1. Background
Postoperative nausea and vomiting (PONV) are among the most common complications following general anesthesia and surgery, particularly in high-risk patients, with reported incidence rates ranging from 53% to 70% (1, 2). The prevalence of nausea and vomiting varies from 27% to 92% after various surgical procedures (3-6). The PONV can result in increased morbidity, prolonged recovery, and higher healthcare costs, as well as serious complications such as dehydration, electrolyte imbalances, and wound-related issues (7, 8). The chemoreceptor trigger zone (CTZ) in the medulla oblongata plays a critical role in initiating the gag reflex, contributing to PONV (9).
Effective PONV management requires consideration of multiple factors, including surgical type, duration, and anesthetic techniques (10). Key risk factors include age < 50 years, female sex, non-smoking status, history of PONV or motion sickness (MS), and postoperative opioid use (11, 12). Current guidelines recommend prophylactic antiemetic treatment for low-to-moderate-risk patients, whereas combination therapy is preferred for high-risk individuals (13). Among the available pharmacological options, haloperidol (a butyrophenone derivative) and ondansetron (a 5-HT3 receptor antagonist) are widely used due to their distinct mechanisms of action (14).
Ondansetron is a highly selective serotonin 5-HT3 receptor antagonist with dual mechanisms of action. It acts peripherally by blocking 5-HT3 receptors in the gastrointestinal tract, thereby preventing vagal afferent nerve activation, while its central effects occur through action in the brainstem’s postrema area. Emerging research indicates that ondansetron possesses significant anti-inflammatory properties, mediated through inhibition of neutrophil extracellular trap (NET) formation via modulation of the TLR8, MAPK14, and NF-κB pathways. Furthermore, the drug mitigates inflammatory damage in critical conditions by downregulating key NET-associated proteins, including neutrophil elastase (NE) and myeloperoxidase (MPO) (15-18).
Haloperidol is a potent dopamine D2 receptor antagonist that exerts its effects through multiple pathways. Historically, haloperidol, though less extensively studied than ondansetron, has shown promise in PONV prophylaxis due to its D2 receptor antagonism, particularly in high-risk surgical patients. By blocking D2 receptors in both the mesolimbic and mesocortical brain regions, it produces antipsychotic effects while simultaneously inhibiting activity in the CTZ located in the medulla. The drug’s antiemetic properties primarily result from dopamine receptor blockade in the area postrema, a critical region for initiating the vomiting reflex. Additionally, haloperidol demonstrates antagonism at serotonin 5-HT2 receptors, which may contribute to its anti-inflammatory and immunomodulatory effects (19, 20).
Haloperidol demonstrates several potential advantages over ondansetron in specific clinical scenarios, supported by evidence. Firstly, haloperidol is significantly more cost-effective than ondansetron, making it a highly advantageous option in resource-limited healthcare settings or where cost containment is a priority (21). Secondly, for refractory chemotherapy-induced nausea and vomiting (CINV) or PONV that does not respond adequately to first-line 5-HT3 antagonists like ondansetron, haloperidol has proven effective as a rescue or adjunctive agent, particularly in breakthrough and refractory cases (22). Thirdly, in palliative care settings for managing terminal nausea, especially in advanced cancer, haloperidol is frequently recommended as a first-line agent and has shown efficacy comparable or potentially superior to ondansetron for nausea refractory to other treatments or of multifactorial origin (23). Fourthly, for severe hyperemesis gravidarum (HG) unresponsive to conventional antiemetics like antihistamines or ondansetron, haloperidol has demonstrated clinical efficacy in reducing intractable vomiting, offering a valuable alternative (24).
Pharmacologically, a key advantage stems from haloperidol’s mechanism: While ondansetron acts solely as a 5-HT3 receptor antagonist, haloperidol is a potent dopamine D2 receptor antagonist acting primarily in the CTZ. This allows haloperidol to target a broader range of emetogenic pathways, particularly those driven by dopamine, which are less effectively blocked by ondansetron alone (25).
The PONV poses a significant challenge in mastectomy patients, where uncontrolled symptoms can compromise recovery and patient satisfaction (26). This is due to hormonal factors, high opioid requirements, and surgery-specific characteristics. Premenopausal patients experience abrupt estrogen and progesterone fluctuations after mastectomy; estrogen enhances serotonin receptor sensitivity in the CTZ and gut, while progesterone withdrawal disrupts GABAergic pathways that suppress nausea. Additionally, mastectomy involves extensive tissue dissection and nerve injury, necessitating high opioid doses (30 - 50% higher than general surgery), which activate μ-opioid receptors and the vestibular nucleus (13, 27). Surgery-specific risks include prolonged duration (> 2 hours), vagal nerve stimulation from chest wall manipulation, and psychological stress, collectively contributing to a PONV incidence of 40 - 80% (4).
Transgender individuals receiving gender-affirming hormone therapy may exhibit altered susceptibility to PONV, as estrogen and testosterone modulate neurotransmitter sensitivity in emetogenic pathways, including serotonin and dopamine systems. Therefore, reducing PONV in these individuals is very crucial.
2. Objectives
This double-blind clinical trial compares the prophylactic antiemetic efficacy of ondansetron versus haloperidol in transgender patients, aiming to optimize PONV management and enhance postoperative outcomes.
3. Methods
3.1. Study Design
This was a double-blind, randomized clinical trial conducted at Hazrat Fatemeh Hospital, involving transsexual patients undergoing elective bilateral mastectomy.
3.2. Sample Size Calculation
The present study included a total of 50 patients (25 in each group) undergoing elective bilateral mastectomy. The sample size was calculated based on the following equation:
Where P1 = 0.50 (expected PONV incidence in control) (26, 28), P2 = 0.14 (d: Thirty-six percent reduction in PONV incidence by expert opinion), Z1-α/2 = 1.96 (α = 0.05), and Z1-β = 0.84 (β = 0.20), this calculation results in (n = 22) for each group, which was inflated to 25 by considering a 10% attrition rate in each group.
3.3. Primary Outcome
The expected incidence of PONV in mastectomy patients without prophylaxis is approximately 40 - 60%. Assuming a 30% absolute reduction in PONV incidence (from 50% to 20%) would be clinically significant. Based on a two-sided α = 0.05 and 80% power (β = 0.20), a minimum of 22 patients per group was required to detect this difference. To account for potential dropouts or protocol deviations, the sample size was increased to 25 patients per group (total n = 50). Type of analysis: Comparison of proportions (chi-square/Fisher’s exact test). Software used: G*Power 3.1 or similar statistical tools for sample size estimation. Feasibility within the study timeline (single-center recruitment). Alignment with similar PONV trials comparing antiemetics. This sample size provided adequate power to detect clinically meaningful differences while maintaining methodological rigor in a double-blind randomized design.
3.4. Randomization and Blinding
Patients were randomly allocated to two groups (A and B) using a computer-generated randomization sequence with block randomization (block size of 4) to ensure balanced group distribution. The randomization list was maintained by an independent statistician not involved in patient care. Sequentially numbered, opaque, sealed envelopes containing group assignments were prepared and opened by the anesthesia nurse just prior to drug administration. Both patients and outcome assessors were blinded to group assignments throughout the study period. The intervention drugs (haloperidol 2 mg IV or ondansetron 4 mg IV) were prepared in identical 1cc syringes by the hospital pharmacy to maintain blinding.
3.5. Selection of the Transgender Population
The selection of this specific population was based on the hypothesis that haloperidol may exhibit enhanced antiemetic effects due to the unique psychological and neurochemical characteristics of transgender individuals. Limited studies have shown that the dopaminergic system is more activated in response to psychosocial stressors associated with gender identity, and since haloperidol is a dopamine D2 receptor antagonist, it was expected to be more effective in this population. Additionally, hormonal changes resulting from the use of sex hormones during the process of gender transition may affect drug metabolism or sensitivity to nausea. Case reports also support the stronger antiemetic effects of haloperidol in populations with psychiatric disorders, such as schizophrenia, who experience similar psychological stresses.
3.6. Standardized Anesthesia Protocol
All patients received:
- Premedication: Midazolam 0.03 - 0.05 mg/kg IV
- Induction: Fentanyl 3 μg/kg + propofol 2 mg/kg + atracurium 0.5 - 0.7 mg/kg
- Maintenance: Propofol 100 μg/kg/min infusion
- Reversal: Neostigmine 0.5 mg/kg + atropine 0.2 mg/kg
- Intraoperative fluids: 5 - 10 mL/kg/h normal saline
- Postoperative analgesia included a standardized morphine dose of 0.1 mg/kg IV, ensuring consistency across patients.
3.7. Outcome Measurement (Detailed Visual Analog Scale Assessment)
The PONV was assessed using the tools below.
3.7.1. Visual Analog Scale
A 10 cm unmarked line where 0 = "no nausea" and 10 = "worst imaginable nausea". Patients marked their current nausea level, measured to the nearest mm by investigators.
3.7.2. Verbal Rating Scale
- Zero: No nausea
- One - three: Mild nausea
- Four - seven: Moderate nausea
- Eight - ten: Severe nausea
3.7.3. Episode Documentation
- Retching: ≥ 1 involuntary attempt to vomit without gastric content expulsion
- Vomiting: ≥ 1 episode of gastric content expulsion
- Rescue antiemetic given for:
- Visual Analog Scale (VAS) ≥ 5 odds ratio (OR)
- Any vomiting episode OR
- Patient request
The assessment timeline for different outcomes is presented in Table 1.
| Time Point | Assessments Performed |
|---|---|
| T0 (PACU arrival) | VAS, VRS, hemodynamics |
| T30, T60, T120 (min) | VAS, vomiting episodes |
| T360, T1440 (min) | VAS, rescue medication use |
| 24 h post-op | Patient satisfaction (5-point Likert scale) |
Abbreviation: VAS, Visual Analog Scale.
3.7.4. Rescue Protocol
Patients received metoclopramide 5 - 10 mg IV for: (1) The VAS ≥ 5 persisting > 15 minutes OR; and (2) any vomiting episode. All assessments were performed by trained research nurses blinded to group allocation.
3.8. Data Analysis
Data analysis included descriptive statistics for central tendency and dispersion indices based on variable type, with mean and standard deviation reported for quantitative variables and frequency and percentage for qualitative variables. Various variables were displayed using tables and graphs. To compare quantitative variables, t-tests and ANOVA were employed. Comparisons between qualitative variables were conducted using chi-Square or Fisher’s exact test. A significance level of 5% was considered, and the data from this study were analyzed using SPSS version 26 software.
4. Results
This study compared the effects of haloperidol and ondansetron in preventing PONV in 50 patients (25 in each group; Figure 1). The mean age of patients was similar between the two groups (haloperidol: 26.68 ± 4.65 years; ondansetron: 27.24 ± 4.15 years; P = 0.656), indicating a balanced age distribution.
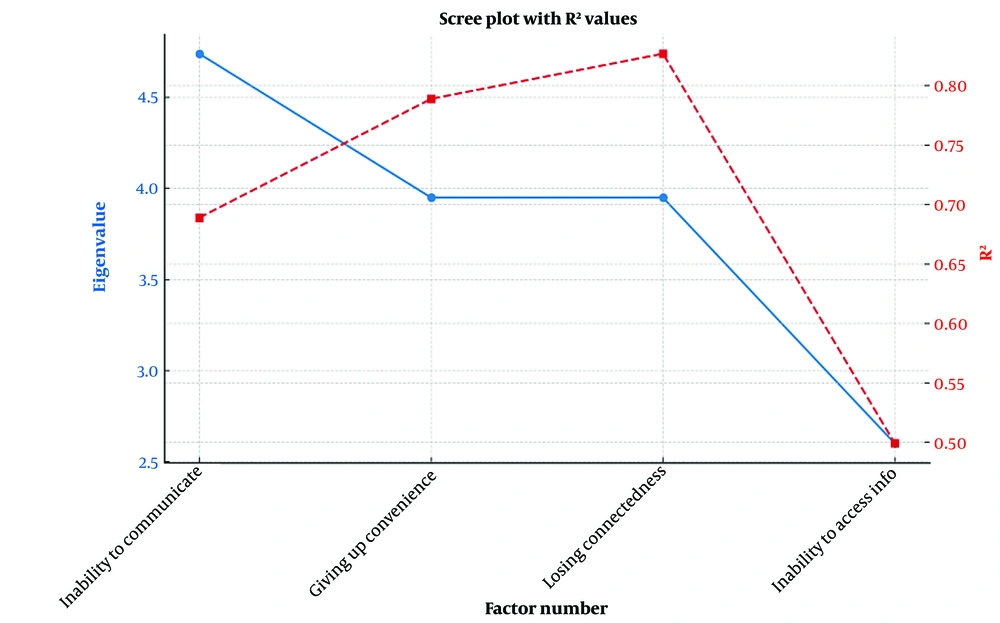
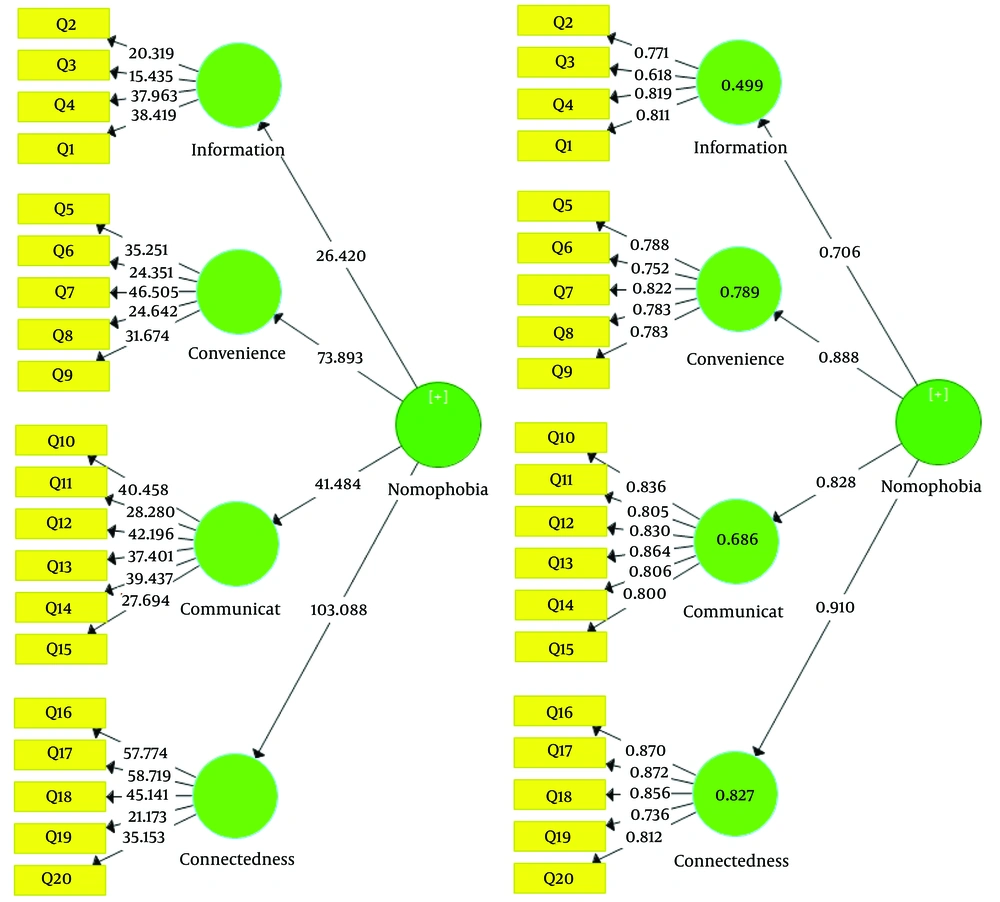
When evaluating PONV at different time intervals, at 0.5 hours postoperatively, 20% of patients in the haloperidol group and 12% in the ondansetron group exhibited PONV symptoms, though this difference was not statistically significant (OR = 1.83, 95% CI: 0.38 - 8.67; P = 0.70). At 1 hour, the incidence of PONV was higher in the ondansetron group (56% vs. 36%), but this difference also lacked statistical significance (OR = 1.83, P = 0.156). However, at 2 hours, the difference approached borderline significance, with 44% of patients in the ondansetron group experiencing PONV compared to 20% in the haloperidol group (OR = 3.1, 95% CI: 0.8 - 11.06; P = 0.06), suggesting a potential trend toward greater efficacy with haloperidol during this period. In other words, the trends favoring haloperidol at this time may signal time-dependent efficacy.
By 6 hours, PONV rates decreased in both groups, with no significant difference observed (haloperidol: Twelve percent; ondansetron: Eight percent; OR = 0.63, P = 0.637). Finally, at 24 hours, only one patient in the haloperidol group (4%) reported PONV, whereas no cases were recorded in the ondansetron group (OR = 0.49, P = 0.312) (Table 2).
| Characteristics | Haloperidol (N = 25) | Ondansetron (N = 25) | Types of Statistical Tests | OR | P-Value |
|---|---|---|---|---|---|
| Age (y) | 26.68 ± 4.65 | 27.24 ± 4.15 | 0.449 b | - | 0.656 |
| PONV (0.5 h) | 0.59 c | 1.83 (0.38 - 8.67) | 0.70 | ||
| No | 5 (20.0) | 3 (12.0) | |||
| Yes | 20 (80.0) | 22 (88.0) | |||
| PONV (1 h) | 2.01 c | 1.83 (0.38 - 8.67) | 0.156 | ||
| No | 16 (64.0) | 11 (44.0) | |||
| Yes | 9 (36.0) | 14 (56.0) | |||
| PONV (2 h) | 3.30 c | 3.1 (0.8 - 11.06) | 0.06 | ||
| No | 20 (80.0) | 14 (56.0) | |||
| Yes | 5 (20.0) | 11 (44.0) | |||
| PONV (6 h) | 0.22 c | 0.63 (0.97 - 4.18) | 0.637 | ||
| No | 22 (88.0) | 23 (92.0) | |||
| Yes | 3 (12.0) | 2 (8.0) | |||
| PONV (24 h) | 1.02 c | 0.49 (0.36 - 0.652) | 0.312 | ||
| No | 24 (96.0) | 25 (100) | |||
| Yes | 1 (4.0) | 0 (0.0) |
Abbreviations: OR, odds ratio; PONV, postoperative nausea and vomiting.
a Values are expressed as mean ± SD or No. (%).
b Independent t-test.
c Chi-square.
In summary, although ondansetron showed a tendency toward better efficacy at certain time points (particularly at 2 hours postoperatively), the observed differences were not statistically significant. Nevertheless, these results may indicate a trend that could reach significance in studies with larger sample sizes. In the long term (24 hours postoperatively), both drugs demonstrated comparable effectiveness in controlling PONV (Figure 2).
The PONV outcomes showed similar efficacy between the haloperidol and ondansetron groups, though numerical differences emerged in early recovery periods. At 0.5 hours post-surgery, 20% of haloperidol recipients reported complete symptom relief (VAS = 0) versus 12% with ondansetron, while 44% versus 32% reported mild symptoms (VAS = 1), respectively (χ2 = 4.418, P = 0.352). This trend continued at 1 hour, where 68% of haloperidol patients were symptom-free compared to 44% with ondansetron, though statistical significance was not reached (P = 0.205). By 2 hours, 80% of haloperidol-treated patients achieved VAS = 0 versus 56% with ondansetron, with 20% versus 40% reporting mild symptoms (P = 0.155). Notably, ondansetron had a 2% rate of moderate symptoms (VAS = 2) at this time point, which haloperidol completely prevented.
Both medications demonstrated strong and comparable effectiveness beyond 6 hours postoperatively. At the 6-hour assessment, 88% of haloperidol and 92% of ondansetron recipients reported complete symptom resolution (P = 0.637). By 24 hours, near-complete efficacy was observed in both groups: Ninety-six percent of haloperidol and 100% of ondansetron patients were symptom-free (P = 0.312), with only 4% of haloperidol recipients reporting mild residual symptoms. While haloperidol showed numerically superior early symptom control (0.5 - 2 hours), chi-square analysis confirmed no statistically significant differences between groups at any time point (all P > 0.05) (Table 3).
| Time (h); Score | Haloperidol (N = 25) | Ondansetron (N = 25) | Total | Chi-Square | P-Value |
|---|---|---|---|---|---|
| 0.5 | 4.41 | 0.35 | |||
| 0 | 5 (20.0) | 3 (12.0) | 8 (16) | ||
| 1 | 11 (44.0) | 8 (32.0) | 19 (38.0) | ||
| 2 | 5 (20.0) | 4 (16.0) | 9 (18.0) | ||
| 3 | 4 (16.0) | 8 (32.0) | 12 (24.0) | ||
| 4 | 0 (80.0) | 2 (8.0) | 2 (4.0) | ||
| 1 | 3.17 | 0.20 | |||
| 0 | 17 (68.0) | 11 (44.0) | 28 (56.0) | ||
| 1 | 6 (24.0) | 9 (36.0) | 15 (30.0) | ||
| 2 | 2 (8.0) | 5 (20.0) | 7 (14.0) | ||
| 2 | 3.72 | 0.15 | |||
| 0 | 20 (80) | 14 (56.0) | 34 (68.0) | ||
| 1 | 5 (20.0) | 10 (40.0) | 15 (30.0) | ||
| 2 | 0 (0.0) | 1 (4.0) | 1 (2.0) | ||
| 6 | 0.22 | 0.63 | |||
| 0 | 22 (80.0) | 23 (92.0) | 45 (90.0) | ||
| 1 | 3 (12.0) | 2 (8.0) | 5 (10.0) | ||
| 24 | 1.02 | 0.312 | |||
| 0 | 24 (96.0) | 25 (100.0) | 49 (98.0) | ||
| 1 | 1 (4.0) | 0 (0.0) | 1 (2.0) |
a Values are expressed as No. (%).
Multiple complications, such as QT prolongation/extrapyramidal symptoms and headache, were monitored, and no adverse effects, specifically no cases of QT prolongation or extrapyramidal symptoms, occurred in either group.
5. Discussion
The study assessed PONV in patients receiving either haloperidol or ondansetron, finding no significant differences in incidence rates at various time points post-surgery. Specifically, the rates of nausea and vomiting were 80% vs. 88% at half an hour, 36% vs. 56% at one hour, 20% vs. 44% at two hours, 12% vs. 8% at six hours, and 4% vs. 0% at 24 hours for haloperidol and ondansetron, respectively.
The PONV is a common complication after surgery and anesthesia, influenced by various patient-related factors (gender, age, BMI, history of MS, etc.), preoperative factors (diet, medications, anxiety), intraoperative factors (anesthetic technique), and postoperative factors (pain management, early ambulation) (29). Opioid use increases the risk of PONV (28, 30, 31). Despite advancements in understanding and treating PONV, its occurrence remains high, especially in laparoscopic and gynecological surgeries (32). Complications from PONV can include pulmonary aspiration, dehydration, and psychological effects on patients and families. High-risk groups include younger patients, women, non-smokers, and those with comorbidities undergoing gynecological procedures (33). The implications of PONV can lead to increased healthcare costs and delays in recovery and discharge (32).
In the present study, the incidence of nausea and vomiting half an hour after surgery was 80% in the haloperidol group and 88% in the ondansetron group, with no statistically significant difference between the two groups. These findings align with similar studies, such as that by Apfel et al., which demonstrated that both ondansetron and haloperidol are effective in reducing the incidence of PONV, with no significant differences between them (28). They found that the female gender, history of MS or PONV, nonsmoking, and the use of postoperative opioids are the main risk factors for PONV.
Numerous studies have indicated that there is no significant difference among various medications in controlling PONV during the postoperative period (34, 35), which corroborates the findings of the current study. Lee et al., in a randomized, double-blinded trial of 90 non-smoking female patients, showed that PONV incidence was 28% with haloperidol vs. 26% with ondansetron (no significant difference). Both drugs significantly reduced PONV compared to patients’ predicted risk. Safety profiles were comparable, with no differences in postoperative pain scores, sedation levels, recovery times, or QTc interval prolongation (36).
According to the VAS scores, the severity of nausea and vomiting at different time points did not exhibit statistically significant differences. These results are consistent with the observations made by Kranke et al., who reported that the severity of PONV is not significantly influenced by the type of medication administered (37). The impact of currently available medications appears to be limited, and in some cases, a combination of these drugs may be necessary for effective PONV control. Medications such as droperidol, metoclopramide, and ondansetron are typically administered 55 to 99 minutes before the conclusion of surgery (38).
In the study by Leksowski et al., which involved 195 patients undergoing open abdominal surgery, ondansetron was found to be less effective in preventing nausea compared to droperidol and metoclopramide, despite similar outcomes in terms of vomiting control. This suggests that while ondansetron is widely used, it may not be the best option for all patients, particularly those at higher risk for nausea (39).
Conversely, Milnes et al. demonstrated that prophylactic administration of ondansetron significantly reduced the incidence of nausea and vomiting in patients undergoing plastic surgery. This finding highlights the potential benefits of ondansetron in certain surgical contexts, suggesting that its effectiveness may be influenced by factors such as the type of surgery or patient characteristics (40).
The Ekinci et al.’s trial [n = 5,922 (gynecological surgeries)] demonstrated ondansetron’s superior efficacy over metoclopramide (41), contrasting with our findings of equivalent haloperidol/ondansetron outcomes. This discrepancy may reflect differences in surgical type (gynecologic vs. mastectomy) or sample size. Conversely, Wu et al.’s cholecystectomy study (n = 494) aligned with our results, showing comparable metoclopramide/ondansetron effects despite procedural differences (42). Carlisle’s cesarean study (n = not specified) revealed ondansetron’s advantage over metoclopramide for nausea control (though equivalent for vomiting prevention) (43), highlighting how anesthesia protocols (neuraxial vs. general) may influence outcomes.
Notably, two laparoscopic cholecystectomy studies (36, 44) corroborated our conclusion, finding no significant difference between ondansetron and haloperidol in PONV incidence or recovery metrics. Recent comparative studies further support the equivalent efficacy of different antiemetic regimens for PONV prevention. Wang et al. found no significant difference between dexamethasone-ondansetron and dexamethasone-haloperidol combinations when used with patient-controlled anesthesia (45). Similarly, Kamali et al. demonstrated comparable effectiveness among ondansetron, haloperidol, and dexmedetomidine in laparoscopic hysterectomy patients (46).
These findings collectively reinforce that while multiple pharmacological options exist for PONV prophylaxis — including 5-HT3 antagonists (ondansetron), dopamine antagonists (haloperidol), and α2-agonists (dexmedetomidine) — none has demonstrated clear superiority over others in head-to-head comparisons. The consistent lack of significant efficacy differences between these agents suggests that clinical decisions should consider factors beyond pure antiemetic potency, such as side effect profiles, cost, and patient-specific risk factors. This study had several limitations that should be considered. The relatively small sample size (50 patients) may have reduced the ability to detect small differences between the two drugs. Additionally, conducting the study at a single center may affect the generalizability of the results. Moreover, the study of a transgender population, while clinically relevant, may limit the generalizability of these findings to other groups. Also, the 24-hour follow-up period may be insufficient to identify delayed adverse drug reactions. The selection of a specific transgender patient population may limit the generalizability of the findings to other demographic groups. Finally, the use of fixed drug doses (haloperidol 2 mg and ondansetron 4 mg) did not allow for evaluation of dose-dependent effects. These limitations highlight the need for larger-scale studies with longer follow-up periods to confirm the results and more thoroughly evaluate the safety profiles of these medications.
5.1. Conclusions
In conclusion, there were no statistically significant differences between the haloperidol and ondansetron groups at half an hour, one hour, two hours, six hours, and 24 hours after surgery. These findings suggest that both drugs are equally effective in controlling PONV. Based on these results, it is recommended that physicians consider both haloperidol and ondansetron when selecting the appropriate medication for the prevention of PONV. Both drugs are equally effective, so the choice should depend on patient risk factors, cost, and side effect profile. Finally, it is suggested that a larger multicenter trial with dose-ranging and safety monitoring be conducted.