hallucinations (P = 0.01) and nightmares (P = 0.03). | The reduction of agitation in the ketamine group in the first 24 hours was not statistically significant) P > 0.05). Within 72 hours after the operation, the agitation of the patients in the ketamine group was less than the placebo (P < 0.05). + The hemodynamics of the patients did not differ between the two groups (P < 0.05). |
| Adverse effects | Adrenal suppression on the day after surgery in the etomidate-midazolam group | Not reported | Not reported | Not reported | Adverse events (cardiovascular, renal, infectious, and gastrointestinal bleeding) did not differ significantly across the three groups (P < 0.4). | Not reported |
| Conclusion | There was no difference in the incidence of delirium between the two groups. | The study found no POCD difference in elderly patients receiving ketamine for complex cardiac surgery. Protective effect of ketamine induction against AKI compared with propofol | The effect of ketamine on the occurrence of delirium in the first 24 hours after surgery is unclear (P = 0.04). | The incidence of delirium was not different in the two groups | The administration of a sub-anesthetic dose of ketamine in patients aged 60 years or older undergoing major surgery did not reduce the incidence of POD, affect postoperative pain, or decrease postoperative opioid administration. | Ketamine reduces agitation up to 72 hours after surgery. |
Summary of Studies Using Ketamine to Prevent Delirium in Coronary Artery Bypass Surgery
4. Discussion
Delirium following CABG surgery is a significant clinical concern due to its potential impact on patient outcomes. Accordingly, the present review was conducted with the aim of investigating the effect of ketamine administration on the occurrence of delirium after CABG surgery. The insights gleaned from this inquiry illuminate the prospective role of ketamine in mitigating POD and its attendant implications for clinical practice.
The current scoping review endeavors to identify recent clinical trials elucidating the effects of ketamine administration on delirium occurrence post-CABG surgery, culminating in a corpus of six pertinent studies. According to the findings presented in Table 1, it is evident that several investigations have been conducted concerning the incidence and effects of delirium, postoperative agitation, and related complications in patients undergoing various medical procedures. Notably, among the studies reviewed, three did not yield statistically significant disparities in delirium incidence when comparing different treatment groups. Conversely, one study elucidated a noteworthy observation whereby the risk of delirium was notably elevated in subjects administered propofol in contrast to those receiving ketamine (12). Additionally, a singular investigation demonstrated the efficacy of ketamine in mitigating postoperative agitation, specifically in individuals undergoing open-heart surgery (18).
Moreover, a study addressed the occurrence of nightmares in the postoperative period in relation to ketamine administration, with its findings indicating a lack of discernible variance in the manifestation of such complications (12).
Furthermore, an examination revealed that the utilization of ketamine prompted earlier postoperative mobilization among patients, thereby potentially ameliorating complications associated with prolonged hospitalization (16). These findings collectively underscore the multifaceted nature of ketamine's effects within the postoperative context and its potential implications for patient care and management strategies.
According to the findings of this investigation, POD emerges as a prevalent complication, particularly among elderly individuals undergoing cardiac interventions, with an estimated incidence potentially reaching 60% (19). The consequences of POD span a spectrum from mild impairment to severe physical complications, encompassing catheter misplacement, self-extubation incidents, enduring cognitive dysfunction post-surgery, and escalated one-year mortality rates. While the etiology of POD is multifaceted, inflammation emerges as a primary contributory factor (12). Diverse strategies have been explored to ameliorate postoperative cognitive dysfunction (POCD), encompassing pharmacological interventions such as lidocaine and steroids alongside measures aimed at sustaining optimal mean arterial pressure and augmenting cerebral oxygenation via cerebral oximetry, blood transfusions, and manipulations in blood flow dynamics during cardiopulmonary bypass (CBP). However, the efficacy of these interventions exhibits variability, with pharmaceutical modalities generally evincing limited effectiveness (15). Notably, anesthetic agents harbor anti-inflammatory properties capable of modulating the inflammatory cascade, thus potentially curbing the incidence of POD (12).
Ketamine, characterized by its analeptic properties, exerts stimulatory effects on the sympathetic nervous system and confers anti-inflammatory attributes, particularly noteworthy in the context of open-heart surgeries (9). Notwithstanding, the precise efficacy of ketamine in mitigating POD remains contentious, as underscored by divergent study outcomes.
A study by Wittwer et al. in 2023 failed to delineate a discernible effect of ketamine compared to propofol on cognitive dysfunction or POD induction (15). Similarly, the investigation by Siripoonyothai and Sindhvananda in 2020 indicated the generally ineffectual nature of ketamine in preventing 24-hour POD, albeit with a potential reduction in delirium events within the initial 24 hours compared to propofol (12). Additionally, synergistic combinations such as ketamine and midazolam have been explored, demonstrating favorable hemodynamic stability, albeit without conclusive evidence of decreased delirium incidence (14). Contrastingly, a 2017 study contradicted the notion of ketamine's efficacy in reducing POD, suggesting potential adverse experiences (17). Nonetheless, Sultanzadeh et al.'s work suggested a role for ketamine infusion in mitigating postoperative agitation (18). Our findings resonate with prior research, including Hadetz et al.'s 2010 study, which suggested a modest reduction in POD with ketamine adjunctive to general anesthetics (11).
Furthermore, our investigations align with the systematic review conducted by Howagyomin et al. in 2018, affirming the potential neuroprotective effects of intraoperative ketamine administration in high-risk populations, albeit without categorical dismissal of POD risk (20). In summation, our scoping review underscores ketamine's potential as an anesthetic possessing anti-inflammatory and analgesic properties, with conceivable implications for POD mitigation post-CABG surgery. However, disparate study outcomes underscore the necessity for nuanced consideration of various factors impacting ketamine's efficacy. The heterogeneity in study designs, patient cohorts, drug dosages, and outcome metrics engenders challenges in result interpretation, necessitating comprehensive future research endeavors. It is imperative that forthcoming investigations not only probe ketamine's efficacy but also meticulously scrutinize its safety profile, with particular attention to potential adverse effects such as tachycardia and unfavorable patient experiences. Additionally, factors such as patient age, pre-existing cognitive status, and cardiovascular health severity warrant meticulous consideration in future analyses. Thus, the imperative for further detailed investigations persists to fully elucidate ketamine's multifaceted effects on POD and associated physiological and cognitive parameters following cardiac surgery.
5. Limitations
In this scoping review, there is a potential risk of overlooking pertinent scientific studies in the literature selection process. Additionally, the imposition of specific historical and linguistic criteria could introduce bias into research assessments, potentially resulting in the exclusion of relevant subjects. Additional factors to consider include the overall research quality, variations among studies, and sample size adequacy.
6. Conclusions
The contemporary scoping review conducted herein has delineated the latest clinical trials investigating the impact of ketamine administration on delirium incidence subsequent to CABG surgery. This comprehensive synthesis encapsulates six pivotal studies yielding noteworthy findings. The analysis offers a nuanced and somewhat equivocal perspective regarding the influence of ketamine administration on POD following CABG surgery. Despite a decade-long investigative endeavor, the definitive ramifications of ketamine on POD remain elusive. On the one hand, certain investigations posit that ketamine, endowed with its distinctive anti-inflammatory and analgesic attributes, holds promise in potentially mitigating POD incidence, thereby furnishing a promising avenue for augmenting postoperative convalescence and cognitive outcomes. Conversely, there exists substantive evidence suggesting that ketamine administration may engender adverse experiences, prompting apprehensions regarding its safety and overall perioperative benefits.
The divergent findings underscore the multifaceted nature of POD, influenced by a myriad of factors, including surgical stress, patient-specific susceptibilities, and the intricate interplay of pharmacotherapeutic agents employed during and post-surgery. The heterogeneity observed in study designs, patient cohorts, dosing protocols, and assessment methodologies further obfuscates definitive conclusions. In light of the extant evidential landscape, it is evident that a more rigorous and meticulously designed research paradigm is imperative to comprehensively elucidate the role of ketamine in POD prevention or mitigation subsequent to cardiac surgery.
Subsequent investigations should strive to elucidate optimal dosing paradigms, administration timings, and patient stratification criteria to optimize the potential benefits of ketamine whilst mitigating attendant risks. Pending the accrual of such substantiated evidence, clinicians are tasked with judiciously balancing the potential merits of ketamine administration against its plausible adverse effects, cognizant of individual patient characteristics and the broader clinical milieu. Consequently, while ketamine harbors promise as a constituent of multimodal strategies aimed at POD reduction, its incorporation into clinical practice necessitates prudent deliberation, grounded in the latest empirical insights and tailored to the idiosyncratic exigencies of each patient. The imperative for further inquiry in this domain is not merely suggested but deemed indispensable to augment the comprehension and utilization of ketamine within the perioperative milieu of patients undergoing CABG surgery.