1. Background
In recent years, breast tumors have been identified as the most common tumors in women, particularly following a modified radical mastectomy (MRM). Effective pain management is essential for both patient satisfaction and early ambulation (1). Opioids are commonly used to manage postoperative pain in MRM patients. Gastritis and peptic ulcers are two adverse gastrointestinal effects associated with NSAIDs. Additionally, constipation, nausea, vomiting, and respiratory depression complicate opioid usage (2). Although the thoracic paravertebral block (TPVB) is regarded as the gold standard for regional anesthesia in breast surgery, its procedural complexity and risk of adverse events, such as pneumothorax and hypotension, have resulted in a growing interest in alternative truncal blocks, particularly the costotransverse block (CTB) and the serratus anterior plane block (SAPB) (3).
The CTB is an ultrasound-guided technique in which a local anesthetic is administered into the costotransverse foramen (CTF). Its purpose is to anesthetize the dorsal rami of the thoracic spinal nerves (T2 - T6) as they pass through the intertransverse space (4). The efficacy of this technique depends on the local anesthetic's spreading through the CTF to nerve roots in the paravertebral space (5).
The CTF is an anatomical space bounded superiorly by the transverse process of the vertebra above, inferiorly by the superior border of the rib at the target level, medially by the lateral edge of the vertebral lamina, laterally by the posterior surface of the rib, anteriorly by the pleura, and posteriorly by the superficial back muscles (6). This method achieves widespread somatic and visceral analgesia throughout the ipsilateral thoracic region, including the breast tissue, pectoral musculature, and axillary area (7).
In contrast, the SAPB relies on superficial or deep fascial infiltration adjacent to the 4th rib, primarily affecting the lateral cutaneous branches of the intercostal nerves (T2 - T9) (8). A debilitating complication of breast malignancy surgery, persistent neuropathic pain confined to the breast, chest wall, medial upper arm, and axilla is a hallmark of post-mastectomy pain syndrome (PMPS). It is hypothesized that intercostobrachial nerve damage is the primary cause of PMPS (9).
The underlying pathophysiology is thought to be generated by ectopic neuronal signals that increase sensitivity to mechanical or chemical stimuli and begin at the dorsal ganglion and nerve damage site (10).
2. Objectives
This randomized prospective trial aimed to evaluate the efficacy of CTB relative to SAPB and traditional analgesia in alleviating acute and chronic pain following breast surgeries.
3. Methods
The study was conducted according to the Declaration of Helsinki, following written informed consent from each patient and approval from the Research Ethics Committee at the Faculty of Medicine Ain Shams University (FMASU MD230/2023). This was a randomized, controlled, double-blind study conducted from October 2023 to October 2024. It was registered as a clinical trial (https://www.clinicaltrials.gov) with database ID number (NCT06260397) on 23/10/2023. Using the PASS 15 program for sample size calculation, setting an alpha error of 0.05, and according to Saad et al., 2018, a sample size of 30 patients per group can detect a difference between study groups with power > 90%. Therefore, 107 patients provided written informed consent for a mode of analgesia that may include either a nerve block or patient-controlled analgesia (PCA) following MRM surgeries. All participants, who were female and aged between 18 and 60, had physical statuses of I to II according to the American Society of Anesthesiologists and were scheduled for primary elective unilateral MRM. Their body weight ranged from 60 to 100 kg. The following criteria were among the exclusions: Refusal to provide consent; a history of allergy to one of the study's medications; contraindications to local anesthesia, such as local infection and coagulopathy; severe cognitive impairment; physical status III and IV according to the American Society of Anesthesiologists; daily use of analgesics for chronic pain; and patients with severe pulmonary dysfunction.
Computer-generated randomization was used to allocate numbers from 1 to 107 into three groups (SAPB in group A, CTB in group B, and PCA in group C), with each number placed in an opaque sealed envelope. Patients were asked to pick one envelope from a box containing similar envelopes, and the number they received assigned them to one of the three groups. The patients and the investigators responsible for assessing the primary and secondary outcomes were blinded to the study group assignment. However, the attending intraoperative anesthesiologists and assessors were not blinded to the study group assignment.
3.1. Preoperative Settings
All patients underwent conventional preoperative testing, which included laboratory and imaging procedures such as an ECG and a plain chest X-ray. The patient was advised that the Visual Analog Scale (VAS) was used to assess postoperative pain, with 0 indicating no discomfort and 10 indicating the greatest conceivable suffering.
3.2. Intra-operative and Anesthesia Configurations
Upon arrival in the operating room, the patients received intravenous midazolam 0.05 mg/kg and were monitored using non-invasive blood pressure, pulse oximetry, and electrocardiography. Baseline measures included mean arterial pressure (MAP), heart rate (HR), and oxygen saturation (SpO2). After a thorough airway examination and anticipating a difficult airway, pre-oxygenation was provided with 100% O2 at 10 L/min for 3 minutes via face mask. Ringer's acetate IV fluid was administered to patients according to their body weight. General anesthesia was delivered to each group with 2 mg/kg propofol, 0.5 mg/kg rocuronium bromide, and 2 - 3 mcg/kg fentanyl. Two percent sevoflurane was used to maintain anesthesia, and ventilation parameters that maintained normocapnia (CO2 between 32 and 36 mmHg) were used (volume control mode, tidal volume 6 - 10 mL/kg, RR 12 - 14 breaths/min, peak respiratory pressure < 40 mmHg). Both groups A and B received both blocks by the most experienced one in the team after induction of anesthesia, and any block failure was excluded from the start.
3.2.1. Group A (Serratus Anterior Plane Block)
All of the patients were placed laterally to accomplish the block. After properly sterilizing the skin with 2% chlorhexidine gluconate, a 10-cm, 22-gauge needle was introduced from caudally to cephalad at the midaxillary line at the level of the fourth rib at an angle of 45 degrees, aiming for the location between the two muscles, serratus and latissimus dorsi. A unilateral SAPB block was carried out on the ipsilateral side. Thirty milliliters of 0.25% bupivacaine were administered after two milliliters of saline were injected to ensure that the needle tip was in the correct plane.
3.2.2. Group B (Costotransverse Block)
Every patient was positioned laterally to conduct the block. A 10-cm, 22-gauge needle was pushed lateral to the spinous process of the fourth thoracic vertebra from the caudally cephalad location after the skin had been sufficiently sterilized with 2% chlorhexidine gluconate. On the ipsilateral side of the surgery, a unilateral CTB block was carried out. A needle was moved parallel to the superior costotransverse ligament (SCTL), ending just short of the fourth rib's cranial portion. After injecting 2 mL of saline to confirm the needle tip was in the appropriate plane, 30 mL of 0.25% bupivacaine was delivered, followed by occasional aspiration to ensure the needle was clear of blood or air.
3.2.3. Group C (Patient-Controlled Analgesia)
Following a full recovery, the patients were moved to the PACU. Following a 5 mg nalbuphine bolus dosage, patients received a PCA pump that delivered 20 mg nalbuphine in 100 mL of 0.9% normal saline at a 5 mL/h baseline infusion rate. This was followed by a 0.5 mL self-administered bolus and a 15-minute lockout period.
3.3. Postoperative Settings
Intravenous 1 g paracetamol every 6 hours and IV ketorolac 30 mg every 12 hours were used to provide basic analgesia for all of the patients. Following the patient's release from the operating room, the postoperative pain was evaluated using the verbal approach for pain assessment. The pain after surgery was assessed using a VAS. If the VAS is greater than 5 after surgery, an IV of 5 mg nalbuphine diluted in 5 mL of saline will be administered as needed.
Primary and secondary outcomes: The goal of this study was to investigate the effectiveness of CTB as a novel and secure approach in comparison to SAPB and the PCA group. Both at rest and during arm abduction, the VAS score was recorded at 0, 6, 12, and 24 hours. The study's secondary goal was to ascertain if preoperative regional anesthesia could lower the incidence of PMPS six months later. One of the researchers, who was blind to the groups, conducted a telephone interview with the patients six months later. The interview involved asking comprehensive questions regarding the symptoms of PMPS.
3.4. Statistical Methods
The collected data were coded, tabulated, and statistically analyzed using IBM statistical package for social sciences (SPSS) software version 28.0, IBM Corp., Chicago, USA, 2021. Quantitative data were tested for normality using the Shapiro-Wilk test, then described as mean ± standard deviation (SD) as well as minimum and maximum of the range, and then compared using the ANOVA test. Qualitative data are described as numbers and percentages and then compared using the chi-square test. The Bonferroni test was used for post hoc comparisons. The level of significance was taken at a P-value ≤ 0.050; otherwise, it was considered non-significant.
4. Results
Figure 1 represents 107 patients who were initially screened for eligibility. Ninety patients met the inclusion criteria and were randomly assigned to receive SAPB, CTB, or PCA. All patients were followed up successfully, with no patients lost during follow-up.
4.1. Demographic Data
Table 1 revealed that the groups under study did not differ significantly in age, weight, BMI, ASA grade, or length of operation.
| Variables | SAPB Group (Total = 30) | CTB Group (Total = 30) | PCA Group (Total = 30) | P-Value |
|---|---|---|---|---|
| Age (y) | 0.290 a | |||
| Mean ± SD | 39.6 ± 11.9 | 44.0 ± 13.4 | 44.2 ± 12.5 | |
| Range | 19.0 - 60.0 | 23.0 - 59.0 | 22.0 - 60.0 | |
| Weight (kg) | 0.241 a | |||
| Mean ± SD | 80.0 ± 10.2 | 83.7 ± 8.8 | 83.0 ± 8.0 | |
| Range | 63.0 - 100.0 | 68.0 - 99.0 | 69.0 - 99.0 | |
| BMI (kg/m2) | 0.397 a | |||
| Mean ± SD | 28.3 ± 3.5 | 29.2 ± 3.0 | 29.4 ± 3.0 | |
| Range | 20.6 - 34.3 | 22.6 - 33.5 | 24.1 - 34.9 | |
| ASA (n %) | 0.669 b | |||
| I | 17 (56.7) | 17 (56.7) | 14 (46.7) | |
| II | 13 (43.3) | 13 (43.3) | 16 (53.3) | |
| Operation duration (min) | 0.351 a | |||
| Mean ± SD | 128.9 ± 13.1 | 133.6 ± 12.1 | 132.0 ± 12.9 | |
| Range | 98.0 - 150.0 | 100.0 - 150.0 | 110.0 - 160.0 |
Abbreviations: SAPB, serratus anterior plane block; CTB, costotransverse block; PCA, patient-controlled analgesia; BMI, Body Mass Index; ASA, American Association of Anthologists.
a ANOVA test.
b Chi-square test.
4.2. Pain Score (Visual Analog Scale-10) at Rest
Figure 2 revealed that the CTB group had the lowest resting pain score (VAS-10) at follow-up time points, followed by the SAPB group, while the PCA group had the highest. All research groups showed non-significant changes at hours 0 and 6; however, the PCA group showed significant differences at hours 12 and 24, whereas the CTB and SAPB groups did not show any statistical differences.
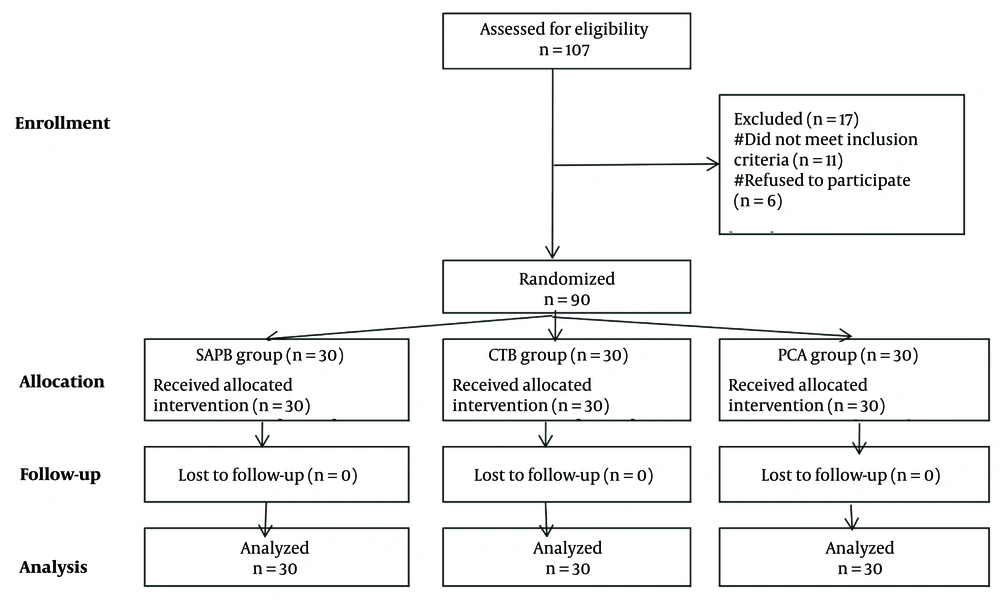
4.3. Pain Score (Visual Analog Scale-10) at Arm Abduction
Figure 3 revealed that the CTB group had the lowest pain score (VAS-10) at arm abduction at follow-up time points, followed by the SAPB group, while the PCA group had the highest. All research groups showed non-significant changes at hours 0 and 6; however, the PCA group showed significant differences at hours 12 and 24, whereas the CTB and SAPB groups did not show any statistical differences.
4.4. Chronic Pain After 6 Months
Table 2 showed that after six months, chronic pain was most common in the PCA group and least common in the CTB group, followed by the SAPB group. The PCA group showed a statistical difference from the CTB group, but the SAPB group did not.
| Status | SAPB Group (Total = 30) | CTB Group (Total = 30) | PCA Group (Total = 30) | P-Value |
|---|---|---|---|---|
| Positive | 5 (16.7) A | 4 (13.3) A | 14 (46.7) B | 0.005 c |
| Negative | 25 (83.3) | 26 (86.7) | 16 (53.3) |
Abbreviations: SAPB, serratus anterior plane block; CTB, costotransverse block; PCA, patient-controlled analgesia.
a Values are expressed as No.(%).
b Capital letters indicate homogenous groups based on post hoc Bonferroni test.
c Significant at p < 0.05.
5. Discussion
Insufficient pain management after MRM surgeries increases the incidence of lung infection and atelectasis and may lead to persistent PMPS. The TPVB was previously considered the gold standard analgesia for chest wall surgeries, with considerable complications like intraspinal hematoma, spinal injuries, and sympathetic block (7). The innervation of the chest wall is quite complex. The purpose of anterolateral chest wall blocks, such as SAPB and PECS blocks, is to anesthetize peripheral nerves, including the long thoracic nerve, the thoracodorsal nerve, and the lateral and medial pectoral nerves. However, they miss the medial breast and axilla (11).
In this randomized clinical research, we wanted to compare the efficacy of CTB, a new modified paravertebral plane block, to SAPB and PCA in terms of immediate and chronic pain relief after MRM procedures. Our results demonstrated that CTB provides relatively better analgesia in both acute and chronic pain following MRM, with reduced opioid intake 24 hours after surgery and fewer adverse effects. At the same time, PCA alone is associated with higher opioid consumption and inferior pain control. The superior analgesic efficacy of CTB can be attributed to its anatomical precision in targeting the dorsal rami of thoracic spinal nerves (T2 - T9) within the CTF. The CTB achieves somatic blockade of the lateral and anterior cutaneous branches (covering breast, axilla, and pectoral regions), visceral modulation via rami communicants, and preemptive analgesia by blocking afferent pain transmission before surgical trauma (6).
While SAPB is technically simpler and avoids pleural puncture, its reliance on lateral intercostal nerve branches (T2 - T9) results in inconsistent coverage of the medial breast and axilla, with higher doses of opioids post-operatively and variable efficacy (12). Inter-transverse process blocks were introduced a few years ago as a substitute for TPVB. The following blocks were described: Mid-point transverse process (MTP) block, multiple injection CTB (MICB), costotransverse foramen block (CTFB), and CTB. They all function by spreading local anesthetics through the costotransverse ligament into the paravertebral region (4).
According to a cadaveric study by Nielsen et al., the dye spread was compared in the erector spinae plane block (ESPB) and MICB using methylene blue. In MICB, 100% of the dye was found in the thoracic paravertebral space (TPVS), compared to 60% in ESPB. The MICB stained the ventral rami, dorsal rami, and the sympathetic trunk (13).
Oh et al. compared CTB and TPVB. The analgesic effect of CTB was non-inferior to that of TPVB 24 hours post-operatively. The difference between the mean 24-hour areas under the curve (AUCs) of the Numeric Rating Scale (NRS) in the CTB (34.25 ± 16.30, n = 24) and TPVB (39.52 ± 17.13, n = 23) groups was -5.27 [95% confidence interval (CI), -15.09 to 4.55], with the upper limit of 95% CI being far below the predefined noninferiority margin of 24. Furthermore, CTB may provide potential safety benefits by keeping the needle tip away from the pleura and vascular structures (14).
Seventy individuals who underwent breast cancer procedures were divided into two groups: The CTB group and the control group, as reported by Aygun et al. At T4, patients received a single injection of CTB. The average time to the first analgesia requirement was 6.34 ± 3.41 hours in the CTB group, compared to 3.34 ± 1.85 hours in the control group (P < 0.001) (15).
Arora et al. compared SAPB and TPVB in a randomized experiment that was conducted on forty patients following breast cancer surgery. Postoperative pain scores were significantly lower in the SAPB group compared with the TPVB group (P < 0.05). The incidence of PONV was also less in the SAPB group (P = 0.028) (16).
In contrast, Ayyamperumal compared SAPB and TPVB in a study of forty females who underwent MRM surgery. The mean duration of analgesia for the SAPB group was 224.2 ± 78.3 minutes and for the Paravertebral group was 336 ± 147.9 minutes (P < 0.001) (17).
Fifty percent of women undergoing MRM develop PMPS. The exact mechanism of PMPS remains unknown. It may be caused by a malfunction of nociception receptors, decreased peripheral and central sensitization, and the discharge of inflammatory substances. According to the literature, there is an association between the severity of post-operative pain and the incidence of PMPS (8).
Berger et al. researched 124 female patients who had TPVB before a full mastectomy in a retrospective study. The statistical analysis demonstrated that severe acute postoperative pain was associated with a higher incidence of long-term chronic pain, particularly at 1 month after the operation (P = 0.003) and at 6 months after the operation (P = 0.018) (18).
5.1. Clinical Implications
We recommend CTB as a preferred regional technique for major breast surgeries as it has wide dermatomal coverage and better reduction in both acute and chronic pain. The SAPB is better reserved for partial mastectomies without axillary clearance.
5.2. Sample Size
We acknowledge that our sample size of 30 patients per group may limit the generalizability of our findings; however, this was determined based on power calculations and feasibility constraints, and future studies with larger cohorts could further validate these results.
5.3. Conclusions
USG single-injection CTB at the level of T4 was not inferior to SAPB in controlling acute and PMPS in patients undergoing MRM surgeries. Both techniques also decrease postoperative opioid consumption.
5.4. Limitations
While our randomized comparison of ultrasound-guided SAPB versus CTB after MRM provides clinically relevant data, several limitations should be acknowledged:
1. Technical variability: Despite all blocks being performed by the most experienced anesthesiologist using standardized ultrasound protocols, subtle local anesthetic spread could influence outcomes.
2. Single-center design.
3. The relative lack of blinding in the PCA group.
5.5. Future Directions
Consider conducting large multi-center trials, adding adjuvants such as dexmedetomidine, and evaluate the combination of CTB and SAPB.
![Pain score [Visual Analog Scale (VAS)-10] at rest between the studied groups Pain score [Visual Analog Scale (VAS)-10] at rest between the studied groups](https://services.brieflands.com/cdn/serve/3170f/de0b3e2d761cc7eb428f0c75b209e60567a2bba8/jcma-10-3-161248-i002-preview.webp)
![Pain score [Visual Analog Scale (VAS)-10] at arm abduction Pain score [Visual Analog Scale (VAS)-10] at arm abduction](https://services.brieflands.com/cdn/serve/3170f/2b4dcdf406cf7666e92aefd7d31663dcd310d98c/jcma-10-3-161248-i003-preview.webp)