1. Background
In anesthesia, the term "airway" refers to the upper airways that are of primary concern during mask ventilation and endotracheal intubation. The most reliable method for securing the airway is endotracheal intubation via direct laryngoscopy (1). A difficult airway arises when an adequately trained anesthesiologist encounters challenges with mask ventilation, endotracheal intubation, or both (2), with an incidence ranging from 1.5% to 8% of the population (3).
An unexpected difficult intubation is a serious challenge for anesthesiologists and can lead to fatal outcomes, especially in "cannot intubate–cannot ventilate" (CICV) situations, which account for 25% of anesthesia-related deaths (4). Therefore, predicting difficult airways is crucial in modern anesthesia management. The LEMON method is a rapid and simple technique used to assess a patient's airway in emergency situations. It involves: (1) looking externally for facial trauma, burns, and loose incisors; (2) evaluating the inter-incisor gap, hyoid-mental distance, and thyroid-to-hyoid distance; (3) checking the Mallampati score (≥3); (4) identifying obstructions, such as trauma, epiglottitis, and patients with obstructive sleep apnea (OSA); and (5) assessing neck mobility (5).
Difficult airway algorithms vary significantly among countries, but awake fiber-optic intubation (AFOI) remains the preferred method, especially in patients with limited mouth opening or neck mobility. Achieving adequate airway block (AB) is the first step toward a successful AFOI (6).
While multiple studies (7-10) have compared topical anesthesia techniques with AB methods for AFOI, these studies often do not account for the limited or absent neck mobility and mouth opening that can be present in many difficult airway cases requiring AFOI.
2. Objectives
In this study, we aimed to evaluate the efficacy of lidocaine nebulization (LN) for upper airway anesthesia compared to traditional upper airway nerve block during AFOI in patients with head and neck burns.
3. Methods
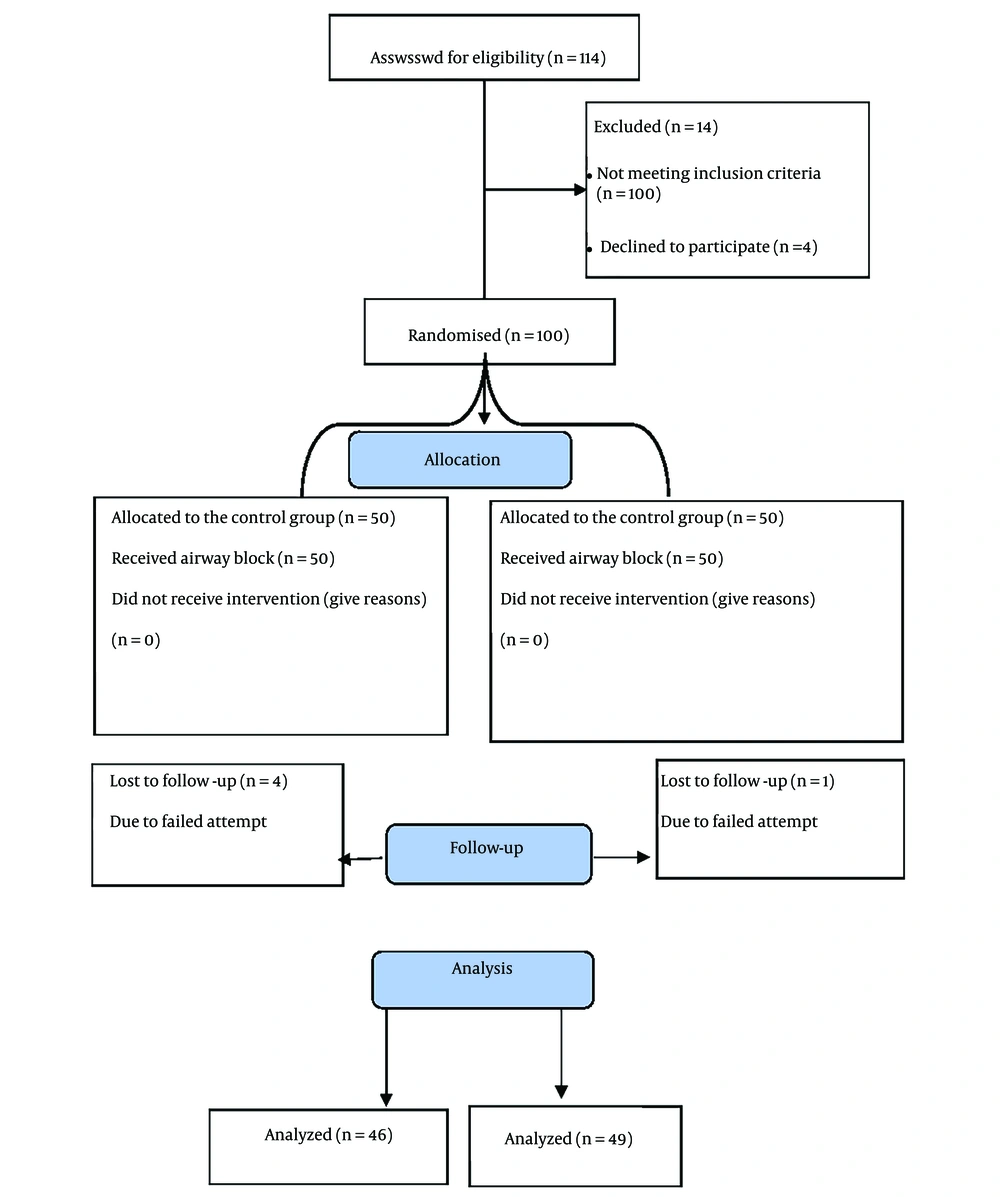
Following Institutional Board Review approval (R121/2022), our trial was registered at clinicaltrials.gov (NCT05550051) on 19/9/2022. Patient enrollment and informed written consent began on 23/9/2022. This randomized, single-blinded prospective study included patients with head and neck burns scheduled for reconstructive surgery between September 2022 and February 2023 at our hospital.
Patients were recruited by anesthesia residents in the anesthesia clinic following admission for surgery. Random allocation was achieved using computer-generated randomization from randomization.com, with number tables placed in sealed envelopes by an anesthesiologist not involved in the study. Eligible participants were adult patients aged 18 - 65 years with head and neck burns, a BMI of 20 - 30 kg/m², and scheduled for reconstructive surgery. Exclusion criteria included patients with coagulopathies, an American Society of Anesthesiologists (ASA) classification of 4, non-cooperative patients, and those with known allergies to lidocaine.
Patients were randomly assigned into two parallel groups of 50 each. In the AB group, AFOI was performed after an AB before the procedure. In the LN group, AFOI was conducted after LN 30 minutes before the procedure. Data collectors and outcome analysts were blinded to the treatment each patient received.
The primary outcome was the time required for successful awake nasal fiber-optic intubation, defined as the duration from inserting the fiber-optic bronchoscope through the patient's nasal opening until a capnography reading was obtained, indicating successful intubation. Secondary outcomes included the revised nonverbal pain scale score during intubation and the number of failed attempts, defined as two failed attempts by an experienced anesthesiologist, followed by the need for tracheostomy under local anesthesia.
3.1. Study Procedures
Preoperative airway assessments were conducted for all patients using the LEMON score. Patients received standard preoperative medications, including 0.3 mg atropine as an anti-sialagogue, bilateral nasal oxymetazoline (Afrin) drops as a nasal decongestant, and 10% lignocaine spray in the nostrils, in accordance with our hospital protocol.
Upon admission to the OR, baseline vital signs were recorded, including blood pressure (BP), heart rate (HR), and O₂ saturation on room air. Patients were randomly assigned to two groups. In the AB group, an upper AB was performed with 2% lidocaine following the technique described by Chavan et al. (11). The block targeted key nerves, and with the patient in a supine position and mild neck extension to palpate the hyoid, a bilateral superior laryngeal nerve block was administered. The injection site was sterilized with povidone-iodine. After identifying the hyoid bone, a sterile 25-G needle was inserted laterally toward the greater cornu. When the needle contacted bone, it was guided inferiorly beneath it, and 2 mL of 2% lidocaine was injected to block the superior laryngeal nerve and its branches. To block the recurrent laryngeal nerve using the transtracheal instillation technique, the patient remained supine with an extended neck. The cricoid cartilage was palpated to locate the cricothyroid membrane. A 22-G needle was inserted perpendicular to the membrane, with aspiration confirming intra-tracheal positioning through the presence of air bubbles. Subsequently, 5 mL of 4% lidocaine was injected, inducing a cough that distributed the local anesthetic and completed the nerve block.
In the LN group, patients received LN with 3 mL of 2% lidocaine, delivered at an O₂ flow rate of 10 L/min to administer 60 mg of lidocaine, approximately 25% of which was absorbed. Patients were instructed to inhale deeply to ensure the anesthetic reached further into the airway for an optimal block (9). Following nebulization, patients were asked about facial and oral tingling or numbness; if these sensations were absent, a second nebulization session was conducted.
During the procedure, vital signs, including BP, HR, and respiratory rate, were continuously monitored. Observations for facial expressions, signs of guarding, and activity were made to complete the patient's Revised Nonverbal Pain Scale (NVPS-R) Questionnaire (12) (Table 1).
| Item | Score (0) | Score (1) | Score (2) |
|---|---|---|---|
| Facial expressions | No particular expression | Occasional grimacing and frowning | Frequent grimacing and frowning |
| Patient’s activity and movement | Lying quietly | Seeking attention through cautious movement | Actively moving |
| Patient’s guarding | Lying quietly | Splinting areas of his body | Lying rigid |
| HR and BP | Unchanged | Increased by > 20/bpm | Increased by > 25/bpm |
| Respiratory rate | Unchanged | Increased by > 10/m | Increased by > 20/m |
Abbreviations: bpm, beat per minute; HR, heart rate; BP, blood pressure.
For each category, the patient was assigned a score of 0 (comfortable), 1, or 2 (distressed). After successful intubation, general anaesthesia was induced with 1 - 2 mg/kg of propofol, 0.25 mg/kg of atracurium, and 2 µg/kg of fentanyl. Fresh gas flow included a mixture of O₂ and air at 2 L/min, and anaesthesia was maintained with 1 - 2 MAC isoflurane and 0.1 mg/kg atracurium every 20 minutes. The patient’s vitals were monitored continuously throughout the operation, with recordings taken every 5 minutes.
Intubation time, the primary outcome, along with vital signs, were recorded by an independent physician who was blinded to the study group. Vital signs were documented immediately and again 5 minutes after intubation. At the end of the surgery, muscle relaxation was reversed with 50 µg/kg of neostigmine combined with 0.02 mg/kg of atropine (13). Signs of lidocaine toxicity, such as seizures, circumoral numbness, central nervous system (CNS) depression, or electrocardiogram changes, were monitored, and the trial would be halted if any signs appeared. Postoperative adverse effects, including hoarseness of voice and aspiration, were also recorded.
3.2. Sample Size
The sample size was calculated using NCSS PASS 11.0. Based on a previous study conducted by Hassanein et al. (10), at least 50 patients per group were necessary to achieve 80% power with a type I error probability of 0.05, allowing for detection of a statistically significant difference between the two groups and rejecting the null hypothesis that failure rates were equal across both groups. The primary endpoint was the time required for successful awake nasal fibre-optic intubation (performed by an expert anesthesiologist with at least 10 years of experience). Secondary endpoints included the number of failed attempts and the NVPS-R score.
3.3. Statistical Analysis
Results were expressed as mean ± standard deviation or as numbers and percentages. Qualitative data were analyzed using the chi-square test, while quantitative data between the two study groups were compared using an unpaired t-test. Comparisons between different measurement times and baseline within the same group were performed using repeated-measures analysis of variance. Data analysis was conducted using SPSS for Windows, version 16.0 (SPSS Inc., Chicago, IL, USA). P-values < 0.05 were considered statistically significant (Figure 1).
4. Results
Statistical analysis showed no significant differences in demographic data between the two groups (Table 2). Additionally, there were no significant differences in hemodynamic parameters between the groups (Table 3).
Abbreviations: ASA, American Society of Anesthesiologists; AB, airway block; LN, lidocaine nebulization.
a Values are expressed as mean ± SD or Number.
b Measured by an independent t-test.
c Measured by the chi-square test.
| Variables | AB Group; (n = 50) | LN Group; (n = 50) | P-Value |
|---|---|---|---|
| HR before intubation (bpm) | 81.40 ± 11.3 | 80.14 ± 11.7 | 0.590 |
| HR immediately after intubation (bpm) | 107.01 ± 16.5 | 109.28 ± 15.9 | 0.490 |
| HR 5 min later (bpm) | 109.81 ± 15.1 | 100.88 ± 14.3 | 0.003 |
| MAP before intubation (mmHg) | 94.64 ± 10.6 | 97.18 ± 10.6 | 0.242 |
| MAP immediately after intubation (mmHg) | 107.49 ± 13.8 | 110.38 ± 13.1 | 0.293 |
| MAP 5 min later (mmHg) | 87.43 ± 14.1 | 91.43 ± 15.1 | 0.182 |
| SpO2 before intubation (%) | 97.19 ± 1.3 | 97.44 ± 1.3 | 0.342 |
| SpO2 was immediately after intubation (%) | 96.31 ± 1.2 | 96.46 ± 1.4 | 0.543 |
| SpO2 5 min later (%) | 99.09 ± 0.9 | 98.92 ± 1.3 | 0.474 |
Abbreviations: bpm, beat per minute MAP, mean arterial pressure; AB, airway block; LN, lidocaine nebulization; HR, heart rate.
a Values are expressed as mean ± SD.
b P values measured by an independent t-test.
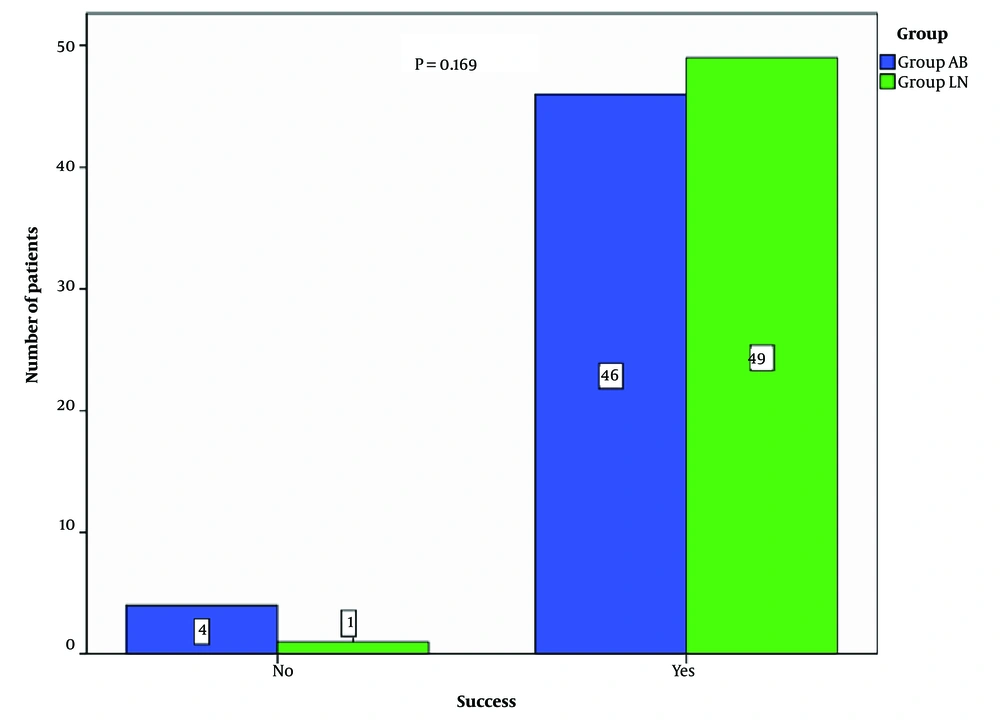
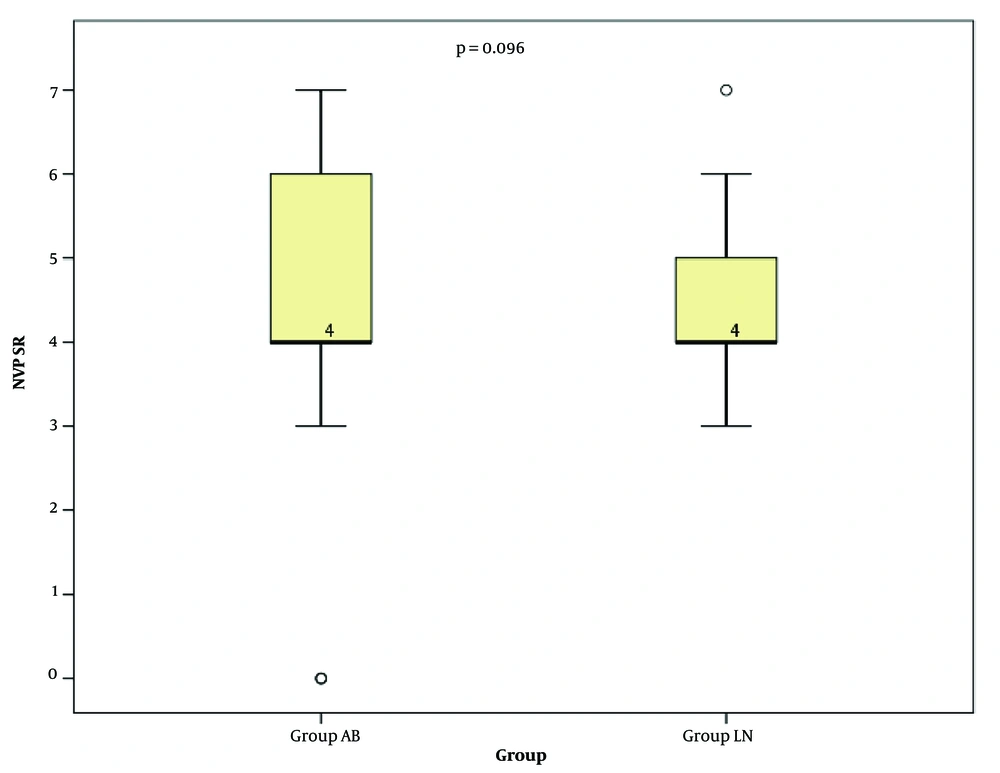
No statistically significant difference was observed between the two groups regarding the time to fibre-optic nasal intubation. Although the number of failed attempts in the AB group was higher than in the LN group, statistical analysis showed no significant difference (Table 4 and Figure 2). The NVPS-R score, which measures patient response and satisfaction, was also not significantly different between the two groups (Figure 3).
Abbreviations: AB, airway block; LN, lidocaine nebulization.
a Values are expressed as mean ± SD, No. (%), or median (range); AB, airway block; LN, lidocaine nebulization.
b Measured by the independent t-test.
c Measured by the chi-square test.
d Measured by independent-samples Mann–Whitney U test.
Regarding side effects, no patients in either group reported any issues such as hoarseness of voice or signs of local anaesthesia toxicity, including cardiac arrhythmia, CNS depression, or seizures. Although the doses and concentrations of lidocaine used in our study were carefully calculated and deemed safe, we monitored for signs or symptoms of toxicity, and none were recorded. Postoperative complications, including aspiration and hoarseness of voice, were also not observed.
5. Discussion
Awake nasal fibre-optic intubation has been practiced for many decades since it was first reported by Murphy in 1967 (14). Numerous techniques have been developed to anaesthetize the upper airway to facilitate awake nasal intubation. In this study, we found that LN alone had a comparable effect to the traditional upper AB commonly used by anaesthesiologists. Lidocaine nebulization is easier to administer, less invasive, and more suitable for patients with head and neck burns, as they often have altered anatomical landmarks that make traditional AB challenging.
An unanticipated difficult intubation remains a significant concern for anaesthesiologists worldwide, leading to the development of various scoring systems and measurements to predict these situations, such as thyromental distance, the Mallampati score, and the LEMON score (15).
Our study included 100 patients divided into two groups, all undergoing reconstructive head and neck surgery following burns. All participants were considered at risk for difficult intubation, ventilation, or both, making them candidates for awake nasal fibre-optic intubation.
The gold standard for facilitating awake nasal fibre-optic intubation has traditionally been upper airway anaesthetization using lignocaine spray combined with local anaesthetic injections to block sensation via the superior laryngeal nerve and through the trachea. While numerous studies have explored methods to facilitate awake nasal fibre-optic intubation, most focus on the use of sedative drugs alongside AB. For example, Chopra et al. and Cattano et al. examined the sedative effects of dexmedetomidine and remifentanil on awake nasal fibre-optic intubation (16, 17). Khandelwal et al. used LN as an adjunct to AB with conventional superior laryngeal nerve block and transtracheal instillation (7).
Chavan et al. compared LN with conventional AB in anaesthetizing patients undergoing surgery for oral malignancies (11). Their study found that the intubation time was shorter in the group receiving superior laryngeal nerve block and transtracheal instillation than in the LN group, differing from our findings, which showed no significant difference between the two groups. In Chavan’s study, the average intubation time was 200 seconds in the AB group compared to 257 seconds in the LN group. These values are notably different from ours, where the intubation times were 26.18 seconds for the AB group and 29.9 seconds for the LN group, likely due to operator experience.
In 2017, Kim et al. reported that the average time for fibre-optic intubation among training residents was 53.8 seconds (18), and some educational videos demonstrate awake nasal fibre-optic intubation performed in under 60 seconds. Based on this, the times reported by Chavan et al. seem relatively long (11). Similarly, Kundra et al. found no significant differences in intubation time between AB and LN groups (19).
Patient satisfaction was also comparable across groups in our study. In Chavan et al.’s study (11), haemodynamic fluctuations were higher in the LN group than in the AB group, a variation we did not observe. This difference might be attributed to the faster intubation times achieved in our study.
Hassanein et al. examined the effects of adding airway nerve blocks to LN for patients undergoing AFOI, concluding that this combination improved anaesthetic quality and patient satisfaction (10).
In our study, there were four failed intubation attempts in the AB group compared to only one in the LN group, though statistical analysis showed no significant difference in success rates, possibly due to the sample size.
Our study may have been subject to some bias since it was not double-blinded. Additionally, unlike similar studies, we did not measure serum lignocaine levels to monitor systemic toxicity during the procedure. Another limitation was combining maxillofacial and neck surgeries, rather than conducting separate studies for each category.
Both upper AB and LN provide effective conditions for awake nasal fibre-optic intubation. However, LN is less invasive, easier to perform, and more suitable for patients with distorted upper airway anatomy, such as those with head and neck burns.