1. Background
Arterial blood pressure (BP) monitoring is a cornerstone of hemodynamic monitoring in patients undergoing surgery. Accurate blood pressure measurement is crucial for the early diagnosis and treatment of both hypotension and hypertension. Sudden changes in blood pressure can impair the function of vital organs, including the brain (1), heart (2), and kidneys (3). Previous studies have indicated that improper hemodynamic management during cardiopulmonary bypass (CPB) is a potential and modifiable risk factor for major complications following cardiac surgery (4). Therefore, precise monitoring of arterial blood pressure (ABP) is essential for the optimal management of heart surgery patients.
This requirement can be addressed by inserting an intra-arterial catheter and connecting it to a pressure monitoring system, which is considered the gold standard for measuring ABP in patients susceptible to rapid hemodynamic changes. However, invasive arterial pressure (IAP) monitoring is associated with complications such as thrombosis, vascular occlusion leading to limb ischemia, hemorrhage, infection, and challenges during catheter insertion (5).
Recently, continuous non-invasive beat-to-beat arterial blood pressure monitors have been introduced, demonstrating favorable comparisons with invasive methods in terms of accuracy and precision. One such example is the CNAP™ monitoring system, which uses inflatable finger cuffs to continuously capture ABP waveforms, calibrated by oscillometric brachial artery cuff measurements. The CNAP™ technique relies on the volume-clamping method while adjusting for changes in vasomotor tone. Approved by the FDA in 2008, the CNAP™ system has been validated for use in specific surgical settings and intensive care units. Non-invasive ABP monitoring systems allow for continuous data collection in a broader range of settings with minimal side effects.
Several studies have compared continuous non-invasive and invasive arterial pressure monitoring during general anesthesia induction in cardiac surgery and subsequently in intensive care units (ICUs). These studies suggest that CNAP can serve as an alternative to IAP in open-heart surgeries, reducing the risks associated with invasive monitoring (6-8). Thus, the CNAP method appears effective for pressure monitoring during cardiac surgery, but its acceptance necessitates comprehensive evaluation across all phases of cardiac surgery.
2. Objectives
Given the significant blood pressure fluctuations during weaning from CPB and the need for precise blood pressure monitoring during this critical phase, the present study was designed to compare systolic, diastolic, and mean arterial pressure (MAP) values between CNAP and IAP during and after weaning from CPB in open-heart surgeries.
3. Methods
This comparative case study was conducted to evaluate two methods of blood pressure measurement during open-heart surgery in patients referred to Dr. Masih Deneshvari Hospital in Tehran. After signing written informed consent during the pre-operative visit, information from 30 patients who met the inclusion criteria (aged 18 - 75 years, undergoing open-heart surgery using the on-pump method) and exclusion criteria (history of peripheral non-elective surgery, BMI > 35, EF < 35%, blood pressure difference between arms > 20 mmHg) was reviewed by the physician. The demographic data of the patients, including age, gender, BMI, and medication history, were recorded in a pre-designed questionnaire.
Upon arrival in the operating room, all study patients were monitored and anesthetized with midazolam, sufentanil, and rocuronium. Anesthesia was maintained using infusions of sufentanil, dexmedetomidine, cis-atracurium, and sevoflurane as needed. An intra-arterial cannula was inserted before the induction of anesthesia for invasive blood pressure (BP) monitoring. A central venous catheter was then placed in the right internal jugular vein for central venous pressure monitoring.
The same surgical team performed all procedures using CPB according to standard protocols. Before separation from CPB, CNAP finger cuffs and a brachial cuff were connected to the opposite hand of each patient for non-invasive BP measurement. BP measurements were taken using both invasive and non-invasive methods simultaneously for 30 minutes at two-minute intervals after CPB weaning.
For the invasive method, BP was measured using a 20-gauge arterial catheter inserted into the radial artery of the non-dominant hand. In the non-invasive method, BP measurements were obtained from the dominant hand using a finger cuff and the volume-clamp method. During the study, all patients lay in the supine position, and their arms were kept at heart level.
The collected data were analyzed using SPSS version 24 statistical software. Descriptive statistics such as mean, standard deviation, and frequency indicators were used to summarize demographic results. For analytical comparisons, paired t-tests or their non-parametric equivalents were employed depending on the results of the Kolmogorov-Smirnov test for normality. All statistical analyses were conducted at a significance level of 5%.
4. Results
The demographic characteristics of the 30 patients undergoing CABG surgery in the present study showed that the average age was approximately 60 years. Among the participants, 76.66% were men, and 23.33% were women. During surgery, the average pump time and clamp time were 121.33 ± 33.59 minutes and 77.7 ± 28.17 minutes, respectively. Additionally, 53.33% of the patients required inotropes or vasopressors during weaning from CPB (Table 1).
| Indexes | Values |
|---|---|
| Age | 59.96 ± 13.82 |
| Gender (P-value = 0.002) | |
| Male | 23 (76.66) |
| Female | 7 (23.33) |
| BMI (kg/m2) | 20.64 ± 3.06 |
| BSA (m2) | 1.77 ± 0.1 |
| Underlying diseases | |
| Hypothyroidism | 1 (3.33) |
| HTN | 16 (53.33) |
| Kidney disorder | 1 (3.33) |
| Diabetes | 11(36.66) |
| Hyperlipidemia | 11 (36.66) |
| MI | 2 (6.66) |
| Smoking | 11 (36.66) |
| Addiction to opium | 5 (16.66) |
| EF (%) | 43.89 ± 8.69 |
| Pump time (minutes) | 121.33 ± 33.59 |
| Clamp time (minutes) | 77.7 ± 28.17 |
| Prevalence of receiving inotropes after CPB | 16 (53.33) |
| Inotrope type | |
| Epinephrine | 6 (20.00) |
| Norepinephrine | 7 (23.33) |
| Dopamine | 1 (3.7) |
| Dobutamine | 1 (3.7) |
| Milrinone | 1 (3.7) |
Demographic Characteristics and Surgery Information of Patients Undergoing Coronary Artery Bypass Grafting Surgery a
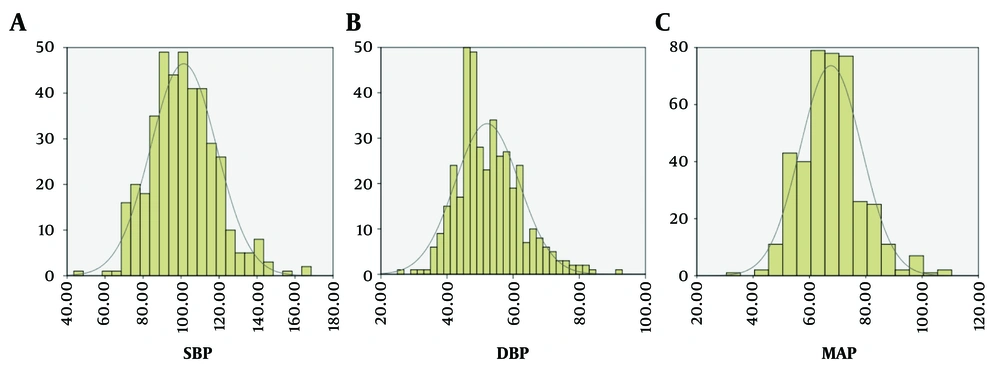
The examination of the median and mode of MAP, SBP and DBP indicators is shown in Table 2 and Figure 1.
| Indexes | Median | Mode |
|---|---|---|
| SBP (mmHg) | 100 | 95 |
| DBP (mmHg) | 50 | 47 |
| MAP | 67 | 65 |
The Examination of the Median and Mode of Indicators
The results for MAP, analyzed using paired samples tests, revealed no statistically significant difference at the 0.05 level between the IAP and CNAP methods in patients undergoing heart surgery (P > 0.05). Thus, the two methods provided comparable MAP values.
In contrast, a comparison of SBP mean values demonstrated a significant difference between the two methods starting 10 minutes after separation from CPB (P < 0.05). The values measured by IAP were higher than those obtained by CNAP at most time points.
Regarding DBP, significant differences were observed between the IAP and CNAP methods at 2, 8, 10, 18, 20, and 22 minutes after separation from CPB (P < 0.05). In these instances, the values measured by CNAP were higher than those measured by IAP.
The systolic CNAP-IAP differences in patients were negative, while the diastolic CNAP-IAP differences in patients undergoing CABG surgery after separation from CPB were positive. The average SBP difference was -7.79 mmHg, indicating that CNAP measurements for systolic blood pressure (SBP) were generally lower than those obtained via IAP. Conversely, the average DBP difference was 4.78 mmHg, showing that CNAP measurements for diastolic blood pressure were higher compared to IAP. Additionally, the mean MAP difference was minimal at 0.49 mmHg, indicating close agreement between the two methods for MAP measurements (Table 3).
| Indexes | SBP (mmHg) | DBP (mmHg) | MAP |
|---|---|---|---|
| CNAP-IAP | -7.79 ± 11.45 | 4.78 ± 12.50 | 0.49 ± 7.7 |
Systolic Blood Pressure Difference and Diastolic Blood Pressure Difference and Mean Arterial Pressur with CONTINUOUS NON-INVASIVE ARTERIAL PRESSURE and Invasive Arterial Pressure Methods in Patients Undergoing Coronary Artery Bypass Grafting Surgery After Separation from Cardiopulmonary Bypass a
5. Discussion
Intra-arterial measurement of blood pressure is the standard method in cardiac surgery patients, providing continuous and reliable monitoring, especially during hemodynamic fluctuations. However, recent findings suggest that CNAP may be a reliable device for continuous assessment of arterial blood pressure, leading to its investigation in a wide range of clinical applications (9, 10). Our study demonstrated no significant difference in MAP measurements between the CNAP and IAP methods during and after weaning from CPB in CABG patients (P > 0.05). SBP measured by IAP was consistently higher than CNAP across all recorded times, with the difference becoming statistically significant 10 minutes after weaning from CPB (P < 0.05). Conversely, DBP measured by CNAP was significantly higher than IAP at various time points during this period (P < 0.05). These findings suggest that MAP measurement by CNAP may be a suitable alternative to the invasive method following separation from CPB in cardiac surgery patients.
In a similar study, Kumar et al. (6) compared CNAP and IAP in hospitalized ICU patients after cardiac surgery. They monitored 30 patients, measuring SBP, DBP, and MAP every minute for two hours after ICU admission. Consistent with our findings, SBP measured by CNAP was lower, while DBP was higher than IAP. The observed bias for SBP was 10.41 mmHg, for DBP was 5.33 mmHg, and for MAP was only 0.039 mmHg (8).
Another study by Kumar et al. investigated differences between CNAP and IAP during anesthesia induction in 60 cardiac surgery patients (6). Similar to our results, SBP measured by CNAP was lower, and DBP was higher than IAP. They reported biases of 5.98 mmHg for SBP, 3.72 mmHg for DBP, and 0.02 mmHg for MAP. The authors concluded that the acceptable bias between CNAP and IAP supports CNAP as a reliable method for patient monitoring during anesthesia induction (11).
The CNAP measurements represent ABP in the brachial artery because of calibration with upper-arm oscillometric measurements. Although comparing CNAP and IAP in the brachial artery would have been closer to an ideal study design, we chose not to perform arterial cannulation at this site, as it is not a standard location for measuring blood pressure during cardiac surgeries and may carry a higher risk of complications compared to radial artery cannulation (12).
Based on cardiovascular physiology, due to wave reflection and resistance to flow, systolic pressure in the radial artery is higher, and diastolic pressure is lower than these pressures in the brachial artery. Therefore, the bias observed between the two methods in the present and similar studies may be attributed to physiological differences in arterial pressures at the brachial and radial sites. Another factor contributing to the difference in systolic and diastolic pressure measurements between the two methods could be that CNAP is calibrated at predetermined intervals, while invasive arterial monitoring provides real-time measurements. The time elapsed since the previous CNAP calibration may account for the observed bias between the two methods.
Although it would have been ideal to measure IAP in the brachial artery, this was not performed in our study due to ethical considerations.
The American Association for the Advancement of Medical Instrumentation states that differences in SBP measured by the oscillometric sphygmomanometry method in the brachial and radial arteries range from 0.68 to 13.4 mmHg, and differences for diastolic blood pressure (DBP) range from 0.8 to 18 mmHg (13). Meanwhile, another study, which compared pressures measured in the brachial and radial arteries, reported that 46%, 19%, and 13% of participants had radial SBP > 5, between 5 and 10, and between 10 and 15 mmHg higher than brachial SBP, respectively. Additionally, 14% of participants exhibited radial SBP > 15 mmHg higher than brachial SBP, representing the so-called "Popeye phenomenon" (14).
In our study, the average value of radial SBP was 7.79 mmHg higher than the systolic pressure measured by the CNAP monitor, and the average DBP difference between the two methods was 4.78 mmHg. These findings indicate that both the average systolic and diastolic pressure differences in this study were within the aforementioned ranges.
In terms of MAP monitoring, the results of the present study showed that the difference between mean values recorded by the two methods was 0.49 mmHg, which is within the clinically acceptable range (±5 mmHg) recommended by the ANSI/AAMI Society for the Advancement of Medical Instrumentation SP10. Furthermore, the measured standard deviation (7.7 ± 0.49) aligns with the declared range (SD < 8 mmHg), confirming that MAP measurement by the CNAP monitor is accurate and reliable.
This study had some limitations, including the small sample size, limited variety in surgical procedures, and the lack of inclusion of high-risk patients. These factors should be considered when designing future studies to expand on the findings presented here.
5.1. Conclusions
The results of the present study demonstrated that MAP measurements obtained using the CNAP method serve as a reliable representation of those obtained through intra-arterial invasive methods. Although differences were observed in systolic and diastolic pressures recorded by the two methods, these differences fell within the clinically acceptable range. Therefore, the systolic and diastolic pressures measured by the CNAP method can be confidently utilized for clinical decision-making. In conclusion, this study suggests that CNAP is a suitable alternative to invasive blood pressure monitoring for patients undergoing CABG surgery, particularly after weaning from CPB.