1. Background
Constipation refers to bowel movements fewer than twice a week. According to the definition, chronic constipation should have two or more of the following symptoms for at least three months: Excessive strain during a bowel movement, stiffness in stool consistency, feeling incomplete excretion after a bowel movement, and defecation less than twice a week (1-3). Various studies have shown the interaction between the function of the urinary system and the intestine. The association between the bladder and intestine is evident through the presence of urinary symptoms in patients with irritable bowel syndrome and the presence of intestinal symptoms in patients with acute cystitis. Gastrointestinal disorders such as constipation can lead to lower urinary tract symptoms, including bladder hyperactivity (4). The embryonic origin of the bladder and rectum is the same, and their autonomic and somatic innervations are similar. Due to the proximity of these two organs, the dysfunction of one of them can affect the other. Therefore, defecation disorders can be associated with urinary tract problems.
Studies in children have shown that constipation is associated with urinary tract problems, including infection, urinary incontinence, vesicoureteral reflux, and urinary tract obstruction. The underlying pathophysiology of these findings has not yet been elucidated (5). A study showed that an increase in rectal diameter is associated with a high frequency of urinary tract infections (6). Another author depicted that the treatment of constipation resulted in significant urinary control (7). Some researchers found that the prevalence of constipation was 8% in children with UTI, and the prevalence of recurrent UTI was 67.8% in children with constipation. A significant relationship was found between recurrent UTI and constipation (8). Previous publications have not indicated any association between constipation duration and the frequency of UTI and its upper and lower types (cystitis and pyelonephritis).
2. Objectives
The purpose of this study was to evaluate the link between constipation duration and urinary tract infection.
3. Methods
This descriptive-analytical study utilized a simple random sampling method. The population consisted of children with chronic constipation aged 1 - 12 years who referred to the Pediatric Gastroenterology Clinic of Besat Hospital of Sanandaj during one year (2018 - 2019). The inclusion criteria included children with chronic constipation aged 1 - 12 years (based on the Rome IV criteria (9)). The exclusion criteria were children with organic constipation and/or previous use of antispasmodics or antibiotics, and patients who had a history of anorectal surgery or anatomical disorders of the urinary tract.
3.1. Intervention
Informed consent was obtained from children or their parents. The questionnaires were filled out by parents. Each questionnaire consisted of demographic information including age, sex, place of residence, duration of chronic constipation, and history or presence of urinary symptoms (including dysuria, frequency, hematuria, abdominal pain, flank pain, and fever). All children were examined for UTI. For this purpose, a sterile urine sample was sent for analysis and culture. Urinary tract infection was considered when there were more than 105 colonies of one type of a pathogen or 104 colonies in symptomatic children with active urine (10). We considered fever as the main criterion for distinguishing upper and lower urinary tract infections (11, 12). Children with UTI were referred to the Nephrology Clinic for treatment. Appropriate treatment for chronic constipation was also prescribed. The study was approved by the Ethics Committee of Kurdistan University of Medical Sciences (Ethical Number: IR.MUK.REC.1397/162).
3.2. Statistic Analysis
Data were analyzed using SPSS V. 22 software and descriptive statistics. After determining the prevalence of constipation and UTI and their 95% confidence intervals, the chi-square and independent t-tests were used to evaluate the study hypotheses. P values of less than 0.05 were considered statistically significant.
4. Results
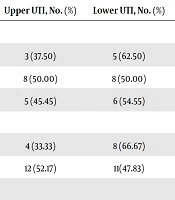
In this study, 220 patients participated. There were 54.55% (n = 120) male patients. Most children were in the age group of 3 - 6 years. Besides, 83% (n = 183) were urbanites. In terms of duration, 45% suffered from constipation for less than a year, 33% for one to two years, and about 22% for more than two years (Table 1). Moreover, 16% (n = 35) had concurrent UTI. Of them, 46% suffered from constipation for less than one year, 26% for one to two years, and 28% for more than two years. There was no significant relationship between the duration of constipation and the frequency of UTI (P value = 0.450) (Table 1). Among children with UTI, the ratio of girls to boys was 2:1 and there was a significant relationship between gender and UTI (P value = 0.010). The highest number of UTI was encountered in the group of 3 - 6 years. There was no significant relationship between age and UTI (P value = 0.528). Among children with UTI, about 46% (n = 16) had upper UTI (pyelonephritis) and 54% (n = 19) had lower UTI (cystitis). There was no significant relationship between the duration of constipation and the type of UTI (P value = 0.911). The details on the type of UTI and duration of chronic constipation are presented in Table 2. The demographics of patients with each type of UTI and duration of chronic constipation are summarized in Table 2. There was no significant relationship between the type of UTI and gender and age (P value = 0.909, P value = 0.476, respectively). The duration of chronic constipation, frequency of UTI, and age distribution are summarized in Tables 1 and 2. The place of residence had no significant relationship with constipation, UTI, and types of UTI (P value = 0.808 and P value = 1.000, respectively) (Tables 1 and 2). The most common symptoms of UTI were frequency (14.55%), dysuria (12.73%), abdominal pain (7.73%), and fever (7.27%). The flank pain, hematuria, nausea, and vomiting were rare. Urinalysis was abnormal in 14.5% of the patients, and urine culture was positive in 8.2%.
| Variable | Chronic Constipation, No. (%) | UTI, No. (%) | P Value |
|---|---|---|---|
| Age group, mo | 0.528 | ||
| 1 - 36 | 43 (19.55) | 8 (18.60) | |
| 37 - 72 | 119 (54.09) | 16 (13.45) | |
| > 72 | 58 (26.35) | 11 (18.97) | |
| Sex | 0.010 | ||
| Male | 120 (54.55) | 12(10.00) | |
| Female | 100 (45.45) | 23 (23.00) | |
| Place of living | 0.808 | ||
| Urban | 183 (83.18) | 30 (16.39) | |
| Rural | 37 (16.82) | 5 (13.51) | |
| Duration of constipation, mo | |||
| 1 - 24 | 99 (45.00) | 16 (16.16) | 0.405 |
| 25 - 48 | 73 (33.18) | 9 (12.33) | 0.528 |
| > 48 | 48 (21.825) | 10 (20.83) |
| Variable | Upper UTI, No. (%) | Lower UTI, No. (%) | P Value |
|---|---|---|---|
| Age group, mo | 0.909 | ||
| 1 - 36 | 3 (37.50) | 5 (62.50) | |
| 37 - 72 | 8 (50.00) | 8 (50.00) | |
| > 72 | 5 (45.45) | 6 (54.55) | |
| Sex | 0.476 | ||
| Male | 4 (33.33) | 8 (66.67) | |
| Female | 12 (52.17) | 11(47.83) | |
| Place of living | 1.000 | ||
| Urban | 14 (46.67) | 16 (53.33) | |
| Rural | 2 (40.00) | 3 (60.00) | |
| Duration of constipation, mo | 0.911 | ||
| 1 - 24 | 8 (50.00) | 8 (50.00) | |
| 25 - 48 | 4 (44.44) | 5 (46.55) | |
| > 48 | 4 (40.00) | 6 (60.00) |
5. Discussion
Constipation is a common gastrointestinal problem in children that can impose huge costs on society. This problem is a major complaint in 3% of referrals to physicians’ clinics and 10% - 25% of referrals to pediatric gastroenterologists. It is, therefore, a major problem for both patients and families (13). Considering the high prevalence of UTI and constipation in children, as well as the complications of UTI on the developing kidney, it is important to investigate the causative and exacerbating factors. On the other hand, constipation is one of the possible contributing factors to the development and recurrence of UTI. However, there are controversial results about the role of bowel dysfunction in urinary disorders such as urinary reflux, UTI, and urinary incontinence. We found that the frequency of constipation was highest in the group of 3 - 6 years (54.09%). Hakimzadeh et al. showed that most cases of constipation were in the group of 2 - 7 years (84.47%) (8). In the Sampaio study, the mean age of the patients was nine years (7 - 11 years) (14). This difference may be related to the difference in the participants’ age in the studies (1 - 12 years vs. 5 - 17 years). The most common age group of constipation patients was between one and five years in Sarvari’s study (15). According to our results, about 16% of children with chronic constipation also had UTI. This rate was reported as 67.8% by Hakimzadeh et al. (8) and 27% by Sampaio et al. (14). These studies suggested a significant association between UTI and constipation. Sampaio demonstrated that children with constipation were about seven times more likely to have inferior UTI, and there was a significant association between the two diseases. Sarvari et al. reported a 13.3% UTI prevalence in children with constipation (15). According to our results, there was no relationship between the frequency of UTI, its types (upper or lower infection), and the duration of constipation (P value = 0.450). Since no previous studies have examined this relationship, we could not compare our findings with others. More than half of the patients in our study were boys, while in other studies, constipation was more common in girls (8, 14, 16). This difference may be due to differences in race and culture. In some areas, boys are more than girls. The majority of patients in our study were from urban areas. The justification for this discrepancy is that urbanites are more likely to see a doctor for treatment than rural people. The most common clinical manifestations of UTI were frequency, dysuria, abdominal pain, and fever. Dehghani et al. also reported that the most common symptoms were dysuria and frequency (16). In the Sarvari et al. study, the most common manifestations of UTI were fever, dysuria, and frequency (15). The results of urinalysis and culture vary among different studies. Dehghani et al. exhibited abnormal urine analysis in 8.3% and positive urine culture in 5.8% of patients (16). In the Sarvari et al. study, the urinary culture was positive in 13.3% (15). We found that urinalysis was abnormal in 14.55%, and urine culture was positive in 8.18%. We noted that lower UTI was more common than upper UTI. This may be due to the anatomical association between the bladder and rectum, so cystitis and lower UTIs were more common in these children. In our study, UTI was more common in girls. Many studies are consistent with our results and showed that UTI was more frequent in girls (8, 15). This can be due to the shortness of urethra in girls and the anatomical abnormalities such as labia majora adhesion. The UTI was mostly found in the age group of 3 - 6 years. Hakimzadeh et al. depicted the highest incidence of UTI in the age group of 2 - 7 years (8).
5.1. Conclusion
Constipation and UTI were more common in the age group of 3 - 6 years. Constipation was more common in boys and UTI in girls. The prevalence of UTI was about 16% in children with constipation, with lower UTI being more common. Most of these children had constipation for less than a year. The duration of constipation had no significant relationship with the prevalence and type of UTI.