1. Background
Trans-nasal surgery is a minimally invasive neurosurgical approach for the management of various cranial disorders (1-3). Despite its potential to reduce the risk of complications, this approach may still pose some inherent risks, including infection (4), bleeding, and hemodynamic fluctuations. Hemorrhage during the surgery can result in hematoma formation or compromise the surgical field. Therefore, meticulous hemostasis during the surgical procedure is imperative to minimize bleeding-related complications (5-7).
Anesthesiologists face several challenges during transsphenoidal pituitary surgery due to the intricate approach and the physiological demands of the procedure. Airway management is complex, as surgery through the nose restricts access and may require nasal intubation, which can be difficult, especially in patients with enlarged facial structures resulting from pituitary tumors. Hemodynamic stability is crucial, as blood pressure fluctuations could increase intracranial pressure (ICP) or lead to significant blood loss if nearby vessels are compromised. Postoperatively, anesthesiologists work to minimize pain and postoperative nausea to prevent ICP spikes, often opting for a quick wake-up protocol to allow immediate neurological assessment. Managing these factors is vital for patient stability and successful surgical outcomes (8, 9).
Medications such as clonidine, remifentanil, atenolol, dexmedetomidine, and magnesium sulfate have been employed to attenuate the hemodynamic responses that occur during trans-nasal trans-sphenoidal pituitary surgery (10-12).
Dexmedetomidine (a highly selective α2 agonist) produces effects that lead to sedation, analgesia, respiratory stability, and balanced hemodynamics (13). Dexmedetomidine has also been reported to have neuroprotective effects, making it a suitable option for neurosurgeries (14).
Magnesium sulfate acts as a non-competitive antagonist of the N-methyl-D-aspartate (NMDA) receptor. It inhibits the release of norepinephrine by blocking N-type calcium ion channels, resulting in analgesia and hypotension (11, 13).
2. Objectives
This study is designed to thoroughly explore the effects of two pharmacological agents, dexmedetomidine and magnesium sulfate, on the overall quality of anesthesia, complications, and pain during surgical procedures. The primary objective is to assess how these medications may decrease pain, thereby promoting better patient outcomes. Additionally, the study will evaluate their impact on surgeon satisfaction, as this is a crucial factor in the overall success of surgical interventions. By examining various parameters such as the depth of sedation, hemodynamic stability, and recovery times, this research aims to provide comprehensive insights into the benefits and drawbacks of using dexmedetomidine and magnesium sulfate in clinical practice.
3. Methods
A double-blind clinical trial was conducted at Loghman Hakim Hospital over the course of a year. The research adhered to the principles outlined in the Declaration of Helsinki. The ethics committee approved the procedures for this double-blind, prospective, randomized clinical trial. After explaining the study protocol to all participating patients, we obtained their written informed consent.
The study included patients aged between 18 and 65 years. All participants had an American Society of Anesthesiologists (ASA) physical status of I or II and were candidates for elective trans-sphenoidal pituitary surgery under general anesthesia.
Exclusion criteria included patients with morbid obesity [Body Mass Index (BMI) > 35 kg/m²], a history of alcohol or drug abuse, liver or kidney diseases, a preoperative heart rate (HR) below 50 beats per minute, an ejection fraction below 30%, coagulopathy, neuromuscular diseases, a known allergy to study medications, and those taking certain medications.
Before surgery, patients underwent assessments that included a review of their medical history, a physical examination, neurological evaluations, and laboratory tests. These tests checked for hemoglobin levels, liver and kidney function, thyroid function, electrocardiogram (ECG) results, and hormonal assays.
Patients were assigned to three groups: Group D (dexmedetomidine), group M (magnesium sulfate), and group C (control). This allocation was done using blocks, and it was concealed to ensure that the patients were unaware of their group assignments. Medications for groups D and M were administered in a blinded manner according to the study protocol.
Before surgery, all patients received three minutes of 100% oxygen, 0.2 mg/kg midazolam, 3 - 5 micrograms/kg fentanyl, and 1 - 1.5 mg/kg lidocaine as premedication.
In group D, each patient received a bolus of one microgram per kilogram within 10 minutes, followed by a continuous infusion of 0.5 micrograms per kilogram per hour until the end of the surgery. In group M, patients received a bolus of 50 micrograms per kilogram within the same timeframe, followed by an infusion of 15 micrograms per kilogram per hour until the conclusion of the operation. Additionally, the individual responsible for analyzing the results was blinded to the group allocations.
Various parameters were recorded, including demographic information, hemodynamic measures (such as HR and mean arterial pressure), blood loss, the Boezaart Scale, the Numeric Pain Rating Scale (NRS), BMI, dosages of fentanyl and propofol, the type of surgery performed, and extubation time. The surgery was conducted by a single surgeon, and anesthesia was induced by a single anesthesiologist for all patients. After the surgery, patients were transferred to the post-anesthesia care unit (PACU) for monitoring.
The primary outcome was hemodynamic stability during and after the surgery and surgeons’ satisfaction with the surgery. The secondary outcome was pain, measured with the NRS (Table 1).
| Score | Description |
|---|---|
| 0 | No bleeding, virtually bloodless field |
| 1 | Slight bleeding, blood suctioning is not required |
| 2 | Mild bleeding, occasional suctioning without interference of surgical field |
| 3 | Moderate bleeding, suctioning is usually used; bleeding threatens the surgical field but improves after suctioning |
| 4 | Heavy bleeding, suctioning is frequently used; bleeding threatens the surgical field directly after suction is removed |
| 5 | Severe bleeding, bleeding appears faster than suctioning and is uncontrollable |
The Boezaart Scale for Intraoperative Surgical Field Evaluation
The hemodynamic data of the patients were recorded from the time before anesthesia induction until the end of the surgery. The NRS was measured in the recovery room one hour after surgery.
To determine the sample size, I utilized G*Power software, based on the study conducted by Soliman and Fouad (13). The parameters for the analysis included an effect size of 0.54, a significance level (α) of 0.05, and a power (β) of 0.90. Ultimately, we selected a sample size of ninety patients.
Statistical analyses were performed using SPSS software version 22. Descriptive analysis and independent t-tests were employed to compare variables between the study groups. A P-value of less than 0.05 was considered statistically significant.
4. Results
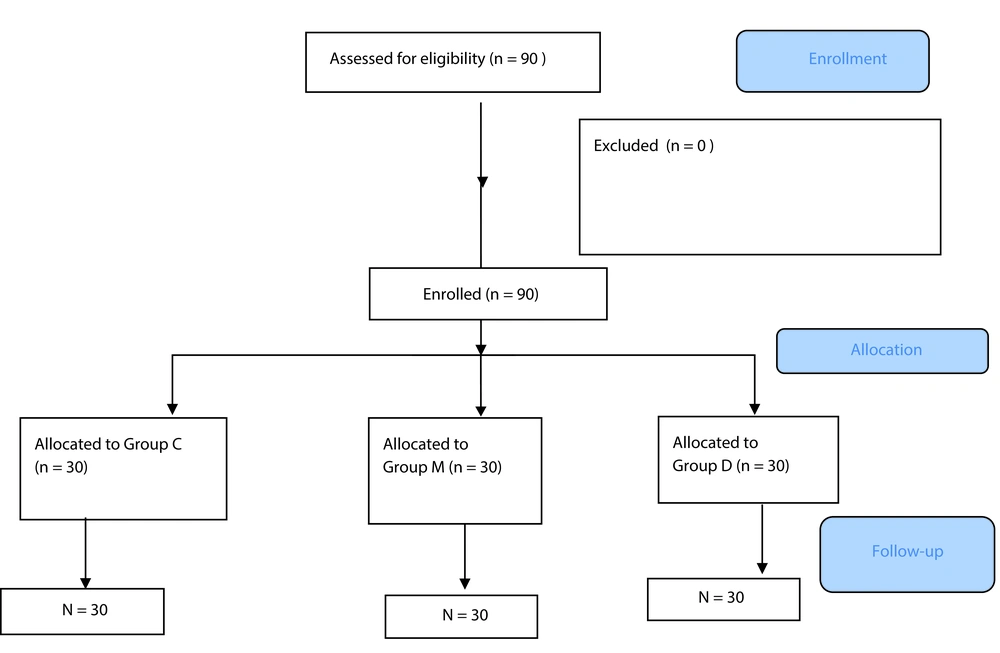
A total of ninety consecutive patients participated in this study, comprising 47 males (52.2%) and 43 females (47.8%). The patients were divided into three groups: 30 controls, 30 patients who received magnesium sulfate, and 30 patients who received dexmedetomidine. All participants were classified as ASA I or II. There were no significant differences among the three groups in terms of gender distribution, age, and BMI, with P-values of 0.582, 0.643, and 0.863, respectively. The mean age of the included patients was 46.27 ± 12.47 years. Figure 1 illustrates the follow-up chart of the participants in the study.
Table 2 presents the mean and standard deviation of the measured variables, categorized by group. Independent t-tests and repeated measures analysis of variance (ANOVA) were conducted to compare each pair of groups. The HR did not show a significant difference between the D and M groups. However, the measured mean arterial pressure (MAP) was significantly lower in the D group (P-value = 0.005). Among the other variables, the only variable that exhibited a statistically significant difference between the two groups was the NRS, which was significantly lower in the D group (P-value = 0.02). Details of the conducted tests are provided in Table 3.
| Variables and Groups | Mean ± SD |
|---|---|
| MAP (mmHg) | |
| D | 58.82 ± 3.60 |
| M | 59.24 ± 1.70 |
| C | 62.99 ± 3.92 |
| Propofol dose (mg) | |
| D | 135.00 ± 28.55 |
| M | 201.67 ± 27.67 |
| C | 250.67 ± 19.46 |
| Fentanyl dose (mcgr) | |
| D | 30.00 ± 38.50 |
| M | 76.67 ± 31.44 |
| C | 160.00 ± 46.23 |
| Extubation time (min) | |
| D | 17.17 ± 2.83 |
| M | 18.63 ± 3.46 |
| C | 18.77 ± 3.18 |
| Amount of bleeding | |
| D | 237.33 ± 201.18 |
| M | 381.33 ± 199.03 |
| C | 450.00 ± 135.97 |
| NRS | |
| D | 3.2 ± 1.03 |
| M | 4.03 ± 0.72 |
| C | 5.40 ± 0.56 |
| Boezaart Scale | |
| D | 2.30 ± 0.65 |
| M | 3.20 ± 0.74 |
| C | 4.03 ± 0.49 |
Demonstrates the Mean and Standard Deviation of Measured Variables According to the Groups
| Variables | Resulted P-Value Comparing D and M Group | Resulted P-Value Comparing D and Control Group | Resulted P-Value Comparing M and Control Group |
|---|---|---|---|
| HR (beats per minutes) | 0.087 | 0.000 | 0.003 |
| MAP (mmHg) | 0.005 | 0.003 | 0.000 |
| Operation time (h) | 0.092 | 0.000 | 0.198 |
| Boezaart Scale | 0.165 | 0.000 | 0.011 |
| Propofol dose (mg) | 0.250 | 0.000 | 0.046 |
| Fentanyl dose (mcgr) | 0.062 | 0.000 | 0.044 |
| Extubation time (min) | 0.088 | 0.056 | 0.579 |
| Bleeding | 0.152 | 0.000 | 0.015 |
| NRS | 0.02 | 0.000 | 0.022 |
Indicates the Result of Conducted t-Test and Repeated Measure Analysis of Variance Between Allocated Groups
All the measured variables in the D group significantly differed from the control group, except for extubation time. The resulting P-values are listed in Table 3.
Table 3 illustrates that all measured variables significantly differed between the control group and the D group, with the exception of extubation time. Additionally, HR, MAP, Boezaart Scale scores, propofol usage, fentanyl administration, bleeding, and the NRS were all significantly lower in the M group.
5. Discussion
The present study demonstrated that patients in the dexmedetomidine group had significantly lower MAP and reduced blood loss compared to those in the magnesium sulfate and control groups. Additionally, surgeon satisfaction was notably higher in the dexmedetomidine group, as indicated by a significantly lower mean Boezaart Scale score (2.30 ± 0.65; P-value: 0.000) when compared to the other two groups. This was further supported by the observation that the use of fentanyl and propofol was significantly lower in the dexmedetomidine group. Interestingly, no significant differences were noted in extubation time among the three groups. These findings suggest that dexmedetomidine is a superior adjuvant for trans-sphenoidal pituitary surgery when compared to magnesium sulfate.
A double-blind, randomized study involving 152 patients undergoing trans-nasal trans-sphenoidal resection of pituitary adenomas found that both magnesium sulfate and dexmedetomidine are safe for these patients. However, dexmedetomidine was more effective in controlling blood pressure and HR than magnesium sulfate, while also providing better visibility at the surgical site and reducing blood loss. Despite these advantages, dexmedetomidine was associated with a higher risk of bradycardia and hypotension compared to magnesium sulfate (13).
In a study by Chhabra et al., both dexmedetomidine and magnesium sulfate were found to be equally effective in inducing controlled hypotension during functional endoscopic sinus surgery (FESS). However, dexmedetomidine achieved the target MAP more quickly and required lower infusion doses. Additionally, dexmedetomidine provided a better surgical field with reduced intraoperative bleeding. The drawback, however, was that sedation and recovery times were longer for patients receiving dexmedetomidine compared to those receiving magnesium sulfate (15).
Srivastava et al. demonstrated that patients undergoing spine surgery who received dexmedetomidine experienced more frequent instances of low blood pressure and slower HRs, with these effects being dose-dependent. In contrast, the magnesium sulfate group had slower recovery times. Both drugs, however, contributed to improved hemodynamic stability with minimal fluctuations and reduced anesthetic usage throughout the intraoperative period when compared to the control group (16).
A comparative analysis by Akkaya et al. focused on the quality of the surgical field during endoscopic sinus surgery, comparing dexmedetomidine and magnesium sulfate. The results showed that dexmedetomidine was more effective at reducing bleeding at the surgical site and provided greater suppression of HR compared to magnesium sulfate. This suggests that dexmedetomidine may be a more effective choice for improving surgical conditions in endoscopic sinus procedures (17).
In a clinical trial by Bala et al., the group receiving dexmedetomidine showed significantly lower intraoperative and postoperative analgesic requirements, as well as reduced needs for anesthetic inhalation and neuromuscular relaxants, compared to the control group (18).
A systematic review of 160 patients across four trials found that the use of dexmedetomidine led to significant changes in HR, arterial pressure, blood loss, and fentanyl consumption (19). These findings align with our results, as patients receiving dexmedetomidine showed improved hemodynamic stability and required less propofol and fentanyl.
A study comparing dexmedetomidine with clonidine for managing hemodynamic responses during trans-nasal trans-sphenoidal resection of pituitary tumors observed that continuous intravenous infusions of dexmedetomidine provided better hemodynamic stability than oral clonidine (10).
In a study by Abdallah et al., 110 patients were divided into two groups to compare the effects of propofol and dexmedetomidine during transnasal transsphenoidal pituitary tumor resection. Patients in the dexmedetomidine group required fewer postoperative analgesics and exhibited lower scores on the Visual Analog Scale (VAS) for pain (20).
In a study involving 80 patients undergoing middle ear surgery, it was found that magnesium sulfate combined with remifentanil could effectively achieve low blood pressure anesthesia. The study also noted significant reductions in postoperative pain at various time points, as well as a decrease in the incidence of postoperative shivering, nausea, and vomiting during the immediate postoperative period (11).
Asgari et al. assessed 100 patients undergoing resection of supratentorial brain tumors and compared those who received dexmedetomidine before anesthesia induction with those who received a saline placebo. The results revealed that patients who received dexmedetomidine had significantly lower systolic blood pressure, HR, and bispectral index score after anesthesia induction, demonstrating improved hemodynamic control (21).
Lastly, Hashemi et al. evaluated 60 patients undergoing percutaneous transforaminal endoscopic discectomy (PTED) and concluded that the procedure is safe and effective, offering excellent analgesia and enabling proper neurological monitoring during surgery (22).
5.1. Limitations
The study we conducted had certain limitations that should be considered. Firstly, it was carried out at a single center and involved a limited number of patients. Therefore, conducting further studies with a larger patient cohort is necessary to comprehensively evaluate a wider range of parameters during and after surgery, as well as potential drug complications.
5.2. Conclusions
In conclusion, our findings suggest that incorporating dexmedetomidine as an adjuvant during trans-sphenoidal pituitary surgery has the potential to improve hemodynamic stability and increase surgeon satisfaction scores to a greater extent than magnesium sulfate.